Paraganglioma (Glomus Jugulare/Tympanicum)
Lester D. R. Thompson, MD
Key Facts
Terminology
Synonyms: Glomus jugulare, glomus tympanicum
Neoplasm arising from paraganglia in vicinity of jugular bulb or medial cochlea promontory
Clinical Issues
10% multicentric, 10% bilateral, 10% familial
Female > > Male (5:1) in sporadic tumors
90% of tumors of jugular foramen are paraganglioma
Pulsatile tinnitus
Hearing loss (conductive)
Do not biopsy: Very vascularized and will bleed
Presurgical embolization for reduced bleeding
15% mortality due to proximity of vital anatomic structures
Image Findings
CT: Bone only without contrast shows a mass with flat base on cochlear promontory
MR T1WI: Multiple black dots in tumor indicate high-velocity flow voids
Octreotide or MIBG scintigraphy helps with occult or familial tumors
Microscopic Pathology
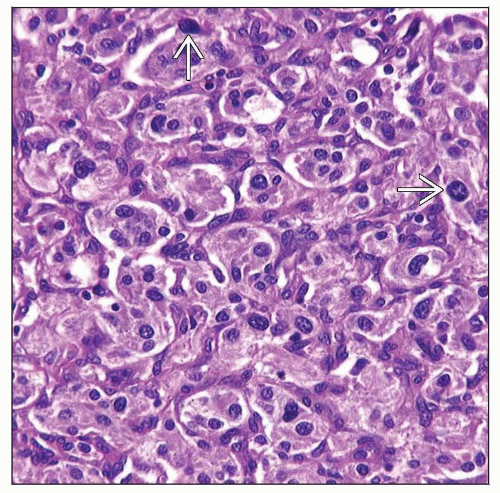
Clustered, zellballen architecture
Richly vascularized stroma, sometimes with fibrosis
Small to intermediate cells with ample granular, basophilic cytoplasm
Ancillary Tests
Neuroendocrine markers
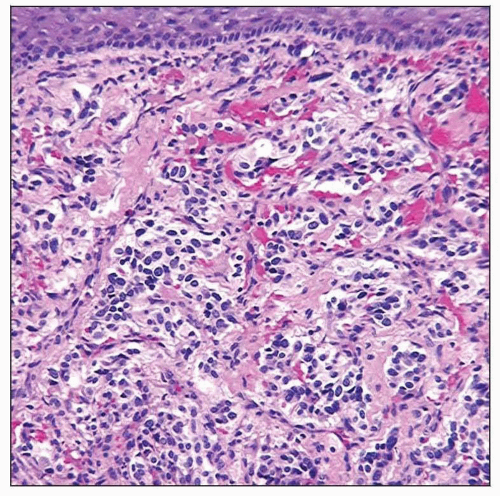 Hematoxylin & eosin shows an intact squamous epithelium (from the EAC) subtended by a nested neoplastic proliferation associated with a rich vascularized network and fibrous connective tissue. |
TERMINOLOGY
Abbreviations
Glomus tympanicum paraganglioma (GTP)
Glomus jugulotympanicum paraganglioma (GJP)
Synonyms
Glomus tympanicum
Glomus jugulotympanicum
Jugulotympanic chemodectoma
Glomus jugulare
Jugular glomus tumor
Tympanic glomus tumor
“Glomus” is usually applied to smooth muscle vascular tumor of nail bed soft tissue
Definitions
Neoplasm arising from paraganglia in vicinity of jugular bulb or medial cochlea promontory
Radiographically and surgically “glomus tympanicum” (GTP) and “glomus jugulotympanicum” (GJP) paragangliomas are distinctive and unique
However, they are identical by pathology parameters; these clinical terms will be used for nonpathology findings
ETIOLOGY/PATHOGENESIS
Cell of Origin
Arises from paraganglia
Along inferior tympanic nerve (Jacobson nerve)
Around jugular foramen
Auricular branch of CNX (Arnold nerve)
Chemoreceptor cells are derived from neural crest
Respond to changes in blood oxygen and carbon dioxide levels
CLINICAL ISSUES
Epidemiology
Incidence
Most common tumor of middle ear (GTP)
Most common tumor of jugular foramen (GJP) (˜ 90%)
Together GTP and GJP account for 80% of head and neck paragangliomas
10% multicentric
10% bilateral
10% familial
10% pediatric
10% malignant
May coexist with pheochromocytoma (adrenal gland) and carotid body tumors
Age
Range: 10-85 years
Mean: 6th decade
Gender
Female > > Male (5:1) for sporadic tumors
Male > Female for inherited/familial tumors
Site
GTP: Middle ear surface of promontory
Anterior inferior quadrant of tympanic membrane
GJP: Jugular foramen
Wall of jugular bulb
Presentation
Pulsatile tinnitus (˜ 90% of patients)
Hearing loss (˜ 50% of patients)
Conductive rather than sensorineural
Vascular retrotympanic mass
Pain
Facial nerve paralysis
Catecholamine function is rare
If familial or syndrome: Autosomal dominant trait with genomic imprinting
Treatment
Options, risks, complications
Do not biopsy; very vascularized and will bleed
Slow growing but locally destructive tumor
Can be “watched” in older patients
Presurgical embolization for reduced bleeding
About 2/3 of patients experience postoperative cranial neuropathy
Surgical approaches
GTP
Tympanotomy for small lesions
Mastoidectomy for larger lesions
GJP
Infratemporal fossa approach (Fisch type A)
Radiation
May work for localized tumors
May be needed in combination with surgery for larger tumors
Palliative in poor surgical candidates or older patients
Prognosis
Excellent overall outcome
Aggressive clinical behavior is seen in ˜ 8-10% of cases
15% mortality due to proximity of vital anatomic structures
Distant metastases are rare
IMAGE FINDINGS
General Features
Radiographs accurately define location, size, extent
Glomus tympanicum
CT: Bone only without contrast shows a mass with flat base on cochlear promontory
MR: Enhancing mass with flat base on cochlear promontory
Performed after bone CT yields suspicious result
Glomus jugulare
CT: Bone only shows a mass in jugular foramen with permeative-destructive change in adjacent bone
MR T1WI: Multiple black dots in tumor indicate high-velocity flow voids from feeder arterial branches
Angiography: Allows for preoperative embolization
Demonstrates blood supply from ascending pharyngeal artery and its branches
Octreotide or MIBG scintigraphy helps with occult or familial tumors
PET with F18 FDG: Avid uptake by tumor cells
MACROSCOPIC FEATURES
General Features
Fragmented due to anatomic restrictions
Irregular, reddish masses
Firm mass
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree