4 Peripheral nervous system
Nerve conduction
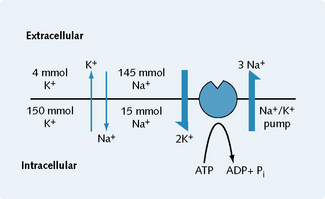
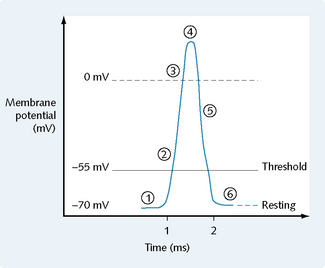
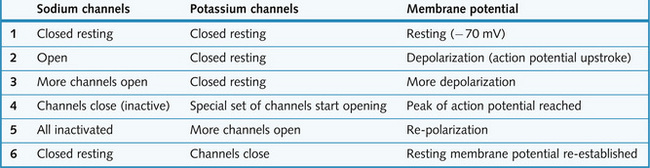
Figure 4.1 shows the concentrations of sodium and potassium inside and outside a resting nerve. The Na+/K+ pump (Na+/K+ ATPase) is an energy-dependent pump that functions to maintain the concentration gradient of these two ionic species across the membrane. Three sodium ions are pumped out of the cell for every two potassium ions pumped in, and thus the excitability of the cell is retained. Figures 4.2 and 4.3 summarize the events that occur during a nerve action potential. During a nerve action potential:
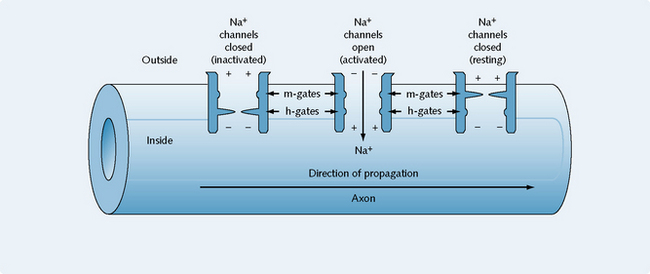
Figure 4.4 shows the voltage-operated sodium channels in their inactivated, activated and resting states. Two types of gate exist within the channel; the m-gates and the h-gates. These gates are open or closed according to the state of the channel.
Somatic nervous system
Neuromuscular junction
Physiology of transduction
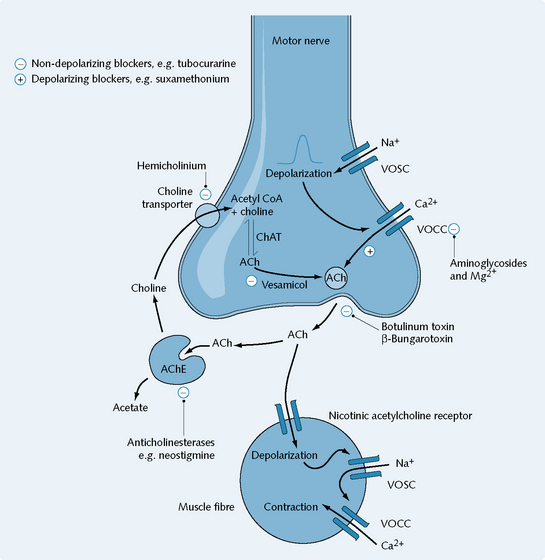
The axon terminal incorporates membrane-bound vesicles containing the neurotransmitter acetylcholine (ACh). Depolarization of the presynaptic terminal of the nerve by an action potential (generated by sodium influx) causes voltage-sensitive calcium channels to open, allowing calcium ions into the terminal. Normally, the level of calcium ions inside the nerves is very low, much lower relative to the external concentration. This calcium influx results in the release of ACh by exocytosis from vesicles. ACh diffuses across to the muscle membrane where it binds to the nicotinic acetylcholine receptor (nicAChR) and/or is inactivated by acetylcholinesterase (Fig. 4.5). Several events then occur:
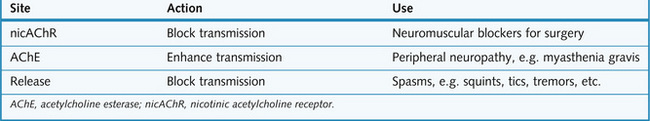
Drugs affecting the neuromuscular junction
Presynaptic agents
Postsynaptic agents
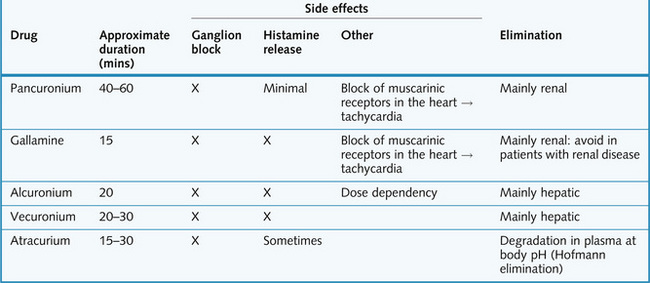
Non-depolarizing blockers
These act as competitive antagonists by binding to the nicAChR but not activating it, and producing motor paralysis. Details of the most commonly used non-depolarizing blockers are given in Figure 4.7