Overview
Physical agents are well characterized and relatively easily measured and knowledge of exposures is important in managing the workplace
Appropriate control of exposure is essential in preventing harm arising from physical agents
Administrative controls and the use of personal protective equipment may be necessary in managing workplace exposures
Administrative controls may include screening of workers to identify any thought to be at particular risk from the exposure
Health surveillance may be used to monitor the effectiveness of controls, and to identify at an early stage any workers who may have suffered harm
Physical Agents
The effects of physical agents have been well studied, and for many of these, exposure criteria are now established at an international level. Fatalities are only likely to occur where established safety procedures are broken
Physical agents impart energy to the body by physical means (for example the effects of noise, vibration, heat, cold or radiations), or through the physical effects of environments which differ from normal ambient conditions (for example those found in diving and compressed air work, at altitude and in flight). The former are much more commonly encountered. In the workplace a healthcare professional may be involved in deciding about an employee’s fitness for work that involves exposure to one or more physical agents, in diagnosing health effects thought to have arisen from such exposures or in giving advice to help prevent such harmful effects. GPs may also see ill health from physical exposures at work and need to be alert to this possible aetiology. They may also be consulted by their patients about the health effects of work, particularly where there is a long-term risk of serious effects such as cancer (Box 15.1).
The potential effects of physical agents range from discomfort and interference with work tasks, right through to death, either acutely or many years after exposure. These effects have been well researched and are mostly well understood. Physical agents are amenable to measurement which, when applied in epidemiological studies, allows a dose–response effect to be established and, from this, acceptable exposure standards. These can then be translated into statutory controls. Measurement and exposure standards for physical agents are often published by international agencies. Accessing these standards and national legislation will provide a good introduction to the hazards associated with each of the physical agents. Textbooks of occupational hygiene give details of measurement methods for each of the physical agents.
Stochastic effects differ from direct effects in that there is considered to be no threshold below which there is no risk, and the probability of an effect arising relates to the dose received. The direct effects of physical agents are regarded as having a threshold below which harm does not arise, and a dose–response relationship where the magnitude of the effect is related to the magnitude of the exposure.
Prevention of harm from physical agents relies on controlling exposures. It may be possible to find alternative ways of doing a job that cut down on exposure, for example pulling a bolt through metal, rather than knocking it through–this can cut down on both noise and vibration exposure. If substitution is not possible, then control at source should be considered. Personal protective equipment is often relied on, for example the use of hearing defenders, but is often not perfect in practice, and should be regarded as a last resort. Some exposures cannot be modified such as outdoor work environments or the effects of pressure when diving. Administrative controls based on a thorough risk assessment will be necessary and these may include screening the population of workers for individuals at particular risk.
Advice and guidance on controlling exposures to physical agents is well established and a good place to look for such information is on the websites of health and safety organizations such as the Health and Safety Executive (HSE) in Great Britain (Box 15.2) or the National Institute for Occupational Safety and Health (NIOSH) in the USA (Box 15.3). Once there is a good understanding of the principles involved, it may be necessary to involve an occupational hygienist or a health physicist to quantify exposures in a particular workplace of concern.
Noise
Occupational noise exposure is one of the most ubiquitous workplace hazards and the harmful effects of noise on hearing have been known since at least the nineteenth century. Progressive deafness beginning with the high frequencies, typically centred on 4 kHz, and gradually spreading to other frequencies, should be a preventable occupational disease. Although hearing loss can be documented by audiometry, tinnitus, which cannot be objectively quantified, can be more distressing for sufferers. Noise also has other effects such as stimulation of the hypothalamic adrenal system and resulting ‘stress’ and changes in blood pressure as well as effects on performance, which depend on the task duration and type of exposure (Figure 15.1).
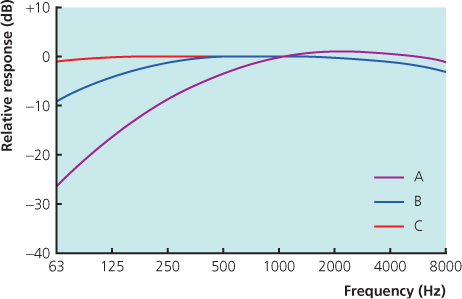
The harmful effects of noise depend on both the magnitude and duration of exposure and are dependent on the total noise energy to which the ear is exposed. Sudden massive overexposure to peak noise of 140 dB(A) or more can cause mechanical damage, ‘acoustic trauma’, resulting in loss of hearing often accompanied by tinnitus. For continuous noise, exposure criteria for an 8-hour working day have been established and do so using noise measurements which are frequency weighted to take account of the sensitivity of the human ear to noise exposure. This is the ‘A’ weighting of noise measurements. Sound levels are measured in decibels (dB) where a figure of 0 represents (Figure 15.2) the limit of detection of sound by the human ear and an increase of 3 dB, on a logarithmic scale, represents a doubling of sound intensity. A daily personal noise exposure (LEP, d) of 85 dB(A) is a level at which the risk of hearing damage is significant and where employers are usually expected to take action to assess and reduce noise exposures. Within the EU a lower action level is set at a daily personal noise exposure at 80 dB(A), an upper exposure action level at 85 dB(A) and the exposure limit value for continuous sound is set at 87 dB(A). Different actions are required at each of these levels, for example hearing protection must be provided only on request, at or above the lower action value. An area where workers are likely to be exposed at or above the upper action value must be designated as a hearing protection zone. Now, hearing protectors must be provided to employees, who are also required to use them. Details of the many other requirements are to be found in the relevant legislation and associated guidance.
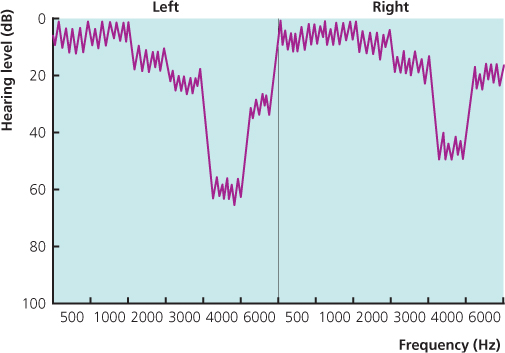
Health surveillance by audiometry will often be required for noise-exposed workers. Testing can be done at the start of a shift to avoid temporary changes in hearing threshold. The results should give a more accurate estimate of hearing function than measurements taken during a shift, although some argue that the latter approach better reflects the overall effects of noise on the individual’s hearing at work. If changes are found on a mid-shift audiogram they should be followed up with a pre-shift assessment (Figure 15.3).
The audiogram is not of itself diagnostic of noise induced hearing loss and has to be interpreted along with the occupational and medical history of the individual employee and a clinical examination. A typical high-frequency dip in the audiogram, in the presence of a history of occupational noise exposure, no significant non-occupational noise exposure and no medical factors which could account for the changes would be presumptive of changes of noise induced hearing loss. A full history of occupational and non-occupational noise exposure has to be taken. Leisure noise may occur from shooting, motor sports, attending concerts and night clubs/discos, in-car entertainment systems and from personal music players. Medical factors potentially affecting the audiogram (Box 15.4) include congenital effects, childhood illnesses, trauma to the head, ear disease such as otosclerosis, exposure to drugs such as aminoglycosides and the effects of ageing. Occupational exposure to aromatic solvents such as styrene may act synergistically with noise exposure in the production of sensorineural hearing loss. Clinical examination including Weber’s and Rinne’s tests will help to classify a hearing loss as conductive or sensorineural. Ageing also results in a high-frequency loss, with the hearing threshold levels falling off at the higher frequencies. Often a pattern suggestive of both noise effects and age is apparent on the audiogram. Other factors with a detrimental effect on hearing thresholds include smoking, high blood pressure and high cholesterol levels.
It will be appropriate to refer the employee to their GP where there is a significant hearing loss that might benefit from the use of a hearing aid, or where undiagnosed medical factors are suspected. One example is where there is a unilateral hearing loss, and particularly where this affects all frequencies. This pattern can be produced by an acoustic neuroma and referral is usually followed by imaging studies which can detect this condition.
Some jurisdictions, for example the United Kingdom, publish guidance based on the audiometric thresholds to help those responsible for advising workers on the significance of their test results. Workers who have developed a mild to moderate hearing loss can usually continue to work in noise exposed environments provided that their future noise exposures are well controlled and they remain under health surveillance.
A clinical assessment following health surveillance is a good opportunity to reinforce messages about the need for meticulous use of hearing protection in all noise exposed workers. For workers with severe hearing loss and limited residual hearing thresholds, the potential risk to that hearing from continuing occupational noise exposure may outweigh the benefits of remaining in the job, evenwhere exposures are thought to be well controlled. Some workers experiencing tinnitus find this exacerbated by noise exposure and may be difficult to place in noisy workplaces (Figure 15.4).
Vibration
Exposure to hand-transmitted vibration (Figure 15.5) is a common experience in a wide range of manufacturing, agricultural and other occupations. Tools are often held with both hands, with one hand being used to operate the controls of the equipment and the other hand used to guide the tool as it is used against the workpiece. The harmful effects of this type of exposure were first noted in the second decade of the twentieth century, as an occupational form of Raynaud’s phenomenon. These effects were confirmed in studies during and after the Second World War, and by the latter part of the century three different types of harm from hand-transmitted vibration were recognized, vascular, sensorineural and musculoskeletal effects, all considered to be components of hand arm vibration syndrome (HAVS). Descriptors for the stages of vascular and sensorineural HAVS were introduced in 1987 following a workshop held in Stockholm (Table 15.1).
Table 15.1 Stockholm workshop classification
| Vascular component | ||
| Stage | Grade | Description |
| 0 | No attacks | |
| 1V | Mild | Occasional attacks affecting only the tips of one or more fingers |
| 2V | Moderate | Occasional attacks affecting distal and middle (rarely also proximal) phalanges of one or more fingers |
| 3V | Severe | Frequent attacks affecting all phalanges of most fingers |
| 4V | Very severe | As in stage 3 with trophic changes in the fingertips |
| Sensorineural component | ||
| Stage | Description | |
| 0SN | Vibration-exposed but no symptoms | |
| 1SN | Intermittent numbness with or without tingling | |
| 2SN | Intermittent or persistent numbness, reduced sensory perception | |
| 3SN | Intermittent or persistent numbness, reduced tactile discrimination or manipulative dexterity or both | |
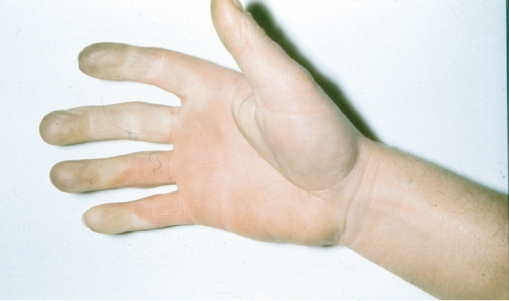
The vascular effects of HAVS are similar to naturally occurring Raynaud’s phenomenon. Part of one or more fingers experiences intense constriction of superficial blood vessels such that the affected part appears white or dusky yellow in appearance with a clear demarcation between the affected part and the normally perfused skin. Typically the whole circumference of the digit is affected and it is numb and dead to touch during an episode. The finger will rewarm if rubbed or held against a warm body surface but otherwise will stay white or ‘blanched’ for 15 minutes or more. It is necessary to take a detailed history from patients to establish whether what is being described is an exaggerated but normal response to peripheral cooling or true episodes of finger blanching. Patients can now use a mobile phone to take photographs to show their medical advisers. Primary Raynaud’s phenomenon affects about 5% of the normal male population and can occur in vibration-exposed workers. It can be difficult to distinguish between the primary and secondary forms (Figure 15.6).
