1 Pharmacodynamics and pharmacokinetics
Part of the nurse’s role, alongside the pharmacist, is the need to ensure that medicines are administered appropriately. That is why it is essential that the nurse has a good knowledge and understanding of pharmacology and the relevant calculations in terms of patient care. Pharmacology is the study of drugs (chemicals) and their interactions with the body. The term is derived from the Greek pharmakon which can mean both ‘remedy’ and ‘poison’. In modern medical practice we use drugs more and more to treat and manage disease, so it is vital that nurses understand the basic mechanisms of drug action and reaction.
The aim of this chapter is to introduce the basic principles of pharmacology in relation to nursing practice. The chapter will give you an appreciation of pharmacodynamics and pharmacokinetics. It will identify the main targets for drug action and allow you to develop an understanding of drug absorption, distribution, metabolism and excretion.
Put simply:
- pharmacodynamics is the effect that drugs have on the body; while
- pharmacokinetics is the study of the way in which drugs move through the body during absorption, distribution, metabolism and excretion.
For drugs to produce their effects they must interact with the body. This can happen in many ways and depends on the properties of the drug, and will be discussed later in this chapter. Pharmacokinetics influences decisions over the route of administration. The processes that occur after drug administration can be broken down into four distinct areas (known as ADME):
A Absorption of the drug
D Distribution of the drug molecules
M Metabolism of the parent drug
E Excretion or elimination of the drug and its metabolites
Absorption
Before a drug can begin to exert any effect on the body it has to be absorbed into the body systems. This absorption process can be affected by many things but the main factor relating to absorption is the route of administration (see Box 1.1).
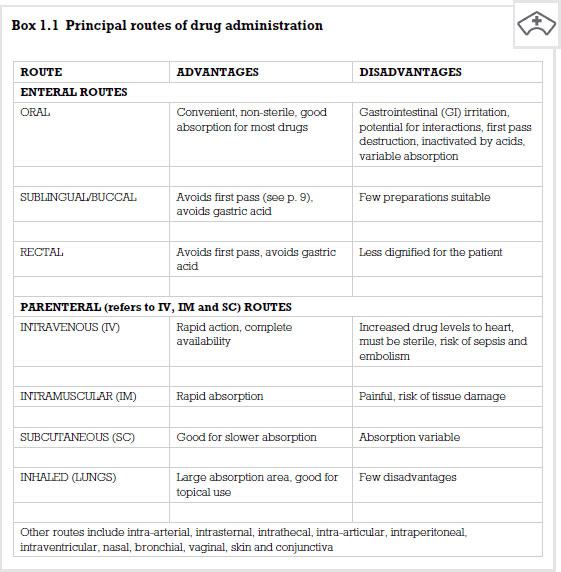
It is important that nurses understand the implications attached to choosing routes of administration of drugs based on their absorption. Many patients may need to have their medication administration tailored to their particular medical condition or the medication which they are prescribed, and this is an important factor to consider as it can impact on the patient’s ability or desire to take their medication.
Other factors controlling the rate and reliability of drug absorption can be said to be physiological or physico-chemical.
Physiological factors relate to human physiological functions:
- Blood flow to absorbing site. The better the blood supply to the area the greater the rate of absorption. Therefore if a person has a good circulation they will have the ability to absorb the drug well.
- Total surface area for absorption. The greater the surface area the greater the rate of absorption. The intestine has a very large surface area, making it an ideal target for drug absorption. This is why you will find that most drugs are given orally where possible.
- Time of arrival and contact time at absorption site. The longer the drug is in contact with the absorbing surface the greater the rate of absorption. This is why if a person is suffering from diarrhoea the chances of a drug given orally being absorbed completely are lowered and other means of administration must be considered.
Physico-chemical factors relate to the chemical make-up of the drug in relation to human physiological function:
- Solubility. How soluble is the drug in body fluids? As the body is made up of a large amount of water, drugs can dissolve readily. However, certain drugs do not dissolve into small enough particles to ensure rapid absorption.
- Chemical stability. Will it break down readily?
- Lipid to water partition coefficient. Is it more fat soluble than water soluble? This is an important area to consider. As your cells are made up of a phospho-lipid layer, any drug that can dissolve well in lipids will pass through your tissues far more rapidly. Examples of drugs that are highly lipid soluble are anaesthetic agents and benzodiazepines.
- Degree of ionization. Some drugs are weak acids and weak bases (alkalis). These drugs tend to disassociate when given to a person. This means that some of the drug remains active and some is inactive. Often this depends on the pH of the solution (i.e. its acidity or alkalinity) in which the drug is being dissolved. For example, a weak acid does not disassociate as much if dissolved in an acid environment. This means that the drug can cross membranes in a more active form than if it had been dissolved in a neutral or base solution.
- Chemical stability. Will it break down readily?
Distribution
Once drugs have been administered and absorbed, they have to be distributed to their site of action. For some drugs that site is known and such drugs are available to give locally or topically. All other drugs need to be distributed throughout the body.
There are four main elements to this:
1. Distribution into body fluids. These are mainly plasma, interstitial fluid and intracellular fluid. Molecular targets for drugs are found in these areas.
2. Uptake into body tissues/organs. Specific tissues take up some drugs – for example, iodine and thyroid gland.
3. Extent of plasma protein binding. Plasma proteins such as albumin can bind drug molecules. This varies widely among drugs. Drugs bound to plasma proteins are pharmacologically inert; only free drugs are active. Some drugs do not bind (e.g. caffeine) and some are highly bound (e.g. warfarin which is 99 per cent bound to plasma proteins). Some drugs can displace others from their binding sites on the plasma proteins – for example, phenylbutazone can displace warfarin from plasma proteins. This is an important consideration for drugs which have this effect.
4. Passage through barriers. The two main examples are the placenta and the blood-brain barrier (BBB). Drugs must be highly lipid soluble to pass across these barriers. If not, they may not be able to reach their site of action.
The factors which affect drug distribution are taken into consideration by drug companies when developing and formulating medications. While these factors are of interest, the nurse’s role in monitoring drug distribution is mainly in monitoring the onset of the effect of, or the response to, the medication. If analgesia is given and the patient reports reduced or relieved pain, the drug has been distributed to its target site.
Biotransformation
Biotransformation of drugs is the process of metabolizing the parent drug compound and occurs mainly in the liver (hence the term hepatic metabolism) to different compounds called metabolites. The drug metabolite may have decreased, increased or undergone no change in pharmacological activity compared to the parent drug. It may also have a different activity. Some drugs are what are termed pro-drugs – that is the drug itself is pharmacologically inactive until it is metabolized by the liver to its active form. A good example is codeine, which is metabolized to morphine by the body. The metabolite is more polar (i.e. chemically charged) than the parent drug and therefore is more readily excreted by the kidney. Drug metabolism can influence dose and frequency of dosing. Drugs which are metabolized quickly have a short duration of action and need to be administered more often (two, three or four times daily). Drugs which are metabolized slowly can have a longer duration of action and may only need to be given on a once-daily basis.
Hepatic metabolism
The terms shown in Table 1.1 are different chemical reactions that change the properties of drugs to facilitate their removal from the body by excretion. Most drugs undergo phase I oxidation followed by phase II conjugation.
Table 1.1 Metabolic phases and processes
| Phase | Process |
| Phase I metabolism | Oxidation |
| Reduction | |
| Hydrolysis | |
| Phase II metabolism | Conjugation |
Excretion
Once drugs have had their desired effect they need to be excreted by the body. Principles of excretion include renal elimination and clearance, secretion into bile for faecal elimination and enterohepatic recirculation. As previously outlined, some drug metabolites can also have pharmacological effects. If these compounds were not eliminated, they would accumulate in the bloodstream and could cause toxic and unwanted effects.
The main method of renal elimination is by active glomerular filtration. This is where ionized drugs are actively secreted into the proximal tubule. These ionized compounds are actively excreted by the kidney and are ‘pushed’ out into urine. A more passive form of drug compound movement occurs in the distal tubule of the kidney. Here there is passive reabsorption and excretion of drug molecules and metabolites according to a concentration gradient. Molecules move from a high concentration to a lower concentration by diffusion. This applies to unionized compounds (drugs without charge), and prevents the entire dose of a drug being excreted at once. This helps to maintain circulating plasma levels to allow the drug effect to continue until the next dose is taken.
Excretion into bile is another method of eliminating drug molecules and metabolites. These are secreted from the liver into bile and into the gut for faecal elimination. As in renal excretion, not all of the drug and its metabolites are eliminated entirely at once. Some drugs undergo enterohepatic recirculation. This is where some of the drug is reabsorbed from the gut, back into the bloodstream and represented to the liver for further metabolism. This can help to maintain circulating levels of active molecules to prolong drug effect until the next dose. An important example of a drug that undergoes this is the combined oral contraceptive pill.
It is important that nurses involved in medicines management are aware of the sites of action for many commonly used drugs. Drugs exert their effects at molecular (chemical) targets, of which there are many. Below are some of the commonest.
Receptors
The plasma membrane of a human cell is selectively permeable in that it helps control what moves in and out of the cell. The cell membrane consists of a thin structured bilayer of phospholipids and protein molecules. The surfaces of plasma membranes are generally studded with proteins that perform different functions, like the reception of nutrients. In biochemistry these protein molecules are referred to as receptors. Molecules which bind to these receptors are called ligands. Examples of ligands are neurotransmitters, hormones or drugs.
A large number of drugs, which are clinically effective, exert their action by interaction with receptors. Examples include:
- ligand-gated ion channels (ionotropic receptors) such as the GABAA receptor, which binds benzodiazepines;
- G-protein coupled receptors such as adrenoceptors;
- kinase-linked receptors such as the insulin receptor;
- nuclear receptors such as the thyroid receptor.
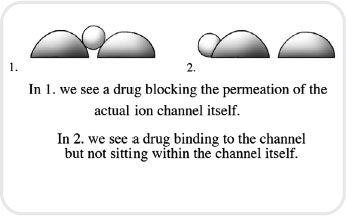
Ion channels
Ion channels provide receptors which drugs can interact with. Drug actions at ion channels can take two forms (see Figure 1.1). The first form are known as channel blockers, whereby the drug blocks permeation of the channel, and the second are channel modulators whereby the drug binds to a receptor site within the ion channel and modulates permeation of the channel. This can happen by the drug altering the channel’s response to its normal mediator.
< div class='tao-gold-member'>