CHAPTER 25 After reviewing this chapter, you should be able to: 1. Convert body weight from pounds to kilograms 2. Convert body weight from kilograms to pounds 3. Calculate dosages based on milligram per kilogram 4. Determine whether a dosage is safe 5. Determine body surface area (BSA) using the West nomogram 6. Calculate BSA using formulas according to units of measure 7. Determine dosages using the BSA 8. Calculate the flow rates for pediatric IV therapy 9. Calculate the safe dosage ranges and determine if within normal range for medications administered IV in pediatrics • Confusion between adult and pediatric formulations • Errors with oral liquid dosage forms that are available in multiple pediatric concentrations • Incorrect preparation of medications that require dilution • Look-alike packaging and look-alike and sound-alike names • Improper education of parents regarding preparation of medications and administration • Inaccurate measuring devices (use of household teaspoons) as opposed to devices such as oral dosing devices for small volume doses The two methods currently being used to calculate pediatric dosages are as follows: Before calculating medications for the child or infant, some guidelines are helpful to know. 1. Calculation of pediatric dosages, as with adult dosages, involves the use of ratio and proportion, the formula method, or dimensional analysis to determine the amount of medication to administer. 2. Pediatric dosages are much smaller than those for an adult. Micrograms are used a great deal. The tuberculin syringe (1-mL capacity) is used to administer very small dosages. 3. Intramuscular (IM) dosages are usually not more than 1 mL for small children and older infants; however, this can vary with the size of the child. The recommended IM dosage for small infants is not more than 0.5 mL. 4. The recommended subcutaneous (subcut) dosage for children is not more than 0.5 mL. 5. Dosages that are less than 1 mL may be measured in tenths of a milliliter, or with a tuberculin syringe in hundredths of a milliliter. 6. Medications in pediatrics generally are not rounded off to the nearest tenth but may be administered with a tuberculin syringe (measured in hundredths) to ensure accuracy. Therefore the most common conversion you will encounter involves the conversion from pounds to kilograms. To do this, remember the conversion 1 kg = 2.2 lb. Conversions of weights are presented in Chapter 9. The methods of converting presented in Chapter 8 can also be used. It is, however, essential that we review this again. 1. Calculation of the total daily dosage 2. Division of the daily dosage by the number of dosages to be administered 3. Use ratio and proportion, the formula method, or dimensional analysis to calculate the number of tablets or capsules or the volume to give to administer the ordered dosage Before beginning to calculate dosages based on weight, let’s review some concepts that may be used. Recommended dosage (also referred to as the safe dosage)—This information comes from a reputable resource, such as a medication reference written especially for pediatrics or another medication reference book. Recommended dosages may also be indicated on the medication label under children’s dosages. This is usually expressed in mg/kg for a 24-hour period to be given in one or more divided doses. This may also be seen as mcg/kg and occasionally mg/lb. Recommended dosage can also be stated as a range and referred to as safe dosage range (SDR). This is the upper and lower limits of the dosage as stated by an approved medication reference. Total daily dosage—Dosage obtained by multiplying the child’s weight after it is converted to kilograms with the use of a reputable medication reference: multiply child’s weight in kilograms by dosage expressed as mg/kg. Divided dosage—This represents the dosage a child should receive each time the medication is administered. The recommended daily dosage may be stated as mg/kg/day to be divided into a certain number of individual dosages, such as “three divided dosages,” q6h, and so on. “Three divided dosages” means that the total daily dosage is divided equally and administered three times per day. q6h means the total daily dosage is divided equally and administered every 6 hours, for a total of four dosages per day (24 hr ÷ 6 hr). This is the dosage for 24 hours divided by the frequency, or the number of times, the child will receive the medication. Deciding if the dosage is safe—This is done by comparing the ordered dosage with the recommended dosage. In other words, this is decided by comparing and evaluating the 24-hour ordered amount with the recommended dosage.
Pediatric and Adult Dosage Calculation Based on Weight
PRINCIPLES RELATING TO BASIC CALCULATIONS
CALCULATION OF DOSAGES BASED ON BODY WEIGHT
CONVERTING GRAMS TO KILOGRAMS
Remember


 Solution Using Ratio and Proportion
Solution Using Ratio and Proportion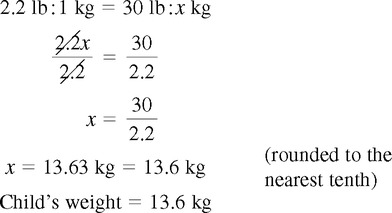
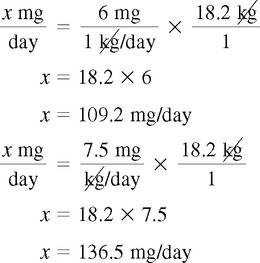
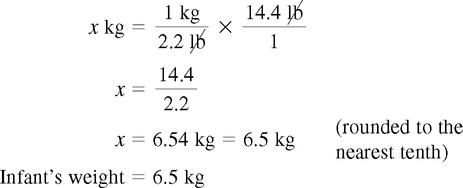
 Solution Using Dimensional Analysis
Solution Using Dimensional Analysis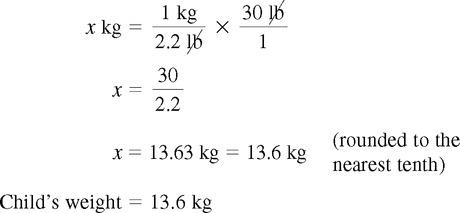

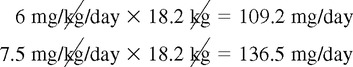
 Solution Using Ratio and Proportion
Solution Using Ratio and Proportion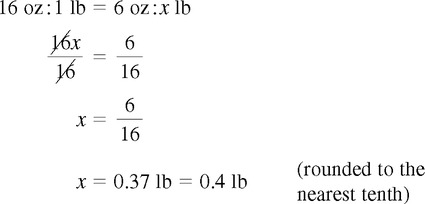
 Solution Using Ratio and Proportion
Solution Using Ratio and Proportion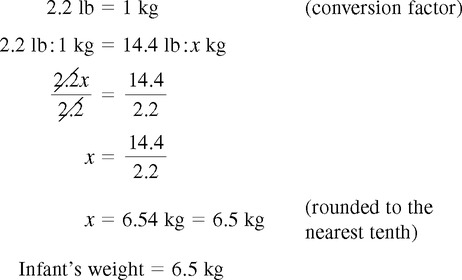
 Solution Using Dimensional Analysis
Solution Using Dimensional Analysis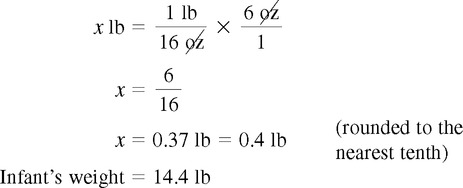

 Solution Using Ratio and Proportion
Solution Using Ratio and Proportion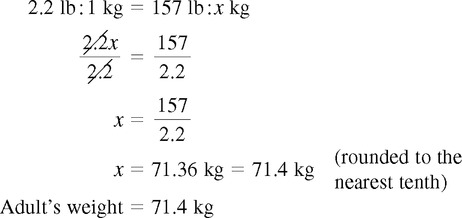
 Solution Using Dimensional Analysis
Solution Using Dimensional Analysis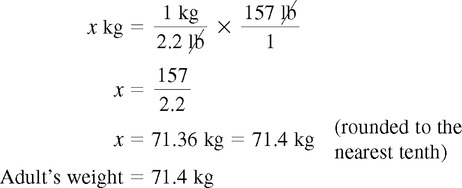
 Practice Problems
Practice Problems
 Solution Using Ratio and Proportion
Solution Using Ratio and Proportion
 Solution Using Dimensional Analysis
Solution Using Dimensional Analysis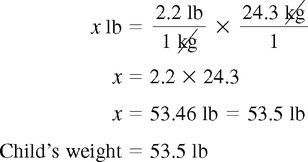

 Solution Using Ratio and Proportion
Solution Using Ratio and Proportion
 Solution Using Dimensional Analysis
Solution Using Dimensional Analysis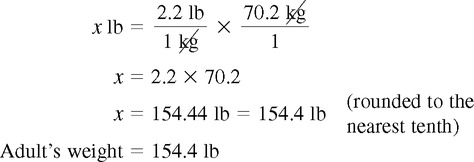

 Solution Using Ratio and Proportion
Solution Using Ratio and Proportion
 Solution Using Dimensional Analysis
Solution Using Dimensional Analysis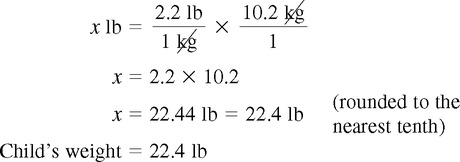
 Practice Problems
Practice Problems
 Solution Using Ratio and Proportion
Solution Using Ratio and Proportion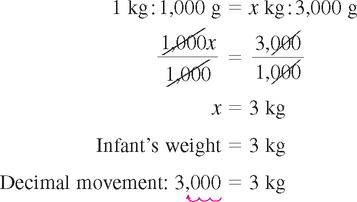
 Solution Using Dimensional Analysis
Solution Using Dimensional Analysis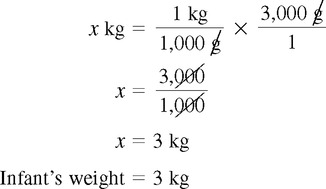

 Solution Using Ratio and Proportion
Solution Using Ratio and Proportion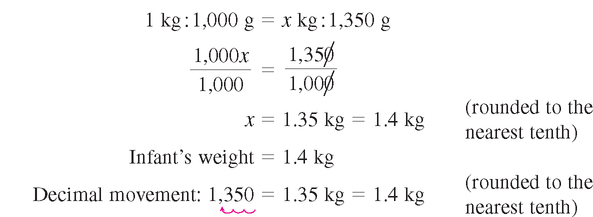
 Solution Using Dimensional Analysis
Solution Using Dimensional Analysis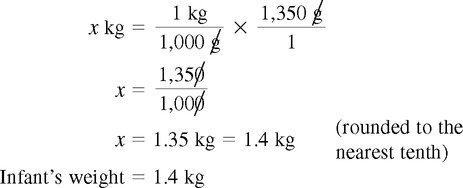

 Solution Using Ratio and Proportion
Solution Using Ratio and Proportion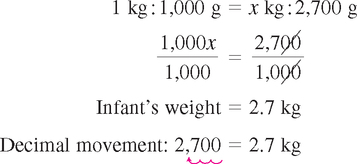
 Solution Using Dimensional Analysis
Solution Using Dimensional Analysis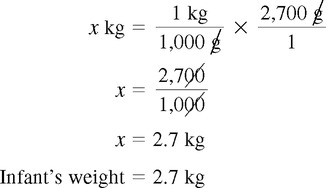
 Practice Problems
Practice Problems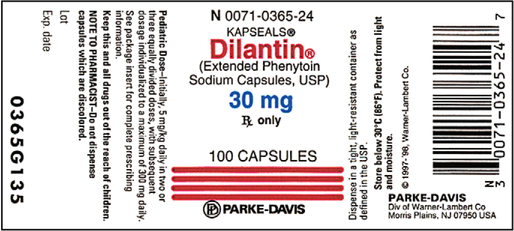
 Solution Using Ratio and Proportion
Solution Using Ratio and Proportion
 Solution Using Dimensional Analysis
Solution Using Dimensional Analysis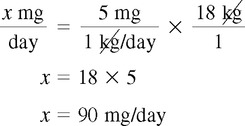
 Solution Using Ratio and Proportion
Solution Using Ratio and Proportion
 Solution Using Formula Method
Solution Using Formula Method
 Solution Using Dimensional Analysis
Solution Using Dimensional Analysis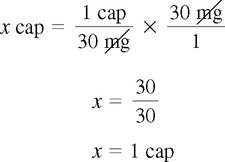
 Solution Using Ratio and Proportion
Solution Using Ratio and Proportion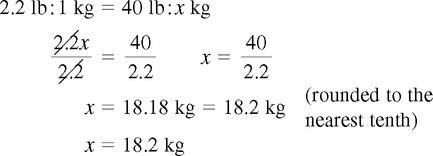
 Solution Using Dimensional Analysis
Solution Using Dimensional Analysis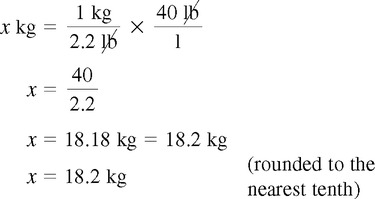
 Solution Using Dimensional Analysis
Solution Using Dimensional Analysis