Figure 15.6 Vascular hand arm vibration syndrome, finger blanching. Donated by the late Professor Taylor to HSE.
The sensorineural effects of HAVS are tingling and numbness of the fingers tips associated with reduced tactile sensitivity. These can progress to a level resulting in significant loss of manual dexterity, and so it is important that they are detected early to allow a reduction in, or cessation of vibration exposure. Such symptoms can also occur as a result of other common problems such as nerve entrapment in the neck, and cubital or carpal tunnel syndromes. Carpal tunnel syndrome can also occur in workers exposed to hand-transmitted vibration and may occur more frequently than sensorineural HAVS. A careful clinical assessment has to be made to ascertain the likely cause of sensory symptoms in the fingers of workers exposed to hand-transmitted vibration (Box 15.5).
Vascular conditions
- Connective tissue disease—scleroderma, mixed connective tissue disease, systemic lupus erythematosus, rheumatoid arthritis, dermatomyositis, polyarteritis nodosa, Sjogren’s disease
- Traumatic—after injury or surgery, hand transmitted vibration, frostbite, thoracic outlet syndrome
- Arterial disease—thromboangitis obliterans, thromboembolism, arteriosclerosis
- Toxins and drugs—vinyl chloride, ergot, beta-blockers, clonidine
- Dysglobulinaemia—cryoglobulinaemia
- Neurogenic—poliomyelitis, syringomyelia, hemiplegia
Neurological conditions
- Peripheral nerve entrapment—carpal tunnel syndrome, ulnar nerve entrapment at elbow or wrist, thoracic outlet syndrome
- Central nervous system disorders—compression myelopathy (spondylosis or spinal cord tumor), subacute combineddegeneration of the cord, multiple sclerosis
- Peripheral neuropathy—diabetic, alcoholic, toxic (e.g. organophosphates, thallium, acrylamide, carbon disulphide, n-hexane, methyl butyl ketone, diethyl thiocarbamate, lead)
- Drug induced (for example, chloramphenicol, isoniazid, streptomycin, polymyxin, ethambutol, nitrofurantoin, metronidazole, gold, indomethacin, vincristine, perhexiline, phenytoin)
The musculsoskeletal component of HAVS is poorly defined and derives from reports of radiograph changes and upper limb pain in workers using vibrating tools. As these tools are often heavy and awkward to manipulate upper limb symptoms are more likely to result from the poor ergonomics of tool use.
Workers regularly exposed to significant hand-transmitted vibration should be under health surveillance to detect any early evidence of HAVS. As a diagnosis can have important economic consequences for the worker it is essential to take time to be sure of the findings and it will often be necessary to assess the worker on more than one occasion before reaching a conclusion about the origin of symptoms. Depending on the level of symptoms work involving exposure to hand transmitted vibration can be permitted with reduced vibration exposure and ongoing surveillance. This is most easily achieved where there is robust vibration exposure information available to the occupational health professional.
Drivers of mobile machinery and many modes of transport are exposed to vibration principally through their seating, although there may be a small component of hand-transmitted vibration experienced from a steering wheel or other controls. The vibration transmitted through the floor, seat cushion or seat back is whole-body vibration. Some workers who have to stand on vibrating surfaces are also subject to whole-body vibration exposure. Many health effects have been reported from whole-body vibration exposure, but for practical purposes the only one of significance is low back pain. Even here there is some question whether the effect is due to vibration itself or the effects of seated posture, twisting and turning (for example in tractor driving) and associated manual handling tasks. Low back pain arising from vibration exposure cannot be distinguished from that arising from other causes, but workers exposed to whole-body vibration may suffer low back pain at an earlier age that their non-exposed contemporaries. Workers should be aware of this possibility and have a means to report any symptoms. Reduction of exposure can be achieved by the fitting of seating with vibration dampers, by ensuring that the seat is adjusted correctly for the individual driver and by paying close attention to the surfaces that have to be driven over, for example filling in pot holes and removing other rough surfaces on roadways or factory floors (Figure 15.7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree