12 Peptic ulcer disease
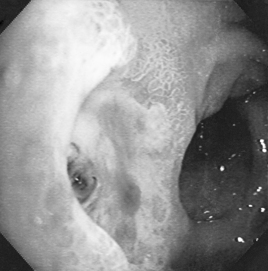
The term ‘peptic ulcer’ describes a condition in which there is a discontinuity in the entire thickness of the gastric or duodenal mucosa that persists as a result of acid and pepsin in the gastric juice (Fig. 12.1). Oesophageal ulceration due to acid reflux is generally classified under GORD. This definition excludes carcinoma and lymphoma, which may also cause gastric ulceration, and also excludes other rare causes of gastric and duodenal ulceration such as Crohn’s disease, viral infections and amyloidosis. About 10% of the population in developed countries is likely to be affected at some time by peptic ulcer, with the prevalence for active ulcer disease being about 1% at any particular point in time.
Epidemiology
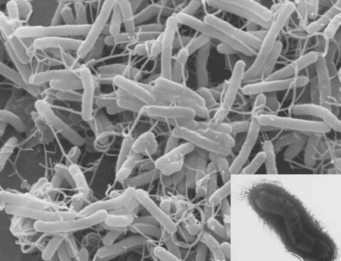
Infection by H. pylori, a spiral bacterium of the stomach, remains an important epidemiological factor in causing peptic ulcer (Fig. 12.2). Most H. pylori infections are acquired by oral–oral and oral–faecal transmission. The most important risk factors for H. pylori infection are low social class, overcrowding and home environment during childhood, for example, bed sharing. Transmission may occur within a family, a fact demonstrated by the finding that family members, especially spouses, may have the same strain of H. pylori. H. pylori seropositivity increases with age as colonisation persists for the lifetime of the host. Subjects who become infected with H. pylori when young are more likely to develop chronic or atrophic gastritis with reduced acid secretion that may protect them from developing duodenal ulcer. However, it may promote development of gastric ulcer as well as gastric cancer. Duodenal ulcer seems to develop in those who are infected with H. pylori at the end of childhood or later. Historically, developing countries have a higher ratio of duodenal ulcer to gastric ulcer but as rates of H. pylori infection decline with improvements in hygiene and rates of gastric ulcer increase with the use of ulcerogenic drugs, this ratio of duodenal to gastric ulcer is declining. The prevalence of H. pylori still tends to be higher in the Asian adult population in whom a lower parietal cell mass has been found. These factors together with slower metabolism may explain the greater efficacy of PPIs in Asian populations. There may be other genetic, environmental or cultural factors influencing peptic ulcer disease.
Pathogenesis
Helicobacter pylori
This organism is a Gram-negative microaerophilic bacterium found primarily in the gastric antrum of the human stomach (see Fig. 12.2). Ninety-five percent or more of duodenal ulcers and 80–85% of gastric ulcers are associated with H. pylori. The bacterium is located in the antrum and the acid-secreting microenvironment of the corpus of the stomach is less hospitable to the bacterium. In the developed world, reinfection rates are low, about 0.3–1.0% per year, whereas in the developing world reinfection rates are higher, approximately 20–30%. Ulcerogenic strains of H. pylori, ulcer-prone hosts, age of infection and interaction with other ulcerogenic factors such as NSAIDs determine peptic ulcer development following H. pylori infection. The contribution of H. pylori infection to the risk of ulcers in NSAID users is not clear but there appears to be an additive effect. The risk of peptic ulcer in long-term NSAID users is greater in those who test positive for H. pylori and eradication of H. pylori in these patients prior to commencing NSAID treatment has been shown to reduce the risk of H. pylori NSAID-associated peptic ulcer.
Non-steroidal anti-inflammatory drugs
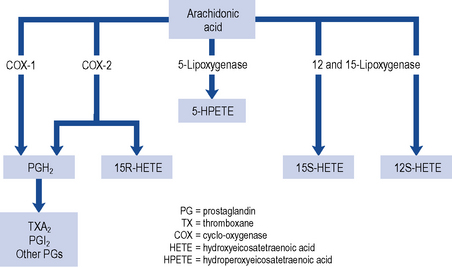
Three patterns of mucosal damage are caused by NSAIDs. These include superficial erosions and haemorrhages, silent ulcers detected at endoscopy and ulcers causing clinical symptoms and complications. Weak acid NSAIDs, such as acetylsalicylic acid, are concentrated from the acidic gastric juice into mucosal cells, and may produce acute superficial erosions via inhibition of COX and by mediating the adherence of leucocytes to mucosal endothelial cells. Enteric coating may prevent this superficial damage but does not demonstrate any clinical benefit in terms of reduction of gastro-intestinal bleeding or ulceration (Bhatt et al., 2008). The major systemic action of NSAIDs that contributes to the formation of ulcers is the reduction of mucosal prostaglandin production. All NSAIDs share the ability to inhibit COX (Fig. 12.3). The presence of NSAID-induced ulcers does not correlate with abdominal pain and NSAIDs themselves often mask ulcer pain. Approximately 20% of patients taking NSAIDs experience symptoms of dyspepsia but symptoms correlate poorly with the presence of mucosal damage. Ulcers and ulcer complications occur in approximately 4% of NSAID users every year. Patients taking NSAIDs have a four-fold increase in risk of ulcer complications compared with non-users. The risk of ulcer bleeding in low-dose aspirin users is two- to three-fold and there may be differences in risk factors. For example, the risk with aspirin is less influenced by age than the risk associated with NSAIDs (McQuaid and Laine, 2006) and H. pylori may have greater influence on the risk of bleeding with low-dose aspirin than with NSAIDs (Lanza et al., 2009).
Each year, in the UK population over the age of 60 years, there are ∼︀3500 hospitalisations and over 400 deaths associated with NSAIDs. The risk of ulcer complications (Box 12.1) is progressive depending upon the number of risk factors present (Lanza et al., 2009). The most important risk factors are a history of ulcer complications and advancing age, particularly over 75 years. Ulcers have been found to be more common in patients who have taken NSAIDs for less than 3 months, with the highest risk observed during the first month of treatment. The risk increases with higher doses of NSAID but mucosal damage occurs with even very low doses of NSAIDs, particularly aspirin. Corticosteroids alone are an insignificant ulcer risk, but potentiate the ulcer risk when added to NSAIDs, particularly in daily doses of at least 10 mg prednisolone (Lanza et al., 2009).
Selective cyclo-oxygenase-2 inhibitors
The gastro-intestinal side effects of conventional NSAIDs are mediated through the inhibition of COX-1 (see Fig. 12.3). COX-1 stimulates synthesis of homeostatic prostaglandins while COX-2 is predominantly induced in response to inflammation. Selective COX-2 inhibitors tend not to reduce the mucosal production of protective prostaglandins to the same extent as NSAIDs. COX-2 inhibitors are, therefore, considered to be safer than non-selective NSAIDs in patients at high risk of developing gastro-intestinal mucosal damage. Although studies have confirmed the reduction of endoscopic and symptomatic ulcers (Hooper et al., 2004), an increase in cardiovascular risk, including heart attack and stroke, has resulted in the withdrawal of some COX-2 inhibitors from the market. Additional contraindications are now in place for those COX-2 inhibitors that remain on the market. Amongst the new contraindications is the recommendation that they should not be taken by patients with established heart or cerebrovascular disease, or taken in combination with low-dose aspirin as this negates any beneficial gastro-intestinal protective effects. The need for and choice of anti-inflammatory agent should therefore take into account gastro-intestinal, cardiovascular and other risks such as potential cardio-renal effects. For all agents, the lowest effective dose should be used for the shortest duration.
Nitric oxide-releasing NSAIDs
Nitric oxide (NO)-releasing NSAIDs are being investigated to see if the gastric mucosa protection associated with nitric oxide prevents ulceration when prostaglandins are inhibited by NSAIDs (Fiorucci et al., 2007). Nitric oxide is coupled to the NSAID via an ester, resulting in prolonged release of nitric oxide. Nitric oxide itself has anti-inflammatory effects adding to the potency of the NSAID. Animal studies suggest NO-releasing agents, such as naproxcinod, have minimum cardiovascular and gastro-intestinal toxicity.
Patient assessment
Presenting symptoms of dyspepsia require careful assessment to judge the risk of serious disease or to provide appropriate symptomatic treatment. Symptom subgroups such as ulcer, reflux and dysmotility type may be useful in identifying the predominant symptom subgroup to which a patient belongs. Many patients have symptoms which fit more than one subgroup (Box 12.2). Many patients seek reassurance, lifestyle advice and symptomatic treatment with a single consultation, others have chronic symptoms. In some cases, medications may be the cause of dyspepsia and should be reviewed (Box 12.3).
Patients at any age who present with alarm features (Box 12.4) should be referred for endoscopic investigation. These groups of patients are at a higher risk of underlying serious disease such as cancer, ulcers or severe oesophagitis. Referral is also recommended for patients over the age of 55 if symptoms are unexplained or persistent despite initial management (NICE, 2004; SIGN, 2003). Malignant disease is rare in young people and in those without alarm features.
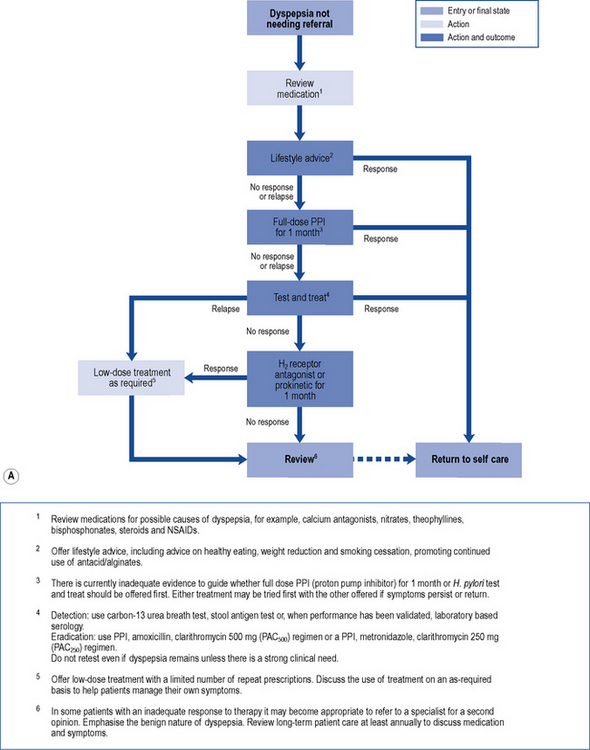
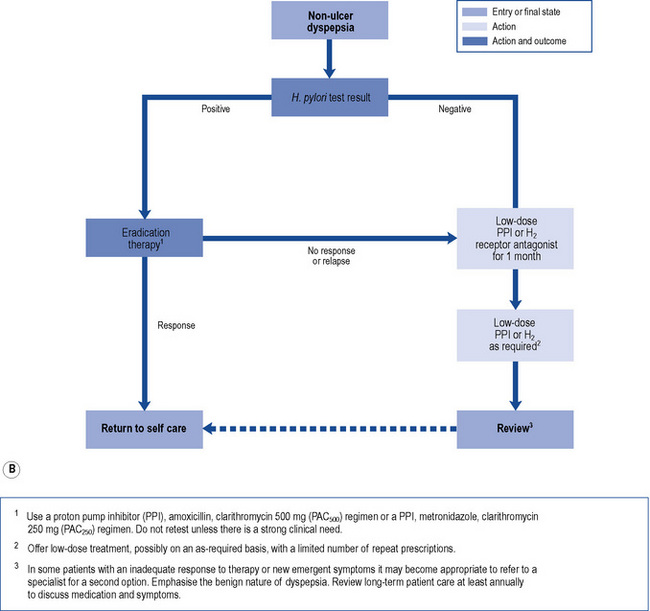
In those patients who do not have reflux-like dyspepsia, testing for the presence of H. pylori is recommended. Eradication treatment should be prescribed for those who test positive and empirical acid suppression for those who test negative. The small proportion of patients with symptoms due to ulcers should be cured. Overall, in functional dyspepsia, symptom control is poor but a small and significant benefit of eradication treatment has been shown. Acid suppression is only of benefit in a small proportion of patients with functional dyspepsia. There is no evidence to support other pharmacological therapies and non-pharmacological strategies may have a future role in functional dyspepsia. Patients should be reassured that the condition is common and not serious. National guidelines (NICE, 2004) provide algorithms to guide practitioners through the management of patients presenting with dyspepsia (Fig. 12.4A and B).
Investigations
Endoscopy
Endoscopy is generally the investigation of choice for diagnosing peptic ulcer, and the procedure is sensitive, specific and safe. However, it is also invasive and expensive. Routine endoscopy in patients presenting with dyspepsia without alarm features (see Box 12.4) is not necessary. Endoscopic investigation should be undertaken in patients with alarm features and in those patients over 55 years who present with unexplained or persistent symptoms of dyspepsia. Biopsies may be taken to exclude malignancy and uncommon lesions such as Crohn’s disease.
Patients with upper gastro-intestinal bleeding have traditionally undergone endoscopy whether as an emergency or on the next available list. Most patients do not require endoscopy and in those at low risk, endoscopy and admission to hospital can be avoided by application of a scoring system. The most widely used is the Rockall risk scoring system which includes endoscopic findings to predict poor outcome. Pre-endoscopic scoring systems are available (Stanley et al., 2009) such as the abbreviated Rockall score or the Glasgow–Blatchford score (GBS) which identify low-risk patients who can be managed safely without endoscopy or admission to hospital.
H. pylori detection
There are several methods of detecting H. pylori infection. They include non-invasive tests such as serological tests to detect antibodies, [13C] urea breath tests and stool antigen tests. Urea breath tests have a sensitivity and specificity over 90% and are accurate for both initial diagnosis and confirmation of eradication. The breath test is based on the principle that urease activity in the stomach of infected individuals hydrolyses urea to form ammonia and carbon dioxide. The test contains carbon-labelled urea which, when hydrolysed, results in production of labelled carbon dioxide which appears in the patient’s breath. The stool antigen test uses an enzyme immunoassay to detect H. pylori antigen in stool. This test also has a sensitivity and specificity over 90% and can be used in the initial diagnosis and also to confirm eradication. However, the breath test is preferable and more convenient. Serological tests are based on the detection of anti-H. pylori IgG antibodies but are not able to distinguish between active or previous exposure to infection. Near patient serology tests are not recommended (Malfertheiner et al., 2007) as they are inaccurate.
Treatment
Complications of peptic ulcer disease
Bleeding peptic ulcer
A number of pharmacological agents have been used for endoscopic injection therapy such as 1:10,000 adrenaline (epinephrine), human thrombin and fibrin glue. Mechanical endoscopic treatment options include thermocoagulation using a heater probe or endoscopic clipping. Combination therapies are superior to monotherapy and a combination of adrenaline 1:10,000 with either thermal or mechanical treatment is recommended (SIGN, 2008; Barkun et al., 2010). Need for surgery, re-bleeding rates and mortality are reduced but bleeding recurs in about 10% of patients and can cause death. Patients with uncontrolled bleeding should receive repeat endoscopic treatment, arterial embolisation or surgery. The risk of recurrent bleeding following endoscopic therapy is reduced by increasing intragastric pH during the first 3 days after the initial bleed and eradication of H. pylori. Biopsies taken at the time of endoscopy are used to detect H. pylori, or the urea breath test can be used once oral intake is established and H. pylori eradication therapy is indicated in those who test positive. Successful eradication of H. pylori reduces the rate of re-bleeding to a greater extent than antisecretory non-eradicating therapy (Gisbert et al., 2004). Following successful H. pylori eradication and healing of the ulcer, there is no need to continue maintenance antisecretory therapy beyond 4 weeks unless required for prophylaxis of ulcer complications in those continuing to take aspirin or NSAIDs (SIGN, 2008).
Acid suppression reduces the re-bleeding rate and should be given to those patients at high risk of re-bleeding following endoscopic haemostatic therapy. The rationale for this is based on the fact that gastric acid inhibits clot formation and if intragastric pH is maintained above 6 during the first 3 days after the initial bleed, there is opportunity for clot stabilisation and haemostasis. Meta-analysis suggests PPIs significantly reduce re-bleeding rates compared with H2-receptor antagonists and are the preferred choice of treatment (Leontiadis et al., 2006). In similar dosage regimens, there is no data to suggest any PPI is more efficacious than another. The optimal dose and route of PPI is unknown in this indication, although reduction in mortality is observed in high-risk patients when high dose PPI therapy is given (e.g. 80 mg bolus omeprazole, pantoprazole or esomeprazole followed by 8 mg/h for 72 h) following endoscopic haemostasis (Leontiadis et al., 2007; SIGN, 2008; Barkun et al., 2010).
The use of intravenous PPI therapy before endoscopy in patients with upper gastro-intestinal bleeding does not affect clinical outcome such as re-bleeding, need for surgery or mortality (Dorward et al., 2006). However, this may reduce the need for endoscopic therapy (Lau et al., 2007) as demonstrated in Asian patients in whom PPIs are more effective. Its benefits are not clear and it is not possible to identify patients with a greater likelihood of being at high risk. Therefore, the use of PPIs is not recommended prior to diagnosis by endoscopy (SIGN, 2008) but may be beneficial if early endoscopy is delayed (Barkun et al., 2010).
In those patients at low risk for re-bleeding and in whom endoscopic therapy is not indicated, usual therapeutic doses of oral PPI are given for 4 weeks to heal the ulcer. Aspirin or NSAIDs should be avoided but if strongly indicated, these patients are given concomitant PPI therapy following successful eradication of H. pylori. The effect of H. pylori eradication on the risk of recurrent ulcer bleeding is greater in patients taking low-dose aspirin than in those taking NSAIDs (Chan et al., 2001). A possible explanation (Lanza et al., 2009) for this might be that aspirin provokes bleeding in H. pylori ulcers and after healing, aspirin is less likely to cause ulceration.
In patients for whom there is a clear indication to continue aspirin therapy, addition of a PPI is of benefit in the prevention of recurrent bleeding in aspirin users (Lai et al., 2002). Clopidogrel alone is not a safer alternative than this combination in terms of prevention of recurrent ulcer bleeding. Cardiovascular and gastro-intestinal risks must be taken into consideration when deciding how long aspirin should be discontinued after a gastro-intestinal bleed. In some cases, low-dose aspirin can be restarted with concurrent PPI treatment within 7 days (Barkun et al., 2010). When the combination of aspirin and clopidogrel is indicated, concomitant PPI therapy is recommended in patients at high risk of gastro-intestinal complications despite the potential drug interaction between PPIs and clopidogrel. An increased risk of myocardial infarction has been observed with the combination of clopidogrel and PPIs (MHRA, 2009). Causality is unclear but it is suggested that through competitive enzyme inhibition, PPIs metabolised by CYP2C19 reduce the conversion of clopidogrel to its active metabolite. Concomitant use is discouraged but if necessary, separation of dosage timing is recommended (Laine and Hennekens, 2010).