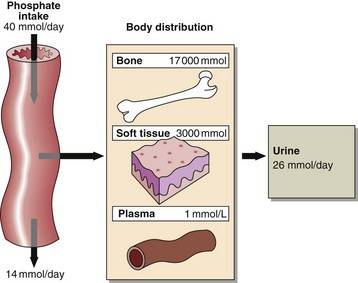
37 Phosphate is abundant in the body and is an important intracellular and extracellular anion. Much of the phosphate inside cells is covalently attached to lipids and proteins. Phosphorylation and dephosphorylation of enzymes are important mechanisms in the regulation of metabolic activity. Most of the body’s phosphate is in bone (Fig 37.1). Phosphate changes accompany calcium deposition or resorption of bone. Control of ECF phosphate concentration is achieved by the kidney, where tubular reabsorption is reduced by PTH. The phosphate that is not reabsorbed in the renal tubule acts as an important urinary buffer. Causes of a low serum phosphate include:
Phosphate and magnesium
Phosphate
Hyperphosphataemia
 Renal failure. Phosphate excretion is impaired. This is the commonest cause of hyperphosphataemia.
Renal failure. Phosphate excretion is impaired. This is the commonest cause of hyperphosphataemia.
 Hypoparathyroidism. The effect of a low circulating PTH decreases phosphate excretion by the kidneys, and this contributes to a high serum concentration.
Hypoparathyroidism. The effect of a low circulating PTH decreases phosphate excretion by the kidneys, and this contributes to a high serum concentration.
 Redistribution. Cell damage (lysis), e.g. haemolysis, tumour damage and rhabdomyolysis.
Redistribution. Cell damage (lysis), e.g. haemolysis, tumour damage and rhabdomyolysis.
 Acidosis. There is impaired metabolism and therefore decreased intracellular utilization of phosphate.
Acidosis. There is impaired metabolism and therefore decreased intracellular utilization of phosphate.
 Pseudohypoparathyroidism. There is tissue resistance to PTH.
Pseudohypoparathyroidism. There is tissue resistance to PTH.
Hypophosphataemia
 Hyperparathyroidism. The effect of a high PTH is to increase phosphate excretion by the kidneys and this contributes to a low serum concentration.
Hyperparathyroidism. The effect of a high PTH is to increase phosphate excretion by the kidneys and this contributes to a low serum concentration.
 Treatment of diabetic ketoacidosis. The effect of insulin in causing the shift of glucose into cells may cause similar shifts of phosphate, which may result in hypophosphataemia.
Treatment of diabetic ketoacidosis. The effect of insulin in causing the shift of glucose into cells may cause similar shifts of phosphate, which may result in hypophosphataemia.
 Alkalosis. Especially respiratory, due to movement of phosphate into cells.
Alkalosis. Especially respiratory, due to movement of phosphate into cells.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Phosphate and magnesium