18 Plastic and reconstructive surgery
Introduction
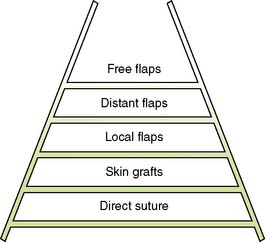
Plastic and reconstructive surgery is concerned with the restitution of form and function after trauma and ablative surgery. The techniques by which this is achieved are applicable to virtually every surgical subspecialty and are not limited to any single anatomical region or system. The ‘reconstructive ladder’ is broad, simple and widely applicable at its base, but narrow, technically demanding and complex at its top (Fig. 18.1). It is important to distinguish plastic and reconstructive surgery from cosmetic, or aesthetic, surgery. In the latter, the techniques of the former are applied to improve appearance but not physical function, although there may be considerable psychological benefit.
Structure and functions of skin
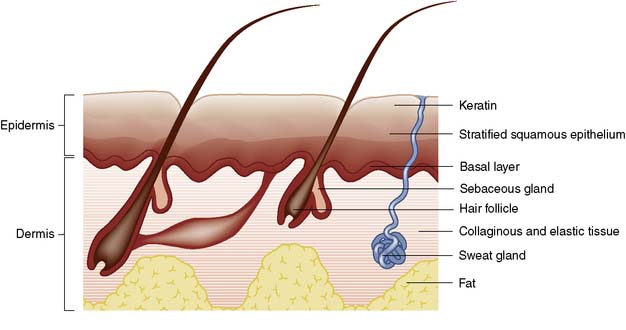
Skin consists of epidermis and dermis. The epidermis is a layer of keratinized, stratified squamous epithelium (Fig. 18.2) that sends three appendages (hair follicles, sweat glands and sebaceous glands) into the underlying dermis. Because of their deep location, the appendages escape destruction in partial-thickness burns and are a source of new cells for reconstitution of the epidermis. The basal germinal layer of the epidermis generates keratin-producing cells (keratinocytes), which become increasingly keratinized and flattened as they migrate to the surface, where they are shed. The basal layer also contains pigment cells (melanocytes) that produce melanin, which is passed to the keratinocytes and protects the basal layer from ultraviolet light.
Wounds
Types of wound
Wounds can be classified according to the mechanism of injury:
• Incised wounds. A sharp instrument causes these; if there is associated tearing of tissues, the wound is said to be lacerated
• Abrasions. These result from friction damage and are characterized by superficial bruising and loss of a varying thickness of skin and underlying tissue. Dirt and foreign bodies are frequently embedded in the tissues and can give rise to traumatic tattooing
• Crush injuries. These are due to severe pressure. Even though the skin may not be breached, there can be massive tissue destruction. Oedema can make wound closure impossible. Increasing pressure within fascial compartments can cause ischaemic necrosis of muscle and other structures (compartment syndrome)
• Degloving injuries. These result from shearing forces that cause parallel tissue planes to move against each other: for example, when a hand is caught between rollers or in moving machinery. Large areas of apparently intact skin may be deprived of their blood supply by rupture of feeding vessels
• Gunshot wounds. These may be low-velocity (e.g. shotguns) or high-velocity (e.g. military rifles). Bullets fired from high-velocity rifles cause massive tissue destruction after skin penetration
• Burns. These are caused not only by heat but also by electricity, irradiation and chemicals.
Principles of wound healing
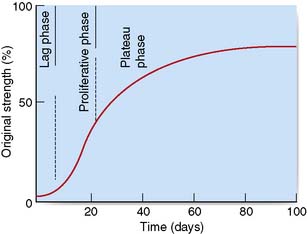
The essential features of healing are common to wounds of almost all soft tissues, and result in the formation of a scar. Soft tissue healing can be subdivided into three phases (Table 18.1) according to the development of tensile strength (Fig. 18.3).
Table 18.1 Phases of wound healing
| Lag phase (2–3 days) |
| Incremental or proliferative phase (approximately 3 weeks) |
| Plateau or maturation phase (approximately 6 months) |
Primary and secondary intention
Wounds may heal by primary intention if the edges are closely approximated: for example, by accurate suturing. Epithelial cover is quickly achieved and healing produces a fine scar (Fig. 18.4). If the wound edges are not apposed, the defect fills with granulation tissue and the restoration of epidermal continuity takes much longer. The advance of epithelial cells across the denuded area may be hindered by infection. This is known as healing by secondary intention and usually results in delayed healing, excessive fibrosis and an ugly scar (Fig. 18.5). If a wound has begun to heal by secondary intention, it may still be possible to speed healing by excising the wound edges and bringing them into apposition, or by covering the defect with a skin graft.
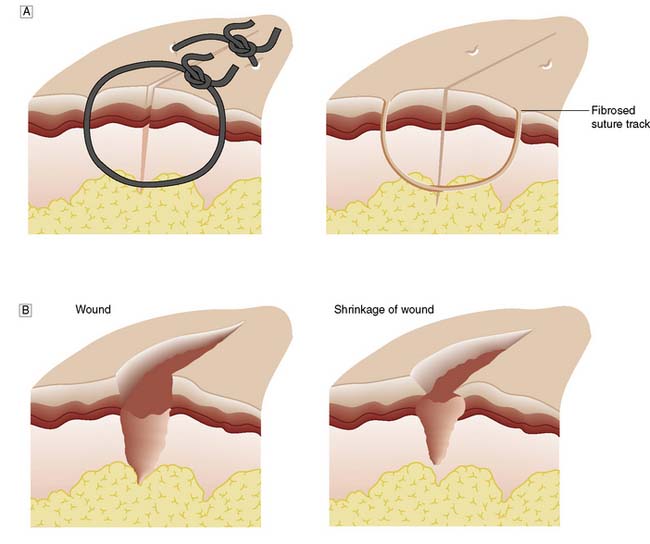
Fig. 18.4 Wound healing.
A Healing by primary intention. B Healing by secondary intention, showing shrinkage of the wound.
Summary Box 18.1 Classification of wound healing
• Healing by first intention is the most efficient method and results when a clean incised surgical wound is meticulously apposed and heals with minimal scarring
• Healing by second intention occurs when wound edges are not apposed and the defect fills with granulation tissue. In the time taken to restore epithelial cover, infection supervenes, fibrosis is excessive and the resulting scar is unsightly
• The term ‘healing by third intention’ describes the situation where a wound healing by second intention (e.g. a neglected traumatic wound or a burn) is treated by excising its margins and then apposing them or covering the area with a skin graft. The final cosmetic result may be better than if the wound had been left to heal by second intention.
Factors influencing wound healing
Wound infection
Classification
• Clean procedures are those in which wound contamination is not expected and should not occur. An incision for a clean elective procedure should not become infected. In clean operations, the wound infection rate should be less than 1%.
Summary Box 18.2 Factors affecting wound healing
Wounds with a good blood supply (e.g. head and neck wounds) heal well
Infection is a major adverse factor and the risk of infection is influenced by:
Intercurrent disease may impair healing. Important factors include:
Surgical technical factors that have a major influence on wound healing include:
• Clean-contaminated procedures are those in which no frank focus of infection is encountered but where a significant risk of infection is nevertheless present, perhaps because of the opening of a viscus, such as the colon. Infection rates in excess of 5% may suggest a breakdown in ward and operating theatre routine.
• Contaminated or ‘dirty’ wounds are those in which gross contamination is inevitable and the risk of wound infection is high; an example is emergency surgery for perforated diverticular disease, or drainage of a subphrenic abscess.
Antibiotic prophylaxis is appropriate for the latter two types of operation.
Involvement of other structures
Summary Box 18.3 Principles of management of contaminated traumatic wounds
• Contaminated wounds should be debrided under general anaesthesia
• The contaminated wound and its margins must be cleansed thoroughly, and grit, soil and foreign bodies/materials removed
• Devitalized tissue is formally excised until bleeding is encountered
• Primary closure is avoided if there has been gross contamination and when treatment has been delayed for more than 6 hours. Inappropriate attempts to achieve primary closure increase the risk of wound infection and expose the patient to the risks of anaerobic infection (tetanus and gas gangrene)
• Wounds left open may be suitable for delayed primary suture after 2–3 days, or for later excision and secondary suture (with or without skin grafting)
• Appropriate protection against tetanus must be afforded and the use of antibiotics should be considered.
involves a limb, the distal circulation must be checked. Where appropriate, X-rays will help to establish whether peritoneal, pericardial or pleural cavities have been entered, and whether there is underlying bony injury.
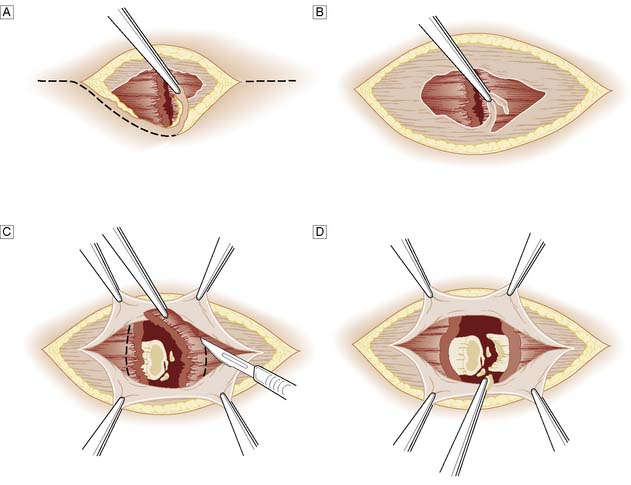
More extensive or severely contaminated wounds usually require inpatient treatment, with exploration and debridement under general anaesthesia. The wound and its margins are cleansed and all obvious foreign material picked out. Devitalized tissue is trimmed back until bleeding occurs. In areas of poor vascularity such as the leg, or if there is severe contamination, crushing or a fracture, the wound margins are formally excised (Fig. 18.6). Bleeding from the wound margin is not a certain indication of its ultimate survival, as impaired venous drainage can lead to progressive necrosis, particularly after a crushing or degloving injury. If there is any doubt, the wound should not be sutured and a ‘second-look’ dressing change should be undertaken under anaesthesia after 48 hours.
Devitalized skin flaps
A common emergency problem is posed by the patient, usually an elderly woman, who falls and raises a triangular flap over the surface of the tibia (pretibial laceration). In some cases, the flap is blue-black in colour and obviously non-viable, but in most cases viability is uncertain. Similar injuries can occur elsewhere in the body. The wound must be cleansed and non-viable tissue excised. No attempt should be made to suture the flap back into place; because of the post-traumatic oedema this would only be possible under tension, and would lead to death of the flap. A small defect can be treated conservatively on an out-patient basis by wound dressing and an elastic supporting bandage providing the arterial circulation is normal; Ch. 21) and the patient is kept ambulant. The wound will normally take several weeks to heal. A larger defect may require a split-skin graft, either immediately or as a delayed primary procedure.
Wounds with skin loss
Flaps
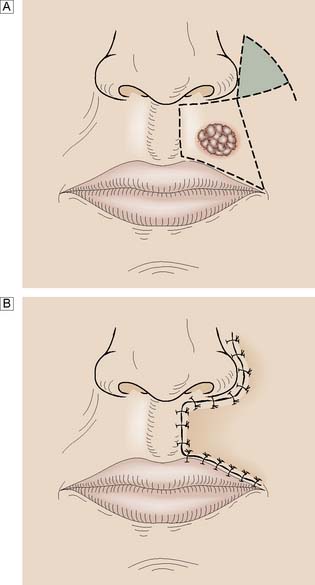
Whereas grafts require a vascular bed to survive, flaps bring their own blood supply to the new site. They can therefore be thicker and stronger than grafts and can be applied to avascular areas such as exposed bone, tendon or joints. They are used in acute trauma only if closure is not possible by direct suture or skin grafting, and are more usually reserved for the reconstruction of surgical defects and for secondary reconstruction after trauma. The simplest flaps use local skin and fat (local flaps), and are often a good alternative to grafting for small defects such as those left after the excision of facial tumours (Fig. 18.7). A flap may have to be brought from a distance (distant flap) and remain attached temporarily to its original blood supply until it has picked up a new one locally (Fig. 18.8). This usually takes 2–3 weeks, after which the pedicle can be divided. Advances in our knowledge of the blood supply to the skin and underlying muscles have led to the development of many large skin, muscle and composite flaps, which have revolutionized plastic and reconstructive surgery. One example is the use of the transverse rectus abdominis musculocutaneous (TRAM) flap for reconstruction of the breast. The ability to join small blood vessels under the operating microscope now allows the surgeon to close defects in a single stage, even when there is no local tissue available, by free tissue transfer (Fig. 18.9). Other tissues, such as bone, cartilage, nerve and tendon, can also be grafted to restore function and correct deformity after tissue damage or loss.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree