Pediatric Pathology
CARDIOVASCULAR
What are the characteristics of Tetralogy of Fallot (TOF)?
Pulmonary valve stenosis; Right ventricular hypertrophy; Overriding aorta; Ventricular septal defect (VSD)
*You have to PROVe TOF with an echo
What is the treatment for TOF?
Surgical repair
How does the anatomy differ from normal in transposition of the great arteries (TGA)?
The aorta arises anteriorly from the right ventricle, while the pulmonary artery (PA) arises from the left ventricle. The aorta is posterior to the PA in a normal heart. This condition may also be referred to as transposition of the great vessels (TGV) by some sources.
Is TGA compatible with life?
No, unless there is a shunt (patent ductus arteriosus [PDA], VSD, patent foramen ovale [PFO], etc) present to allow mixing of the blood
What are the five congenital heart diseases that cause cyanosis (right-to-left shunt) early in postnatal life?
- Truncus arteriosus
- TGA
- Tri cuspid atresia
- Tetralogy of Fallot
- Total anomalous pulmonary venous connection (five words)
*5Ts—count them out on your hand
Why does right-to-left shunting cause cyanosis?
Right-to-left shunting means that deoxygenated blood from the right side of the heart passes into the left side of the heart and is pumped to the systemic circulation. This bypasses the lungs, resulting in circulation of deoxygenated blood which does not meet the oxygen demand of peripheral tissues, resulting in cyanosis.
What is the murmur associated with a patent ductus arteriosus (PDA)?
Continuous machinery-like murmur
At birth, what is used to close a PDA?
Indomethacin
What is used to keep a PDA open?
Prostaglandin E (PGE)
What is the most common congenital cardiac anomaly?
VSD
What are the different types of VSD?
Membranous (most common); infundibular; muscular (multiple: Swiss-cheese septum)
What are the three congenital heart diseases that cause a left-to-right shunt and late cyanosis?
- PDA
- VSD
- Atrial septal defect (ASD)
*All are three-letter acronyms containing a D
Why does late cyanosis occur?
With persistent left-to-right shunting, pulmonary resistance increases, leading to pulmonary hypertension. Eventually a left-to-right shunt becomes a right-to-left shunt, causing cyanosis.
What is the name for the situation when a left-to-right shunt becomes a right-to-left shunt?
Eisenmenger syndrome
What are the different types of ASDs?
Primum (septum primum fails to fuse with endocardial cushions); Secundum (most common due to inadequate development of the septum secundum)
What are endocardial cushion defects?
A spectrum of malformations including VSD, foramen primum, cleft anterior leaflet of the mitral valve, and atrioventricular canal defects
What cardiac defect is associated with Turner syndrome?
Coarctation of the aorta
What are the two types of coarctation of the aorta?
- Infantile type—aortic stenosis is proximal to the insertion of the ductus arteriosus (DA)
- Adult type—aortic stenosis is distal to the insertion of DA
What are the clinical and radiographic characteristics of coarctation of the aorta?
Higher blood pressure in the upper extremities when compared to the lower; notching of the ribs
RESPIRATORY
What are the risk factors for infantile respiratory distress syndrome (IRDS)?
Prematurity, male gender, maternal diabetes, and delivery by cesarean section
What is the etiology of IRDS?
Insufficient pulmonary surfactant
What does the chest x-ray of an infant with RDS show?
Uniform, minute reticulogranular densities producing a diffuse “ground-glass” appearance
What are the microscopic features of RDS?
Collapsed air spaces, expanded respiratory bronchioles, and alveolar ducts lined by eosinophilic hyaline membranes
What is the treatment of IRDS?
Surfactant replacement therapy and oxygen
What is the treatment given to the mother to prevent IRDS?
Steroids (glucocorticoids)
What is the classic presentation of cystic fibrosis (CF)?
History of meconium ileus; recurrent sinusitis, bronchitis; foul smelling stools
How is the diagnosis of cystic fibrosis confirmed?
Sweat test shows increased sweat chloride concentration
What is the genetic defect in cystic fibrosis?
Autosomal recessive mutation of the cystic fibrosis transmembrane conductance regulator (CFTR) gene on chromosome 7
What is the pathogenesis of cystic fibrosis?
The defective chloride channel causes secretion of abnormally viscid mucus that plugs the liver, pancreas, and lungs. This leads to impaired food digestion and absorption and increased susceptibility to pulmonary infections leading ultimately to chronic infection and subsequent respiratory failure.
What organisms infect and may subsequently colonize the lungs of individuals with cystic fibrosis?
Pseudomonas aeruginosa; Staphylococcus aureus; Hemophilus influenza; Burkholderia cepacia
What is the treatment for cystic fibrosis?
There is no curative treatment. Symptomatic treatment with N-acetylcysteine can loosen mucous plugs. Antimicrobials are given for pulmonary infections. Ultimately, lung transplant may be necessary. Pancreatic enzyme replacement is also typically needed.
What clinical feature of cystic fibrosis is unique in males?
Congenital bilateral absence of the vas deferens, azoospermia, and infertility
What is the number one cause of death in infants age 1 month to 1 year?
Sudden infant death syndrome (SIDS)
What preventative measure has been shown to reduce the incidence of SIDS?
“Back to bed”
GASTROINTESTINAL
What congenital malformation typically presents with immediate regurgitation upon feeding?
Tracheoesophageal fistula (TEF)
What are the defects associated with tracheoesophageal fistula?
Vertebral; Anal; Cardiac; Tracheal; Esophageal; Renal; Limb
*The VACTERL anomalies
What is the most common type of tracheoesophageal fistula?
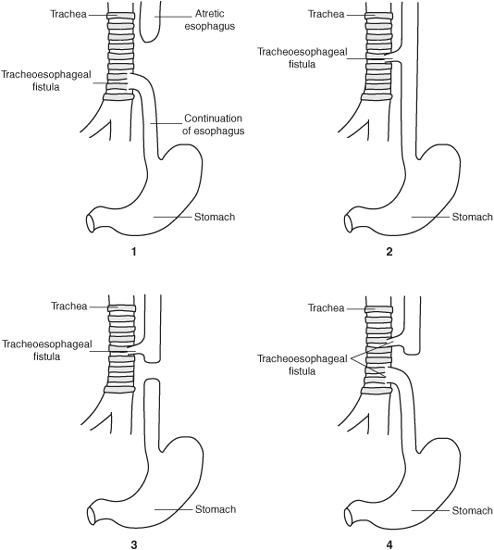
˜85% of cases are a blind upper esophageal atresia with a distal fistula between the lower esophagus and trachea (Type C).
Figure 15.1 Types of tracheoesophageal fistulas. 1. Type C—esophageal atresia with distal TEF, most common type, ˜85% of cases. 2. H type—TEF without atresia, about ˜5% of cases. 3. Type B—esophageal atresia with proximal TEF. 4. Type D—esophageal atresia with both proximal and distal TEF. (Type A is not shown, but is esophageal atresia without TEF.)
How does pyloric stenosis typically present?
Projectile, nonbilious vomiting in a 2- to 4-week-old, classically firstborn male, infant
What is the pathogenesis of pyloric stenosis?
Hypertrophy and possibly hyperplasia of the muscularis propria in the pylorus. Inflammation and edema may also contribute to further narrowing of the pyloric outlet.
What is the treatment of pyloric stenosis?
Pyloromyotomy (surgical muscle splitting)
What malformation is associated with projectile, bilious vomiting, and bloating in a new born?
Annular pancreas
How does an annular pancreas form?
A band of pancreatic tissue (from a bifid ventral pancreatic bud) surrounds the duodenum
What congenital malformation is associated with Down syndrome and presents with bilious emesis within the first day of life?
Duodenal atresia
What is the radiographic finding/sign associated with duodenal atresia?
The double bubble sign (air bubbles in the stomach and duodenum)
What is the treatment for duodenal atresia?
Surgical repair
What is a Meckel diverticulum?
Persistence of the vitelline duct, which connects the developing gut to the yolk sac
What are the characteristics of Meckel diverticulum?
- 2% of the general population have a Meckel diverticulum
- 2% of Meckel diverticula are symptomatic
- Symptoms occur in patients 2 years old or younger, typically
- They arise 2 ft from the ileocecal valve
- They are 2 in (3-5 cm) in length
- There are 2 types of commonly associated ectopic tissue—gastric and pancreatic
*Follow the rule of 2s and try not 2 miss it!
What is the classic presentation of intussusception?
Severe episodic abdominal pain, often patients will curl into the fetal position, sometimes accompanied by nausea, vomiting, and bloody stools
What is the pathophysiology of intussusception?
Proximal portion of the gastrointestinal (GI) tract telescopes into the adjacent portion; proximal portion, or leading point, may be a Meckel diverticulum, polyp, or tumor
What is the treatment for an intussusception?
Air contrast enema to increase intraluminal pressure and facilitate reduction of the intussusception
What are the clinical characteristics of Hirschsprung disease?
Delayed passage of meconium, constipation, and abdominal distention
What is the next step in diagnosis?
Rectal biopsy showing lack of ganglion cells is confirmatory.
The biopsy of the intestine reveals a lack of ganglion cells (in Auerbach and Meissner plexuses) in the muscle wall. What is the mechanism of this defect?
Failure of neural crest cell migration. These neural crest cells eventually become ganglion cells.
What is the treatment of Hirschsprung disease?
Colostomy prior to corrective surgery allows for pelvic growth and normalization of dilated bowel.
An infant is born with the abdominal contents outside the body, yet contained in a midline sac of peritoneum. What is the diagnosis?
Omphalocele
*The “O” reminds you of the belly button which is midline and covered (by skin)
What other abnormalities are associated with omphalocele?
GI and cardiac defects
An infant is born with the abdominal contents outside of the body lateral to the umbilicus and not covered by peritoneum. What is the most likely diagnosis?
Gastroschisis
What are the classic features of appendicitis?
Right lower quadrant abdominal pain (often initially periumbilical), fever, vomiting
What is the treatment of appendicitis?
Appendectomy
Which side of the body is more common for a congenital diaphragmatic hernia?
Left
What is the pathogenesis of congenital diaphragmatic hernia?
Abnormal formation of one of the pleuroperitoneal membranes or a defect in the fusion of pleuroperitoneal membrane with the septum transversum and mesentery of the esophagus
What is the treatment of congenital diaphragmatic hernia?
Surgical repair
What is the most common complication/cause of death in congenital diaphragmatic hernia?
Respiratory distress secondary to pulmonary hypoplasia
What is necrotizing enterocolitis (NEC)?
Severe gastrointestinal disease of neonates of currently unclear etiology that is characterized by necrosis of the mucosa of the intestine. Premature infants are at particularly high risk of developing NEC.
MUSCULOSKELETAL
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree