34 1. In many countries the general surgery of children from birth to early teenage years is the preserve of specialist paediatric surgeons. As these surgeons work in centres with paediatric anaesthetic care and paediatric nursing, together with a wide spectrum of paediatric medical expertise, a high level of specialist care is possible. 2. This model of care is not, however, universally available and in exceptional circumstances, in all countries, an adult general surgeon will be called upon to act. Because of unfamiliarity, general surgical junior and senior staff may be intimidated when faced with a young child with a significant surgical problem. There is justifiable concern about the evaluation of a sick child, assessment of respiratory and cardiovascular status and, of course, consideration of an unfamiliar range of potential diagnoses. 3. Attending paediatricians may be accustomed to dealing with sick children but are not usually familiar with the details of surgical disease, nor the likely effects of intervention on the child’s physiology. Although young children and adults differ in their response to surgery, the impact of surgical disease or a surgical procedure are broadly similar and predictable in all age groups. 4. Your assessment of the child prior to and following operation is critical to success. 1. Assessing a 3-day-old infant is clearly different from assessing a 12-year-old child. Nonetheless, certain features of acute surgical diseases are common throughout the paediatric age group. 2. Assess the child’s general demeanour, respiratory rate, level of activity and response to intervention. They all give an initial impression of severity of illness. 3. First assess the cardiovascular status. Ensure the peripheries are warm with palpable peripheral pulses. If you cannot palpate the radial, ankle or foot pulses, impairment of the circulation is likely and needs volume replacement. Give this either as colloid – human albumin or gelatin solution, or as crystalloid – normal (0.9%) saline or Ringer’s lactate. Give 20 ml/kilogram rapidly (<1 hour), repeated two or three times depending on the response. Confirm restoration of circulatory volume by detecting an improved pulse volume or a falling pulse rate. Institute more invasive intravascular monitoring if there is a failure to respond to two such boluses. 4. Examine the abdomen in the standard manner – each quadrant in turn. Palpate gently only in children. Do not perform deep palpation – it is unhelpful. Never seek to test for rebound tenderness; this is quite unreliable. Be patient but persistent when dealing with anxious young children. 5. Digital rectal examination is, for the most part, quite useless. Reserve it usually for those in whom you suspect an anorectal abnormality. In this case have it performed only once by the most senior person available. You rarely gain useful or important information by this manoeuvre. 6. Opinions vary on the usefulness of listening to bowel sounds. We remain convinced that auscultation consistently yields useful information on what is happening within. 7. It is impossible to stop nurses and paediatricians from measuring abdominal girth. We have never seen a patient of any age in whom this information was useful. 1. Respiratory distress or cyanosis at birth in a full term infant may be a consequence of congenital diaphragmatic hernia or oesophageal atresia. Order a chest X-ray as an aid to diagnosis. Diagnose choanal atresia (Greek: choane = funnel; funnel-shaped narrowing of the posterior nares) by your inability to pass a nasogastric tube beyond the nasopharynx. 2. Consider bile-stained (green) vomiting to be the result of mechanical intestinal obstruction until proven otherwise. Always order an abdominal X-ray and carry out a surgical evaluation. 3. Consider abdominal distension as pathological, particularly if it is associated with bile vomiting or a failure to pass meconium (the dark green faeces passed by neonates). 4. All but 3% of full-term infants pass meconium in the first 24 hours. Carefully inspect the perineum if meconium does not appear within this period. If you see a normally sited anus, gently insert a little finger to confirm patency – one of the few indications for this intervention. 5. Failure to pass urine in the first 24 hours is always abnormal. In a male infant, the presence of an associated distended bladder indicates the presence of urethral obstruction, most commonly caused by posterior urethral valves. 6. The majority of abdominal masses in the newborn are renal in origin. Almost all are benign. 7. The passage of blood per rectum is always significant. When the bleeding occurs on the first day of life test the blood to see whether it is fetal or maternal in origin. Subsequent bleeding is almost always from the baby and indicates the presence of intestinal disease. 1. Routine ultrasound examination of the fetus is part of antenatal care. This results in detection of a wide variety of structural abnormalities, often in the first trimester. 2. Detection of an abnormality early in the pregnancy may affect the subsequent management of the pregnancy or the timing and mode of delivery: detection of a lethal abnormality such as anencephaly (Greek: an = no + encephalos = brain) or bilateral renal agenesis raises the question of termination. 3. If you detect an abnormality which can be successfully treated postnatally (e.g. unilateral hydronephrosis) it changes neither the timing nor mode of delivery. Elective caesarean is the likely mode of delivery in the presence of a sacro-coccygeal teratoma or a large exomphalos (Greek: ek = out + omphalos = navel). Occasionally, subsequent scanning reveals not only the persistent abnormality but also deterioration in the condition of the fetus. This is particularly true with chest masses, such as cystic adenomatoid malformations of the lung, where progressive enlargement may result in venous obstruction, and hydrops fetalis (severe oedema of the fetus). Under these circumstances, premature delivery may be the only option available to try to save the baby. 1. With appropriate support, newborn infants can be safely transferred over very long distances. 2. You require transport incubators with facilities to monitor heart rate, body temperature and provide mechanical ventilation. 3. You also need facilities to allow endotracheal intubation, insertion of a chest drain and vascular access. 4. For general surgical transfer, insert an 8 or 10Fr nasogastric tube and leave on free drainage. 5. Ensure that a signed consent form for operation accompanies the baby, together with details of the pregnancy, delivery and postnatal course. 6. Finally, send 10 ml of the mother’s blood with the baby to facilitate cross-matching. 7. If the baby is significantly compromised, as a general rule undertake resuscitation prior to transfer. Only exceptionally should the baby be transferred with ongoing intensive resuscitation. 1. The standard maintenance intravenous fluid available in the UK is 0.45% saline in 5% dextrose. This is adequate for most children, although premature infants may need the dextrose level to be raised to 10%. 2. In the newborn, you may use the umbilical vein but prefer peripherally sited cannulae. 3. Replace fluid losses – nasogastric aspirate or vomiting – using 0.9% saline with 20 mmol of potassium chloride per litre. The standard daily requirements are shown in Table 34.1. 1. In the initial 48 hours after operation, give one half of maintenance requirements. 2. On the third and fourth days, give two-thirds of maintenance requirements and full maintenance fluids from the fifth day onwards. 3. After major surgery there are substantial hidden losses within the tissues and the peritoneal cavity. Assess and replace these losses. Standard replacement fluids for this purpose include normal saline, Ringer’s lactate solution, human albumin or gelatin solutions. 4. Assess the need for such additional fluid on the basis of heart rate, pulse volume, peripheral temperature and urine output. In general, give one or two boluses of 20 ml/kilogram in the first 12–18 hours after major surgery. Calculate such losses and replacement separately from the maintenance fluid which is given in the manner noted above. Calculate nasogastric losses separately and replace them ml for ml. 1. Cross-match 1 unit of fresh packed cells. 2. Administer vitamin K, phytomenadione 1 mg intramuscularly, if this was omitted in the immediate postnatal period. 3. Check the blood glucose using Dextrostix. Correct hypoglycaemia by giving 10% glucose intravenously. 4. Correct any fluid and acid–base imbalance (most acid–base imbalances will self-correct with adequate resuscitation). 5. In all emergencies, keep the stomach empty through a large (8FG) nasogastric tube. 6. Ensure good intravenous access through a cannula conveniently sited for the anaesthetist. 7. Use ECG, pulse, blood pressure and oxygen saturation monitors. Monitors for measuring partial pressures of oxygen and carbon dioxide in inspired and expired gases are also available. 8. For very sick infants, continuously record blood pressure through a transduced intra-arterial cannula, which also facilitates intermittent blood gas analysis and assessments of serum electrolyte and haemoglobin concentrations. 9. Use a central venous cannula when blood loss is expected to be massive or when peripheral venous access is limited, but measurements of central venous pressure are of limited value in this age group. 10. Keep the infant normothermic. Radiant heat losses, especially from the head, must be limited by wrapping the head and swaddling the infant in warm gamgee. A thermostatically controlled warm air blanket should be placed below the patient. The ambient temperature of the theatre should be kept at 26°C with doors closed to prevent draughts. 1. Place the prepared infant supine on the operating table. 2. Make an adequate, transverse skin incision, 1–2 cm above the umbilicus, with a scalpel. 3. Divide the subcutaneous fat and fascia with cutting diathermy to limit blood loss. 4. Similarly, divide the anterior sheath of the left and right rectus abdominus muscles and then divide the muscle bellies. 5. Coagulate the superior epigastric vessels on the deeper surface of each rectus abdominus muscle. 6. Divide the posterior sheath and fascia down to the peritoneum. 7. Open the peritoneum on either side of the midline. 8. Identify, clamp and divide the relatively large umbilical vein. Ligate both ends of the vein with 4/0 polyglycolic acid ties. 9. After assessment, the incision may be readily extended, using cutting diathermy, into the oblique muscles of the abdominal wall at either or both ends. 1. It is unnecessary to close the peritoneum separately. 2. Close the muscles and fascia en masse with either continuous or interrupted sutures of 3/0 or 4/0 polyglactin, polyglycolic acid or polydioxanone. 3. Close the skin with a continuous subcuticular 4/0 or 5/0 suture. 4. Do not use tension sutures or through-and-through skin sutures because the cosmetic results are unacceptable. 1. Inform your anaesthetist of your intention to perform the case laparoscopically. 2. Check that the camera and light source are working correctly. 3. Check that you have an adequate supply of insufflation gas and that your insufflator is working correctly. Select your maximum intra-abdominal pressure (start with 6–8 mmHg in an infant and 8–10 mmHg in an older child). Select a low initial flow rate 0.2 L/min in an infant, 0.5 L/min in an older child. 4. Ensure that equipment and access ports of the correct size are available to you. Use 3 mm equipment for infants and 5 mm for older children. Laparoscopy in infants (e.g. inguinal hernia repair, pyloromyotomy) may be performed without access ports, passing the instruments directly through the thin abdominal wall. Occasionally a larger access port (10 or 12 mm) will be required to remove an operative specimen (e.g. appendicectomy, cholecystectomy). 5. Ensure that a full set of open operating equipment is ready in the event that conversion is required. 1. Make a short transverse incision using a scalpel in the upper margin of the umbilicus long enough for the intended access port. 2. Divide the subcutaneous fat with scissors down to the linea alba. 3. Clear a short (approximately 1 cm long) section of the linea alba so that you can see it clearly. Pick up the linea alba with two artery forceps, one just above the umbilicus, the other 1 cm cranial to this. 4. Incise the linea alba transversely between the artery forceps with a knife, taking care not to incise the underlying peritoneum or umbilical vein. 5. Pick up the peritoneum with two pairs of toothed forceps, ensuring that you have not picked up bowel or omentum, and incise it with a scalpel. 6. At this stage insert a 3/0 (infant) or 2/0 (older child) polyglycolic acid suture in a purse-string around the edges of the muscular layer. A suture mounted on a ‘J’ shaped needle is preferable for this. Inserting the suture at this stage improves the seal and security of the access port. 7. Insert the access port mounted with a blunt trocar. 8. Tighten the purse-string suture around the access port, place one throw of a knot on the suture and use the long end of the suture to secure the access port in the wound. 9. Attach the gas tubing to the access port and begin insufflation. Ensure that a pneumo-peritoneum is developing by abdominal examination. There should be free flow of gas into the peritoneal cavity up to the pre-set insufflation pressure. If a pneumo-peritoneum is not developing or if the flow of gas is not free then cease insufflation, check that the access port is correctly located in the peritoneal cavity and restart. 10. Perform a laparoscopic examination of the abdominal cavity to confirm the preoperative diagnosis and identify optimal sites for working port insertion. As a general rule, these should be on either side of the camera with an adequate angle between them to allow easy vision and comfortable dissection. 11. Insert the working ports under direct vision. Make a short transverse skin incision with a scalpel. Insert a port mounted with a cutting trocar and advance it into the peritoneal cavity using a back and forth screwing type movement. Watch carefully via the laparoscope to avoid damage to abdominal viscera. Once the port is within the abdominal cavity, remove the trochar and insert a working instrument. 1. Remove all working instruments and working ports. Approximate the muscle edges using a 4/0 or 5/0 polyglycolic acid suture. Observe the inside of the incision through the laparoscope to ensure adequate closure and avoid damage to viscera with the needle. 2. Once working ports are closed, cease insufflation, remove the laparoscope and primary port and allow gas to escape. 3. Undo the single throw on the purse-string suture and tighten the suture, approximating the edges of the wound. Tie the suture, ensuring that the defect is completely closed with no viscera (especially omentum) extruding. 4. Close the subcutaneous tissue with a 4/0 polyglycolic acid suture. 1. An anastomosis may be created between two intestinal ends following resection so long as there is a healthy blood supply. Discrepancy in the size of the two ends is not a contraindication to anastomosis. However, in case of doubt it is often safer to fashion a stoma. 2. Identify the ends to be anastomosed, ensuring their orientation is correct. 3. Trim each end so that the margin is straight and clean. Clear the mesentery from the serosal surface of the bowel for a few millimetres from the cut edge to create a clean margin for anastomosis, ensuring that you do not impair the blood supply. 4. Take an appropriately sized monofilament suture – 4/0 in a child, 4/0 to 6/0 in an infant. 1. Starting on the mesenteric border, place a single extramucosal, seromuscular suture approximating the two edges. Place this suture adjacent to the mesentery, taking care not to damage the vessels. Leave the end of this suture long and grasp it with artery forceps to aid manipulation. 2. Place an additional single interrupted suture on either side of, but close to the first suture. 3. Place a single suture approximating the edges on the ante-mesenteric border. Leave the end long and grasp it with artery forceps. 4. Using the artery forceps to lay the anastomosis out in front of you, complete the anterior wall of the anastomosis using a single layer of interrupted extramucosal sutures. Ensure that they are adequately spaced to make a water-tight anastomosis, but not so tight as to cause ischaemia. If there is a discrepancy in size between the two ends you will need to leave a wider space between each suture on the wider end of bowel than the other. 5. Use the artery forceps to turn the bowel over, laying out the posterior wall in front of you. Complete the anastomosis as for the first side. 1. An ileostomy or colostomy may be required in a number of scenarios whenever it is desirable or essential to divert the faecal stream. The loop colostomy is one of the most commonly used stomas in paediatric surgery and is suitable in the infant with obstruction such as Hirschsprung’s disease or anorectal malformations, as well as some conditions in older children. End stomas may be created in small or large intestine. 2. When creating an ileostomy it is prudent to evert a section of the bowel to create a luminal orifice away from the skin so as to protect the skin from effluent. We describe the techniques of loop colostomy and end ileostomy. Prescribe preoperative antibiotics giving anaerobic cover. 1. Make a V-shaped incision, either in the left iliac fossa for a sigmoid colostomy, or in the right hypochondrium for a transverse colostomy. The latter colostomy has the advantage of leaving sufficient distal colon for secondary surgery to be performed in conditions requiring mobilization of the distal colon. 2. Carry the V incision through skin and subcutaneous tissue. 3. Raise the flap of the V, exposing the underlying muscle. 4. In an older child you may need to extend the incision in the skin and subcutaneous layer to allow adequate room for passage of the colon. Turn a V-shaped incision into a W (see Fig. 34.2). 5. Split the muscle transversely, perpendicular to the V incision. 6. Open the peritoneum in the same direction as the muscle. 7. Locate the part of the intestine that will form the colostomy. Remember that the sigmoid loop may be greatly dilated and may appear in the right upper quadrant where it is easily confused with the transverse colon. The lack of an attached omentum serves to differentiate it from the transverse colon. 8. Ensure that the bowel is not twisted as it is drawn to the surface. Twisting may produce intestinal obstruction. 9. Make a small opening in the colonic mesentery. 10. Pass the apex of the V skin flap through the mesenteric defect and suture it to its original position with two or three loosely tied 4/0 polydioxanone sutures. 11. Incise the colon longitudinally with cutting diathermy. 