Peripheral Neuroepithelioma/Primitive Neuroectodermal Tumor
Alexandros D. Polydorides, MD, PhD
Key Facts
Terminology
Rare malignant small round blue cell tumor
Variable evidence of neuroectodermal differentiation
Etiology/Pathogenesis
From neural crest cells or primitive neuroepithelium
t(11;22)(q24;q12) in 90% of cases (EWS-FLI-1 fusion)
Related to Ewing sarcoma (same translocation)
Probably phenotypic spectrum of the same entity
Clinical Issues
Trunk, extremities, scalp, face, neck, shoulder
Painless nodules, misdiagnosed as benign tumor, cyst
Highly aggressive behavior, distant metastases
5-year disease-free survival: ˜ 60%
Macroscopic Features
Hemorrhagic, ulcerated or polypoid, ill-defined mass
Microscopic Pathology
In dermis, focal extension into superficial subcutis
Sheets, nests, lobules, trabeculae and cords of cells
Delicate reticulin positive fibrovascular stroma
Monomorphic cells, no nucleoli, scant cytoplasm
Intercellular vague Homer Wright rosettes
Mitoses, apoptosis, necrosis (may be confluent)
Ancillary Tests
Diffusely, strongly positive for membranous CD99
Positive for 1 or more neural markers (e.g., NSE)
Membrane-bound dense core neurosecretory granules
Intracytoplasmic glycogen commonly seen
Diagnostic Checklist
Primary vs. metastatic, e.g., metastatic neuroblastoma
Histologically indistinguishable; work-up required
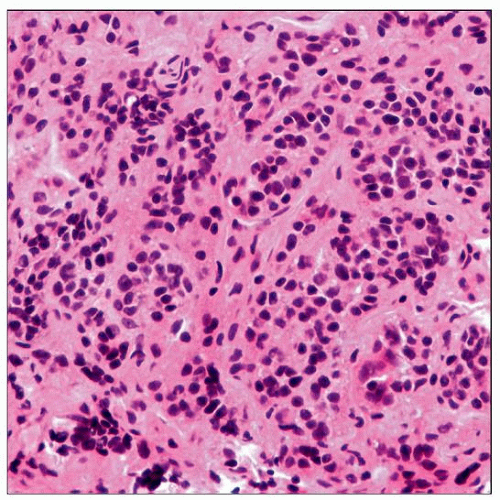
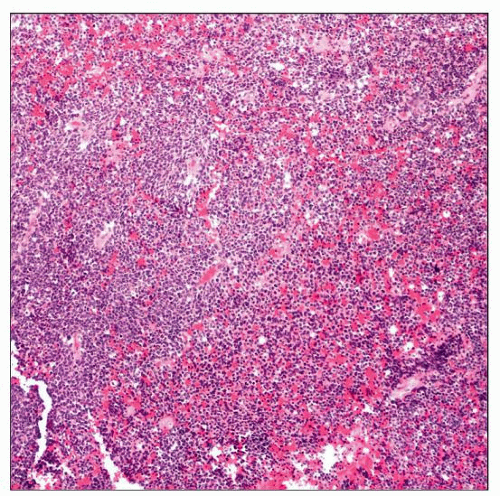 Low-power view shows PNET with the classic appearance of patternless, hypercellular lobules to sheets of undifferentiated, “small round blue” cells. |
TERMINOLOGY
Abbreviations
Primitive neuroectodermal tumor (PNET)
Peripheral neuroepithelioma (PNE)
Synonyms
Primary malignant peripheral PNET
Peripheral (cutaneous) neuroblastoma
Extraskeletal Ewing sarcoma
Definitions
Rare malignant small blue round cell tumor of dermis and superficial subcutis
Variable evidence of neuroectodermal differentiation (morphologic, ultrastructural, immunohistochemical)
ETIOLOGY/PATHOGENESIS
Histogenesis
Not entirely clear, regarded as controversial
Derived from neural crest cells or neuroepithelium of primitive neuroectodermal tissue
Alternatively, from primitive neuroepithelial cell
Considered PNET of peripheral nervous system
Thought to arise from peripheral nerves
Not connected to sympathetic nervous system
Morphologic similarities with other embryonal tumors
Assumed to share common histogenetic origins
Central nervous system PNET (medulloblastoma)
Askin tumor (chest wall/thoracopulmonary PNET)
Genetics
t(11;22)(q24;q12)
Related to Ewing sarcoma (same translocation)
Probably phenotypic spectrum of same tumor
CLINICAL ISSUES
Epidemiology
Incidence
Very rare (especially if metastasis excluded)
Age
Children, adolescents, young adults (20s)
Occasionally may affect older patients
Gender
No gender predilection reported
Site
Trunk, extremities, scalp, face, neck, shoulder
May uncommonly involve vulva, vagina
Presentation
Mostly painless nodules
But may be tender
May be clinically misdiagnosed as benign tumor or cyst
Usually do not secrete catecholamines or metabolites
Natural History
Highly aggressive behavior
May grow rapidly
Distant metastases common
Regional lymph nodes, lung, liver, bones, brain
Treatment
Surgical approaches
Goal is complete surgical resection
Adjuvant therapy
Chemotherapy and radiation
Prognosis
Slightly better than soft tissue counterpart
Probably due to earlier detection
5-year disease-free survival: ˜ 60%
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree