 Overview
Overview
Musculoskeletal pain arises from the muscles, bones, joints, and connective tissue. It can be acute (e.g., acute sport injuries such as tendonitis, sprains, or strains) or chronic (e.g., pain from osteoarthritis). It may be felt in the affected tissue itself or referred from another anatomic source (e.g., hip pain referred from its primary source in the low back).
 Definitions of Common Musculoskeletal Injuries and Disorders
Definitions of Common Musculoskeletal Injuries and Disorders
- Muscle injuries include strains, contusions, and delayed onset muscle soreness (e.g., overexertion).
- Strains are caused by stretching or tearing of a muscle or tendon.
- Contusions represent bruising of a muscle caused by blunt trauma.
- Delayed-onset muscle soreness begins ≥8 hours after repeated, unaccustomed eccentric muscle contraction. The soreness usually peaks at 24–48 hours but can last for days.
- Strains are caused by stretching or tearing of a muscle or tendon.
- A muscle spasm is an involuntary muscle contraction. A muscle cramp is a prolonged muscle spasm that produces painful sensations.
- Tendonitis is inflammation of a tendon resulting from acute injury or chronic overuse (e.g., carpal tunnel syndrome).
- Fluoroquinolone antimicrobial agents are associated with the development of tendonitis or tendon rupture. Patients >60 years of age who are taking steroids or have had heart, lung, or kidney transplantation are at greater risk.
- Bursitis is inflammation of the bursa (the fluid-filled sacs located between joint spaces). Bursitis generally results from an acute injury to the joint or over-repetitive joint action; it is worsened by any movement of the structure adjacent to the bursa.
- Sprains are caused by excessive stretching or partial or complete tearing of a ligament. Sprains commonly occur during physical activity.
- Osteoarthritis is characterized by a gradual softening and destruction of the cartilage between bones. Often referred to as “degenerative joint disease,” osteoarthritis is caused by genetic, metabolic, and environmental factors.
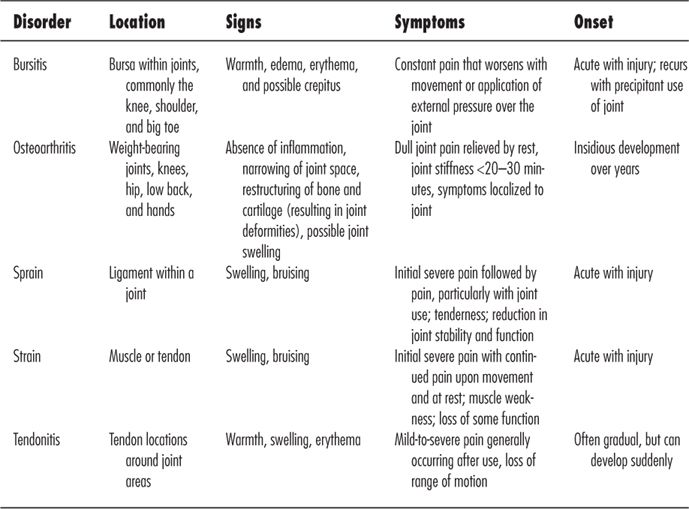
TABLE 1. Comparison of Common Musculoskeletal Disorders
 Signs and Symptoms
Signs and Symptoms
Pain is a common symptom of a number of common musculoskeletal disorders (see Table 1).
 Treatment
Treatment
- Self-treatment of patients presenting with pain secondary to acute musculoskeletal injuries or disorders should be limited to those with mild-to-moderate pain and no exclusions for self-treatment, such as a visibly deformed joint or systemic symptoms.
- Pain associated with osteoarthritis may be self-treated after an initial medical diagnosis.
- Use of a pain scale helps to quantify the intensity of a patient’s pain. With a numerical pain scale, patients rank their pain on a scale of 0–10, with 0 being no pain and 10 being the worst pain the patient can imagine. In general, nonprescription medications are appropriate for numerical rating scale scores of 1–3 and may be appropriate for scores of 4 or 5. Scores ≥6 indicate pain that requires medical referral.
 General/Nonpharmacologic Treatment Measures
General/Nonpharmacologic Treatment Measures
- RICE (rest, ice, compression, elevation) therapy promotes healing and helps reduce swelling and inflammation associated with acute muscle and joint injuries.
- Rest the injured area after injury and continue until pain is reduced (generally 1–2 days). Slings, splints, or crutches can be used if necessary.
- Apply ice to the injured area as soon as possible for periods of 10–15 minutes, three to four times per day. Ice should not be applied for >15 minutes at a time; excessive icing causes considerable vasoconstriction and reduces vascular clearance of inflammatory mediators from the damaged area. Ice therapy may be continued for 1–3 days, depending on the severity of the injury.
- Apply compression to the injured area with an elastic support or an elasticized bandage.
- Elevate the injured area at or above the level of the heart for 2–3 hours per day to decrease swelling and to relieve pain.
- Rest the injured area after injury and continue until pain is reduced (generally 1–2 days). Slings, splints, or crutches can be used if necessary.
- Heat therapy is an alternative for patients who develop pain of a noninflammatory nature (e.g., acute low back pain). Heat is applied for 15–20 minutes, three to four times per day. Heat may be applied in the form of a warm, wet compress; heating pad; hot-water bottle; or heat-generating wrap or adhesive products (e.g., ThermaCare or Precise).
- Heat should not be applied to recently injured (<48 hours) or inflamed areas, because it intensifies vasodilation and can exacerbate vascular leakage and tissue damage.
- Heat should not be used in conjunction with topical analgesics, over broken skin, or on areas of skin with decreased sensation. Heat-generating adhesive products should be worn over a layer of clothing in patients >55 years of age and should not be used during sleep.
- Heat should not be applied to recently injured (<48 hours) or inflamed areas, because it intensifies vasodilation and can exacerbate vascular leakage and tissue damage.
- For osteoarthritis, nonpharmacologic treatment measures include:
- Applying heat or cold to the affected area.
- Supporting the affected area with splints.
- Performing range-of-motion and strength maintenance exercises.
- Avoiding a sedentary lifestyle and keeping joints active.
- Losing weight if overweight.
- Using assistive devices if needed.
- Applying heat or cold to the affected area.
 Pharmacologic Therapy
Pharmacologic Therapy
- Nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen is used most commonly to treat pain associated with musculoskeletal injuries. These agents are considered to be essentially equivalent in terms of analgesic efficacy; the selection of a particular agent should be based on patient risk factors and preferences. In general, acetaminophen is preferred in noninflammatory diseases, whereas NSAIDs are preferred if inflammation is present.
- Acetaminophen produces analgesia through a central inhibition of prostaglandin synthesis.
- NSAIDs and salicylates produce analgesia through peripheral inhibition of both isoforms of the enzyme cyclooxygenase (COX-1 and COX-2), with subsequent inhibition of prostaglandin synthesis.

Stay updated, free articles. Join our Telegram channel
- Acetaminophen produces analgesia through a central inhibition of prostaglandin synthesis.

Full access? Get Clinical Tree


