Introduction
Nutrition, an important element in a neonate’s care, promotes growth and development. When infants are unable to take enteral nutrition or enteral nutrition is contraindicated, parenteral nutrition (PN) is provided. Most times PN is started as soon as intravenous (IV) access is established in the neonate. Early nutrition improves weight gain and decreases growth failure.1,2 PN for neonates is not only used with gastrointestinal (GI) disorders (e.g., gastroschisis, omphaloceles) but also provides nutrition because enteral nutrition is advanced. Many components make up a PN comprised of different macronutrients and micronutrients.
Fluids and Nutrition
Fluid and nutrition management typically go hand in hand. These two components are vital in the day-to-day care of a neonate. As pharmacists we can help track daily fluid input, output, and caloric intake to optimize nutrition support toward ensuring proper weight gain. Pharmacists can be a great resource in fluid and nutrition management of a neonate.
IV Fluid Management
Fluid management in neonates is a major part of nutrition support. It can often be challenging to manage due to different disease states and comorbidities. Neonates are comprised mainly of water and have decreased body fat when compared to children and adolescents.3 On average, neonates lose about 10% of their weight in the first 24 to 48 hours of life due to shifts in fluids and natural diuresis. Term neonates should be back to their birth weight by 1 week of life, although preterm neonates may take 2 or more weeks.
At birth, a neonate requires about 60 to 70 mL/kg/day and increases by 10 to 20 mL/kg/day to goal. An average fluid goal for neonates ranges from 120 to 150 mL/kg/day.4–6 Extremely low birth weight infants may require up to 170 to 180 mL/kg/day due to immaturity of skin and increased fluid losses. When thinking about fluid requirements, pharmacists should take into account sensible and insensible water losses. Insensible water losses include conditions such as prematurity, phototherapy, and tachypnea. Fluids should not be advanced too vigorously in patients with respiratory distress, bronchopulmonary dysplasia (BPD), congenital heart defects, and heart failure as it can worsen their condition.
Nutrition Management
Calorie requirements are higher for preterm neonates than for term neonates. Preterm neonates require about 90 to 120 kcal/kg/day compared to term neonates who require 80 to 100 kcal/kg/day.6 Weights should be monitored daily to ensure proper nutrition and growth. Term neonates on average should gain 15 to 30 g/day. Preterm infant weight gain is measured in terms of g/kg/day. They should regain their birth weight by day of life 14; then, the goal average weight gain per week is 15 to 18 g/kg/day until they reach 2 kg. After preterm infants reach 2 kg, their average weight gain per week is 25 to 35 g/day. Growth in neonates may fluctuate depending on severity of current illnesses and nutrition status. The World Health Organization and the Fenton growth charts are used to assess growth in preterm and term infants.
Macronutrients
Carbohydrates
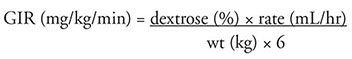
Dextrose is a major component in a neonate PN. It should provide 40 to 50% of total calories from the PN. Dextrose concentration typically ranges from 10 to 15%. Specific patient populations such as infants of diabetic mothers may require higher dextrose concentration and glucose infusion rates (GIR), which are important in starting and advancing PN. Normal starting GIR is 3 to 5 mg/kg/hr and is advanced by 2 to 3 mg/kg/hr to a maximum of 10 to 12 mg/kg/hr. When advancing dextrose and IV fluid rates, pharmacists should remember that both affect GIR. In some instances if both dextrose and IV fluid goals are increased at the same time, this may increase GIR by more than 2 to 3 mg/kg/hr. Every 1 gram of dextrose provides 3.4 kcal. Blood glucose is monitored for hypo- and hyperglycemia.
Excessive increase in glucose load can cause hyperglycemia, excessive carbon dioxide, and potential liver damage. Blood glucose levels of greater than 150 mg/mL are associated with adverse outcomes in neonates. Hyperglycemia increases the risk of intraventricular hemorrhage (IVH), necrotizing enterocolitis, and infections and is associated with prolonged hospital stays. To manage hyperglycemia, either the dextrose concentration or the IV fluid rate should be adjusted, resulting in a change in GIR to prevent further complications. Although it may not be feasible or cost effective to change dextrose concentrations of a PN right away, IV fluids with a lower dextrose concentration may be administered via Y-site with the PN. For example, a neonate has a PN containing dextrose 10% currently infusing at a rate of 8 mL/hr and the neonate becomes hyperglycemic after running the D10% PN for 4 hours. To provide a lower dextrose concentration, an IV fluid containing dextrose 5% may be co-administered 1:1 with the D10% PN in the same IV line. This results in the D10% PN running at 4 mL/hr and the D5% IV fluid at 4 mL/hr. This decreases the dextrose concentration to 7.5%, which in turn decreases the GIR.
While decreasing dextrose concentrations, it is also important to make sure GIR does not drop significantly in order to prevent hypoglycemia. Insulin therapy may be warranted for consistent hyperglycemia despite other efforts. Insulin therapy may be used to treat infants with hyperglycemia; however, the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) guidelines do not recommend using insulin to prevent hyperglycemia.8 Other factors can increase blood glucose in neonates that should be considered when initiating or changing dextrose content. Often times, stress from procedures or surgery and medications (e.g., steroids) can cause an increase in blood glucose. These should be taken into consideration when advancing dextrose and fluid goals.
On the flip side, it is also crucial that neonates do not get hypoglycemic (<45 mg/mL). Premature infants and infants of diabetic mothers are at high risk of hypoglycemia. Patients exhibiting signs of hypoglycemia should be treated with increased GIR regardless of blood sugar levels.8
Protein
Initiation of parenteral protein, provided as amino acids (AAs), is crucial to the growth and development of neonates. AAs are initiated at a goal of 3 to 4 g/kg/day depending on the age of the neonate. Protein requirements are highest for the premature neonates, and requirements decrease with increasing age. Early administration with high doses of AAs up to 4 g/kg/day has been shown to improve growth.9–11 Specific types of AA products (e.g., TrophAmine, Premasol, Aminosyn) are made for neonates and provide additional AAs that other formulations do not contain. These products provide arginine, tyrosine, and taurine, which are conditionally essential in neonates. Some AAs such as TrophAmine have a lower pH, which helps with calcium and phosphorus solubility.12 Every 1 gram of AAs provides 4 kcal; however, there is controversy on whether calories from AAs should be counted in the total calorie count.13 Opinions leading toward not including them in the calorie count argue that dextrose and fats are for energy and that AAs are for protein synthesis.14 Blood urea nitrogen and renal function are monitored.
Fat Emulsions
Intravenous fat emulsions (IVFEs) provide a major concentrated source of calories. The majority of fat emulsions provided to neonates are soy-based, which consist mainly of omega-6 fatty acids. Linoleic and α-linolenic acid are the essential fatty acids that make up fat emulsions. Fats provide 9 kcal for every 1 gram received; however, the emulsifying agents and glycerol in IVFEs increase the calories. IVFEs are available at concentrations of 10%, 20%, and 30%. The 20% concentration is preferred over 10% because of the decreased phospholipids. The 30% concentration is rarely used in neonates because it has to be used only in 3-in-1 PNs.15 IVFE at 20% concentration provides 2 kcal per milliliter. Fat emulsions not only provide calories but also prevent and treat fatty acid deficiency syndrome. Fat emulsions should be initiated at low doses (0.5 to 1 g/kg/day) and titrated up to maximum doses (3 g/kg/day) to prevent hypertriglyceridemia and other complications. Triglycerides should be monitored with any increase in doses and at least once weekly when goal dose is achieved.
Dissimilar to soybean oil, a product called Omegaven consists of omega-3 fatty acids, specifically eicosapentaenoic acid and docosahexaenoic acid. Omegaven has been shown to have benefits when used in patients with PN-associated liver disease (PNALD) also known as intestinal failure-associated liver disease (IFALD). Omegaven is not currently approved in the United States but may be administered for compassionate use. An investigational new drug application is required prior to administering and obtaining Omegaven from the manufacturer, Fresenius Kabi, in Germany. Omegaven works to improve bile flow and interferes with the metabolism of omega-6 fatty acids, which can cause inflammation. Omegaven has been shown to decrease bilirubin levels, slow the rate of liver disease progression, and reverse cholestasis. It is associated with restoration of liver function in patients with short bowel syndrome and advanced liver disease.16–18
Micronutrients
Electrolytes
Electrolytes added to PN include sodium, potassium, calcium, phosphorus, and magnesium. Electrolyte requirements differ between preterm neonates and term neonates as shown in Table 3-1. When assessing the need for electrolytes, pharmacists should consider a patient’s laboratory test results as well as any underlying disease states. For example, patients with renal insufficiency or failure may require less potassium and phosphorus compared to someone with normal renal function. Neonates require a tremendous amount of calcium and phosphorus for bone growth and heart function. The majority of bone mineralization in utero occurs in the third trimester, so this may not happen if the neonate is born prematurely.19 Neonates on short-term PN should receive 76 mg/kg of elemental calcium per day with a calcium-to-phosphorus ratio of 1.7:1 (mg:mg).20 Calcium is available as calcium gluconate or calcium chloride. Calcium gluconate is preferred because it provides less dissociated calcium ions and, therefore, decreases the possibility to precipitate with phosphate ions. Calcium is a vesicant and can cause serious damage if extravasation occurs. Calcium gluconate is less irritating to blood vessels when compared to calcium chloride. In the occurrence of extravasation, hyaluronidase may be used as an antidote around the extravasated area. Acetate and chloride are added in forms of sodium and/or potassium acetate or chloride to PN for acid−base balance.
Role of Trace Elements
Trace elements play an important role in enzyme activity. Trace elements included in neonatal PN are selenium, zinc, copper, chromium, manganese, and molybdenum. Selenium is recommended for use in all patients and is more critical for patients on long-term PN therapy. Selenium deficiency can lead to cardiomyopathy and thyroid dysfunction.21 Zinc is used for growth and promotes wound healing and immune system function. Zinc deficiency can lead to growth restriction, alopecia, and skin rash.22
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


