Paget Disease
Scott R. Owens, MD
Key Facts
Terminology
Primary
Perianal Paget disease not associated with underlying rectal or anal neoplasm
Secondary
Perianal Paget disease associated with adenocarcinoma of distal rectum or anus
Clinical Issues
Diffuse infiltration of epidermis by malignant cells makes surgical excision difficult
Local recurrence is common
Microscopic Pathology
Large, malignant-appearing cells
Abundant, pale cytoplasm
Cells infiltrate singly or in small clusters
Often more numerous in base of epidermis
Ancillary Tests
Primary EMPD
CK7(+); GCDFP-15(+); CK20(−); CDX-2(−)
Secondary EMPD
CK7(−); GCDFP-15(−); CK20(+); CDX-2(+)
Top Differential Diagnoses
Anal melanoma
Squamous cell carcinoma in situ (Bowen disease)
Diagnostic Checklist
Must exclude underlying visceral adenocarcinoma
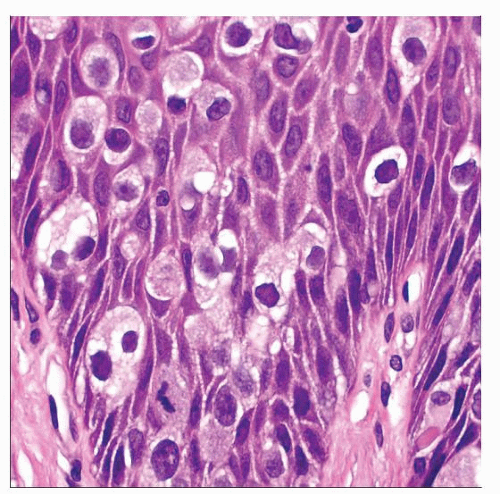
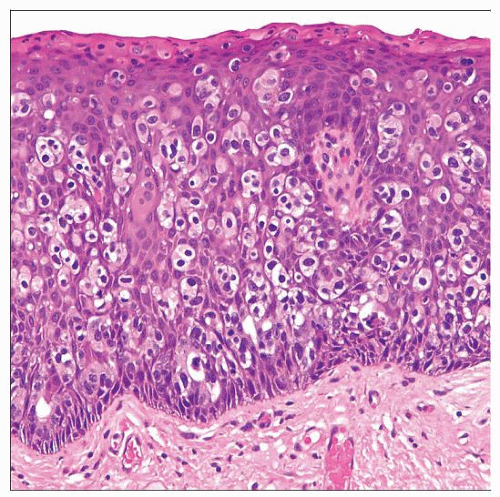 Hematoxylin & eosin shows infiltrative malignant cells within the epidermis. Note predilection of Paget cells for the deeper epidermis and overlying parakeratosis, a common finding. |
TERMINOLOGY
Abbreviations
Extramammary Paget disease (EMPD)
Synonyms
Paget disease of anus
Perianal Paget disease
Definitions
Rare neoplastic condition characterized by infiltration of perianal epidermis by malignant epithelial cells
Primary
Not associated with underlying rectal or anal neoplasm
Secondary
Associated with adenocarcinoma of distal rectum or anus
ETIOLOGY/PATHOGENESIS
Primary EMPD
Controversial origin
Malignant cells may originate within epidermis &/or apocrine glands or ducts
Adnexal “stem cells” have been suggested as cell of origin
Secondary EMPD
Spread of individual mucin-containing adenocarcinoma cells into perianal epidermis
Cells extend distally from gastrointestinal carcinoma
Distal rectum most common
Anal adenocarcinoma also possible (rare)
Manifestation of poorly differentiated adenocarcinoma
CLINICAL ISSUES
Epidemiology
Age
Typically occurs in older patients
Gender
Both sexes are affected
Some cases in perianal region are associated with EMPD of vulva in women
Site
Perianal skin
Presentation
Skin rash
Pruritus
Ulcer
Treatment
Options, risks, complications
Surgical excision difficult
Diffuse infiltration of epidermis by malignant cells makes margin clearance challenging
Medical therapy possible
Surgical approaches
Wide local excision of primary EMPD may be effective
Intraoperative frozen section evaluation of margins necessary
Abdominoperineal resection (APR) may be required
Extensive anal disease
Underlying carcinoma of rectum or anus
Treatment of secondary EMPD must center on treatment of underlying adenocarcinoma
Drugs
Topical imiquimod may be effective
MACROSCOPIC FEATURES
General Features
Rash on perianal skin
Erythema
Raised, moist, or scaly patches
Evidence of pruritus
Hyperkeratosis
Acanthosis
Excoriation
Ulcer
Abdominoperineal resection specimen may be received
Attached rectum may contain adenocarcinoma in cases of secondary EMPD
MICROSCOPIC PATHOLOGY
Key Descriptors
Predominant pattern/injury type
Pagetoid
Infiltration among intact squamous cells
Cells arranged singly or in small clusters
Tubular or glandular structures may be seen (especially when associated with underlying adenocarcinoma)
Often more numerous in base of epidermis
May spread down pilosebaceous units &/or into adnexal structures
Predominant cell/compartment type
Epithelial
Histologic features
Large, malignant-appearing cells
Abundant, pale cytoplasm
Involved epidermis may exhibit pseudoepitheliomatous hyperplasia
ANCILLARY TESTS
Frozen Sections
May be used in cases of primary EMPD where wide local excision is attempted
Identification of Paget cells may be difficult
Epithelioid appearance
Mitotic figures
Possible intracellular mucin vacuole
Histochemistry
Alcian blue/periodic acid-Schiff
Reactivity: Positive
Staining pattern
Cytoplasmic staining pattern
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree