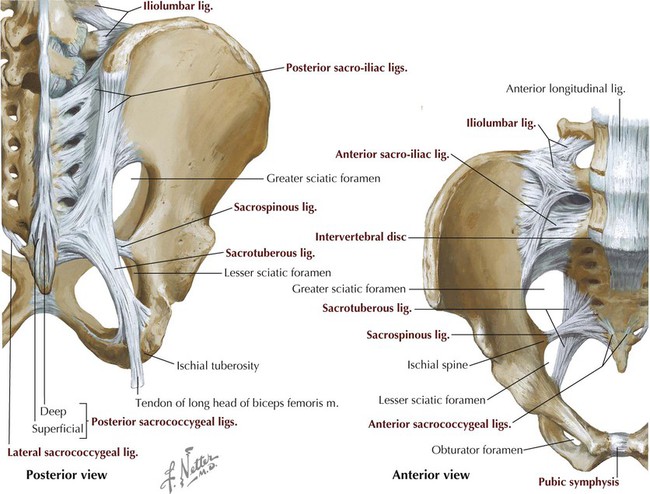
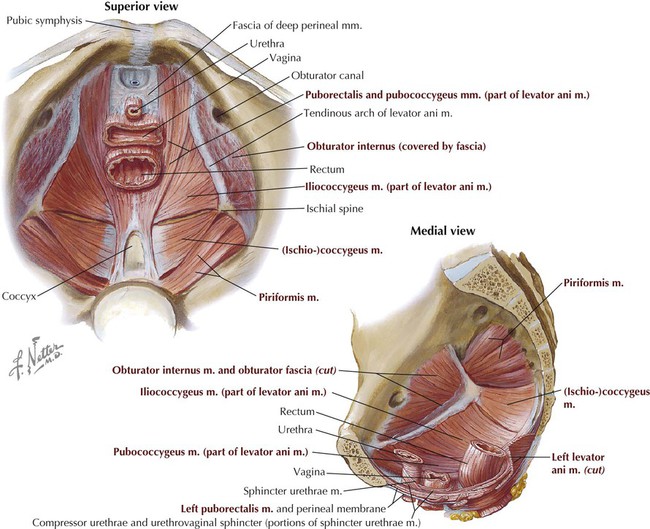
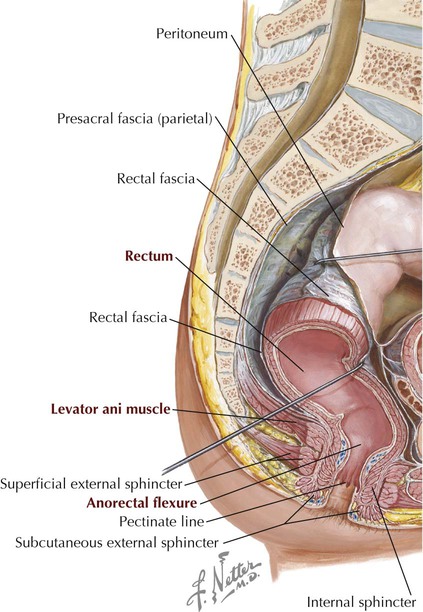
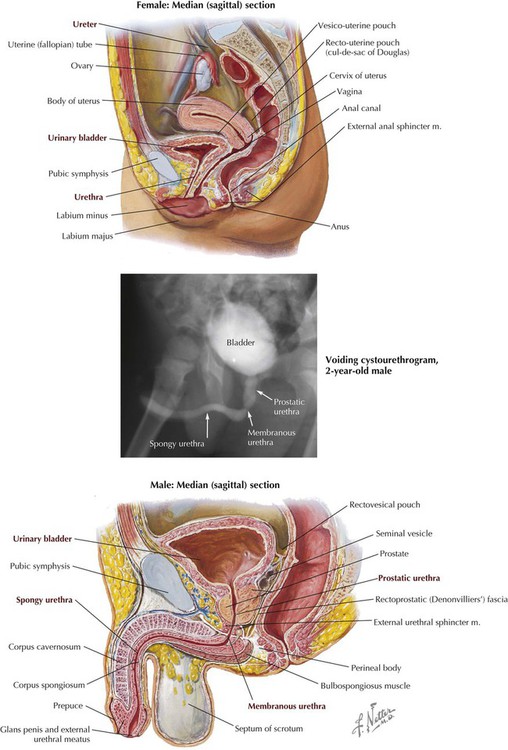
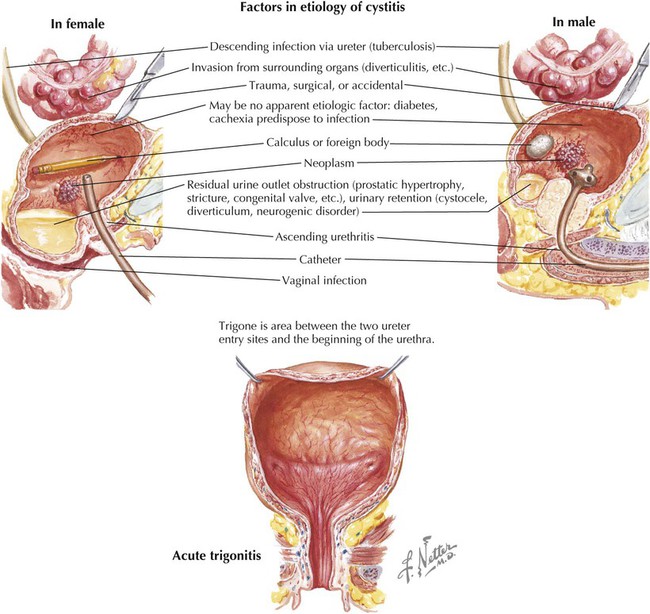
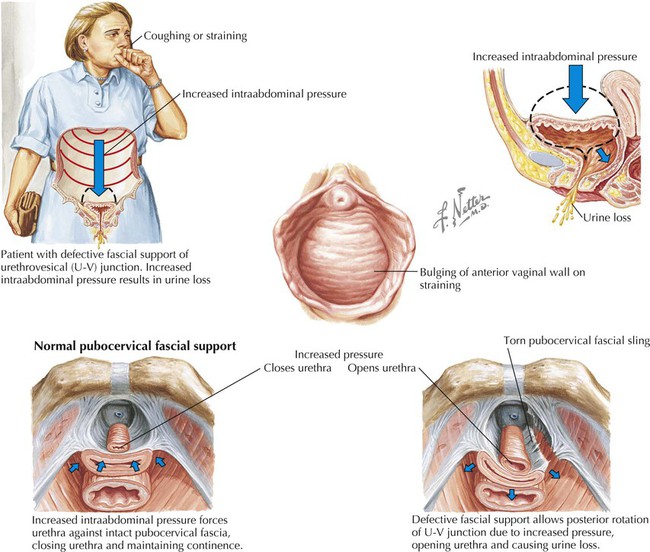
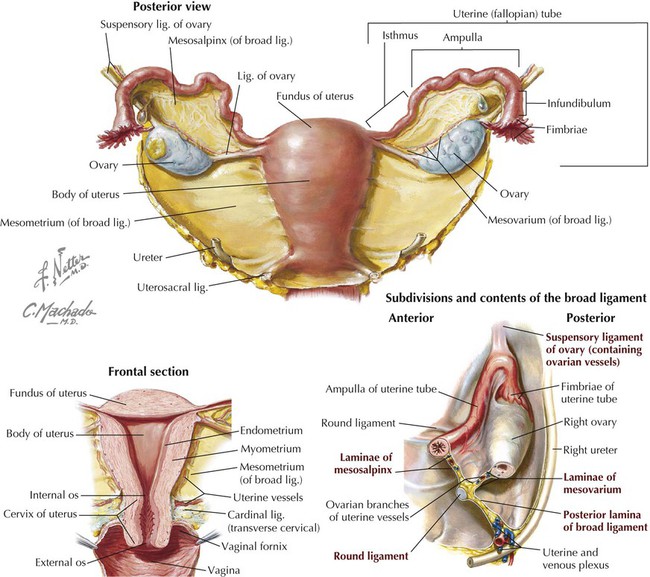
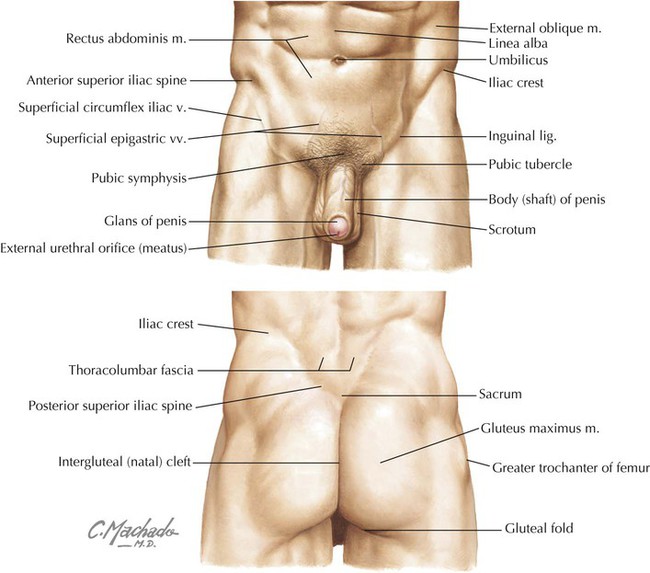
Key landmarks of the surface anatomy of the pelvis and perineum include the following (Fig. 5-1): • Umbilicus: site that marks the T10 dermatome, that lies at the level of the intervertebral disc between L3 and L4; can lie slightly lower in infants or morbidly obese individuals and higher in late pregnancy. • Iliac crest: rim of the ilium that lies at approximately the L4 level; also the approximate level of the bifurcation of the abdominal aorta into its two common iliac branches. • Anterior superior iliac spine: superior attachment point for the inguinal ligament. • Inguinal ligament: ligament formed by the aponeurosis of the external abdominal oblique muscle; forms a line of demarcation separating the lower abdominopelvic region from the thighs. • Pubic tubercle: the inferior attachment point of the inguinal ligament. • Posterior superior iliac spine: often seen as a “dimpling” of the skin just above the intergluteal (natal) cleft; often more obvious in females. The pelvic girdle is the attachment point of the lower limb to the body’s trunk. (The pectoral girdle is its counterpart for the attachment of the upper limb.) The bones of the pelvis include the following (Fig. 5-2): • Right and left pelvic bones (coxal or hip bones): fusion of three separate bones—the ilium, ischium, and pubis—that join in the acetabulum (cup-shaped surface where pelvis articulates with head of femur). • Sacrum: fusion of the five sacral vertebrae; the two pelvic bones articulate with the sacrum posteriorly. • Coccyx: terminal end of the vertebral column; a remnant of our embryonic tail (see also Table 2-2). The pelvis protects the pelvic viscera, supports the weight of the body, aids in ambulation by swinging side to side in a rotary movement at the lumbosacral articulation, provides for muscle attachments, and provides a bony support for the lower birth canal. The pelvic inlet is the circular opening where the lower abdominal cavity is continuous with the pelvic cavity; the promontory of the sacrum protrudes into this opening and is its posterior midline margin (Fig. 5-3). The pelvic outlet is diamond shaped and bounded by the pubic symphysis anteriorly, the pubic arches, the inferior pubic rami and ischial rami, the sacrotuberous ligament, and the coccyx. The perineum is enclosed by these boundaries and lies below the pelvic floor (see Fig. 5-17). The pelvic girdle forms a stable articulation to support the transfer of weight from the trunk to the lower limb. Weight is transferred from the lumbar vertebral column to the sacrum, across the sacro-iliac joints to the coxal (pelvic or hip) bones, and then to the femur (thigh bone). The joints and ligaments reflect this stability (Fig. 5-3 and Table 5-1). The sacro-iliac ligaments are strong, and the posterior sacro-iliac ligament, posterior to the articular joints, is one of the strongest ligaments in the body and supports its entire weight (see Chapter 2). TABLE 5-1 Joints and Ligaments of the Pelvis *Other ligaments include those binding any two vertebrae and facet joints. • The bones of the female pelvis usually are smaller, lighter, and thinner. • The pelvic inlet is oval in the female and heart shaped in the male. • The female pelvic outlet is larger because of everted ischial tuberosities. • The female pelvic cavity is wider and shallower. • The female pubic arch is larger and wider. • The greater sciatic notch is wider in females. • The female sacrum is shorter and wider. • The obturator foramen is oval or triangular in the female and round in the male. The female pelvis may assume variable shapes, as follows: • Gynecoid: normal, and most common form in Caucasian women. • Android: a masculine pelvic type. • Platypelloid: foreshortened in the anteroposterior dimension and wider in the transverse dimension. • Anthropoid: resembling the pelvis of an anthropoid ape, with a greatly elongated anteroposterior dimension and a shortened transverse dimension. The muscles of the true pelvis line its lateral wall and form a floor over the pelvic outlet. (The pelvic inlet is demarcated by the pelvic brim.) Two muscles line the lateral wall (obturator internus and piriformis) and attach to the femur (see Table 6-5), and two muscles form the floor, or pelvic diaphragm (levator ani and coccygeus) (Fig. 5-4 and Table 5-2). The levator ani muscle consists of three muscle groups intermingled to form a single sheet of muscle (iliococcygeus, pubococcygeus, and puborectalis). The levator ani muscle is an important support structure for the pelvic viscera in bipeds (upright-walking humans) and helps maintain closure of the vagina and rectum. Bipedalism places greater pressure on the lower pelvic floor, and the coccygeus and levator ani muscles have been “co-opted” for a different use than originally intended in most land-dwelling quadruped mammals. Thus, the muscles once used to tuck the tail between the hind legs (coccygeus) and wag the tail (levator ani) now subserve a support function as we have evolved as bipeds and have lost our tail. TABLE 5-2 In both genders the distal gastrointestinal tract passes into the pelvis as the rectum and anal canal. The rectosigmoid junction superiorly lies at about the level of the S3 vertebra, and the rectum extends inferiorly to become the anal canal just below the coccyx (Fig. 5-5). As the rectum passes through the pelvic diaphragm, it bends posteriorly at the anorectal flexure and becomes the anal canal. The anorectal flexure helps maintain fecal continence through the muscle tone maintained by the puborectalis portion of the levator ani muscle. During defecation this flexure straightens, and fecal matter can then move into the anal canal. Superiorly, the rectum is covered on its anterolateral surface with peritoneum, which gradually covers only the anterior surface, while the distal portion of the rectum descends below the peritoneal cavity (subperitoneal) to the anorectal flexure. Features of the rectum and anal canal are summarized in Table 5-3. TABLE 5-3 Features of the Rectum and Anal Canal The distal elements of the urinary tract lie within the pelvis and include the following (Fig. 5-6): • Distal ureters: pass retroperitoneally into the pelvic inlet and are crossed anteriorly by the uterine artery in females and the ductus deferens in males before terminating in the urinary bladder. The ureter enters the bladder and passes obliquely through the smooth muscle wall; this arrangement provides for a sphincter-like action. • Urinary bladder: lies behind the pubic symphysis in a subperitoneal position; holds up to 800 mL of urine (less in women and even less during pregnancy), and contains a smooth triangular area internally between the openings of the two ureters and the single urethral opening inferiorly, the trigone of the bladder. The smooth muscle of the bladder wall is the detrusor muscle. • Urethra: short in the female (3-4 cm) and contains two small para-urethral mucous glands (Skene’s glands) at its aperture; longer in the male (20 cm) and divided into the prostatic, membranous, and spongy portions. The prostatic portion (about 3 cm) traverses the prostate gland, the membranous portion (2 cm) traverses the external urethral sphincter (skeletal muscle), and the spongy portion (15 cm) traverses the corpus spongiosum on the ventral aspect of the penis. • Internal sphincter: smooth-muscle involuntary sphincter at the neck of the bladder and innervated by sympathetic fibers from L1 to L2; during ejaculation, it contracts and prevents semen from entering the urinary bladder. • External sphincter: skeletal muscle voluntary sphincter surrounding the membranous urethra and innervated by the somatic nerve fibers in the pudendal nerve (S2-S4). Micturition (urination/voiding) occurs by the following sequence of events: • Normally, the sympathetic fibers relax the bladder wall and constrict the internal urethral sphincter (smooth muscle around the bladder neck, present only in males), thus inhibiting emptying. • Micturition is initiated by the stimulation of stretch receptors (afferents enter the spinal cord via the pelvic splanchnic nerves, S2-S4) located in the detrusor (smooth) muscle of the bladder when it begins to fill. • Parasympathetic efferents (pelvic splanchnics) induce a reflex contraction of the detrusor muscle and relaxation of the internal sphincter (males only), enhancing the urge to void. • When appropriate (and sometimes not!), somatic efferents via the pudendal nerve (S2-S4) cause voluntary relaxation of the external urethral sphincter, and the bladder begins to empty. • When complete, the external urethral sphincter contracts (in males the bulbospongiosus muscle contracts to expel the last few drops of urine from the spongy urethra), and the detrusor muscle relaxes under sympathetic control. The uterus is pear shaped, about 7 to 8 cm long, and exhibits a body (fundus and isthmus) and cervix. While the uterine cavity looks triangular in coronal section (see Fig. 5-8), in sagittal section it appears only as a thin slit (Fig. 5-6, top). The normal position of the uterus is in an anteflexed (anteverted) position and lies almost in the horizontal plane. A double sheet of peritoneum (actually a mesentery) called the broad ligament envelops the ovaries, uterine tubes, and uterus (Figs. 5-7 and 5-8). During embryonic development the ovaries are pulled into the pelvis by a fibromuscular band (homologue of the male gubernaculum). This ovarian ligament attaches the inferomedial pole of the ovary to the uterus, then reflects anterolaterally off the uterus as the round ligament of the uterus, enters the deep inguinal ring, courses down the inguinal canal, and ends in the labia majora of the perineum as a fibrofatty mass. Features of the female pelvic reproductive viscera are summarized in Table 5-4. TABLE 5-4 Features of the Female Pelvic Viscera • Infundibulum: fimbriated, expanded distal portion that opens at the ostium into the peritoneal cavity and lies close to the ovary. • Ampulla: wide portion of the tube lying between the infundibulum and the isthmus; the usual site of fertilization. • Isthmus: proximal, narrow, straight, and thickened portion of the tube that joins the body of the uterus. • Intramural portion: traverses the uterine wall to open into the uterine cavity. The male pelvic reproductive viscera include the prostate gland and paired seminal vesicles. These structures lie in a subperitoneal position and are in close association with the urethra (Fig. 5-9). The testes descend into the scrotum late in human prenatal development and are connected to the seminal vesicles by the ductus (vas) deferens
Pelvis and Perineum
2 Surface Anatomy
3 Musculoskeletal Elements
Bony Pelvic Girdle
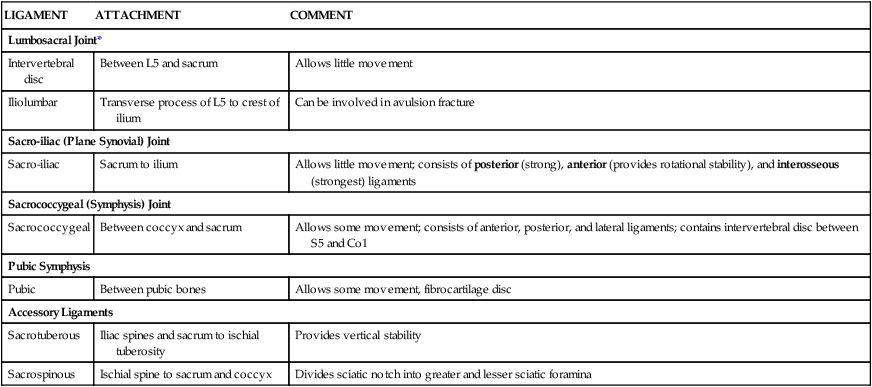
LIGAMENT
ATTACHMENT
COMMENT
Lumbosacral Joint*
Intervertebral disc
Between L5 and sacrum
Allows little movement
Iliolumbar
Transverse process of L5 to crest of ilium
Can be involved in avulsion fracture
Sacro-iliac (Plane Synovial) Joint
Sacro-iliac
Sacrum to ilium
Allows little movement; consists of posterior (strong), anterior (provides rotational stability), and interosseous (strongest) ligaments
Sacrococcygeal (Symphysis) Joint
Sacrococcygeal
Between coccyx and sacrum
Allows some movement; consists of anterior, posterior, and lateral ligaments; contains intervertebral disc between S5 and Co1
Pubic Symphysis
Pubic
Between pubic bones
Allows some movement, fibrocartilage disc
Accessory Ligaments
Sacrotuberous
Iliac spines and sacrum to ischial tuberosity
Provides vertical stability
Sacrospinous
Ischial spine to sacrum and coccyx
Divides sciatic notch into greater and lesser sciatic foramina
Muscles of the Pelvis
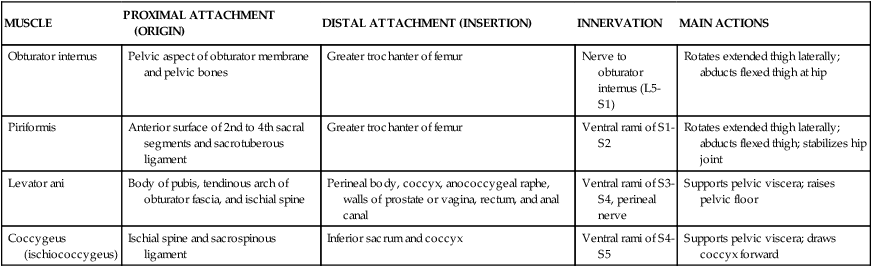
MUSCLE
PROXIMAL ATTACHMENT (ORIGIN)
DISTAL ATTACHMENT (INSERTION)
INNERVATION
MAIN ACTIONS
Obturator internus
Pelvic aspect of obturator membrane and pelvic bones
Greater trochanter of femur
Nerve to obturator internus (L5-S1)
Rotates extended thigh laterally; abducts flexed thigh at hip
Piriformis
Anterior surface of 2nd to 4th sacral segments and sacrotuberous ligament
Greater trochanter of femur
Ventral rami of S1-S2
Rotates extended thigh laterally; abducts flexed thigh; stabilizes hip joint
Levator ani
Body of pubis, tendinous arch of obturator fascia, and ischial spine
Perineal body, coccyx, anococcygeal raphe, walls of prostate or vagina, rectum, and anal canal
Ventral rami of S3-S4, perineal nerve
Supports pelvic viscera; raises pelvic floor
Coccygeus (ischiococcygeus)
Ischial spine and sacrospinous ligament
Inferior sacrum and coccyx
Ventral rami of S4-S5
Supports pelvic viscera; draws coccyx forward
4 Viscera
Distal Gastrointestinal Tract
STRUCTURE
CHARACTERISTICS
Pelvic diaphragm
Consists of levator ani and coccygeus muscles; supports pelvic viscera
Internal sphincter
Smooth muscle anal sphincter
Pectinate line
Demarcates visceral (above) from somatic (below) portions of anal canal by type of epithelium, innervation, and embryology
External sphincter
Skeletal muscle sphincter (subcutaneous, superficial, and deep)
Distal Urinary Tract
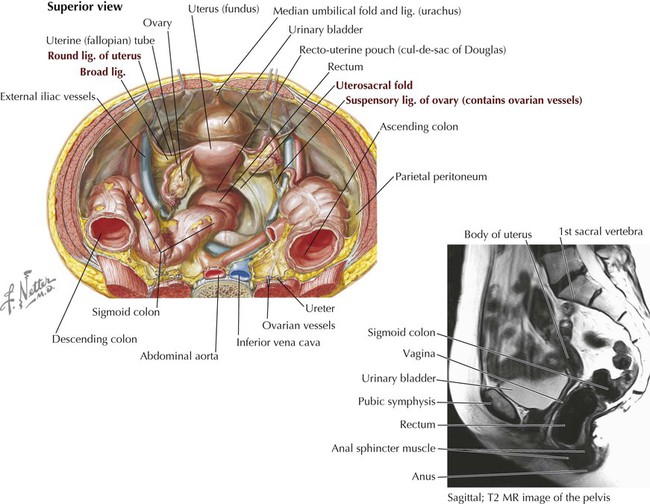
Female Pelvic Reproductive Viscera
STRUCTURE
CHARACTERISTICS
Urinary bladder
Covered by peritoneum
Uterus
Consists of a body (fundus and isthmus) and cervix; supported by pelvic diaphragm and ligaments; enveloped in broad ligament
Ovaries
Suspended between suspensory ligament of ovary (contains ovarian vessels, nerves, and lymphatics) and ovarian ligament (tethered to uterus)
Uterine tubes (fallopian tubes)
Courses in mesosalpinx of broad ligament and consists of fimbriated end (collects ovulated ova), infundibulum, ampulla, isthmus, and intrauterine portions
Vagina
Fibromuscular tube that includes the fornix, a superior recess around protruding uterine cervix
Rectum
Distal retroperitoneal portion of large intestine
Vesico-uterine pouch
Peritoneal recess between bladder and uterus
Recto-uterine pouch (of Douglas)
Peritoneal recess between rectum and uterus and lowest point in female pelvis
Broad ligament
Peritoneal fold that suspends uterus and uterine tubes; includes mesovarium (enfolds ovary), mesosalpinx (enfolds uterine tube), and mesometrium (remainder of ligament)
Round ligament of uterus
Reflects off uterus and keeps uterus anteverted and anteflexed; passes into inguinal canal and ends as fibrofatty mass in labia majora
Transverse cervical (cardinal or Mackenrodt’s) ligaments
Fibrous condensations of subperitoneal pelvic fascia that support uterus
Uterosacral ligaments
Extend from sides of cervix to sacrum, support uterus, and lie beneath peritoneum (form uterosacral fold)
Male Pelvic Reproductive Viscera
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Pelvis and Perineum