12. Suture the full thickness of the opened colon to the surrounding skin with interrupted 4/0 polyglycolic acid sutures. 1. Consider the continuing need for antibiotics and the duration of postoperative starvation. In general terms, the child can take oral fluids and then a light diet once the stoma begins to function. At this point place a stoma bag. 2. This technique may also be used to form a loop ileostomy. In this case you should attempt to evert the proximal limb using the technique described below for terminal ileostomy. 1. Identify a suitable location on the abdominal wall for the stoma. This should be on flat skin, with a wide enough margin for application of a stoma bag. 2. Consider where you will place the mucous fistula to the distal bowel. Ideally this should be beside the functioning stoma in order to facilitate eventual stoma closure. 3. Ensure that the bowel end is healthy with an adequate blood supply and that the mesentery is long enough for the cut end to reach the anterior abdominal wall. 1. Excision of a disc of skin is not usually necessary: a simple transverse incision is usually satisfactory. 2. Carry the incision through the subcutaneous tissue and split the muscle. Ensure that the peritoneum is divided adequately to avoid obstruction of the intestine. 3. Place grasping forceps through the incision and grasp the end of the bowel to be made into a stoma. Pull the bowel through, ensuring that it does not become twisted and that the entire thickness of the bowel wall passes through the opening. 4. Draw the bowel out of the wound and suture the peritoneum or deep muscular fascia to the serosa, leaving an adequate length to form a mature everted stoma. 5. Place a suture through the skin, through the adjacent serosa, then take a full-thickness bite of the cut end of the bowel and tie the knot snug with the skin, everting the bowel. Repeat this circumferentially using 4 or 6 sutures to form a spout. 6. This technique may also be used to form a terminal colostomy. In this case you do not need to evert the bowel forming a spout, but can simply suture the bowel flush with the skin edge. 1. Stenosis, which may cause partial or even complete obstruction and require dilatation or revision of the stoma. 2. Prolapse usually involves the distal limb of a loop stoma. An attempt at reduction should be made, but this is sometimes difficult and revision may be necessary. A small degree of uncomplicated prolapse is well tolerated and is best left alone. 1. Proximal small-bowel obstruction is usually associated with bile-stained vomiting, a failure to pass meconium and an absence of abdominal distension. Mid-small-bowel obstruction or distal intestinal obstruction is usually associated with abdominal distension from early in life and subsequently with bile-stained vomiting. Frequently, there is a failure to pass meconium. 2. Abdominal X-ray confirms whether the obstruction is high or low, depending on the number of gas-filled loops seen on the X-ray film. If the anus is present, perform a digital examination to confirm that the anus is patent and also to see if the baby subsequently passes flatus and stool. Obviously, in the presence of intestinal atresia or meconium ileus, no flatus will be passed but the reverse is true in the presence of Hirschsprung’s disease, when explosive decompression may occur. 3. Ideally, prefer to transfer the child to a regional centre, but if this is not possible, then perform a laparotomy without undue delay. 4. Do not hesitate to decompress the upper gastrointestinal tract by passing a nasogastric tube and administer intravenous fluids. 5. Administer broad-spectrum antibiotics, including cover for gram-negative organisms and anaerobic organisms. The procedure performed depends on the operative findings: 1. If duodenal atresia is encountered, tack together the two duodenal segments with three or four seromuscular sutures. Then open the two segments with parallel incisions and complete an anastomosis. 2. For jejunal atresia, the best option is an end-to-end anastomosis but this is not a straightforward anastomosis for a non-specialist surgeon as it necessitates tapering of the very dilated proximal bowel. Under these circumstances a side-to-side anastomosis may be safer. 3. For distal small-bowel atresia, either a double-barrelled stoma or end-to-end anastomosis is possible. 4. Construct all anastomoses using fine monofilament sutures – nothing larger than a 5/0 suture – using the standard anastomosis technique previously described. 5. In meconium ileus, the distal small bowel is plugged with inspissated pale meconium pellets. Proximal to this, the small bowel is dilated and filled with tenacious meconium. Preferably perform an enterotomy in the dilated bowel and patiently evacuate all intestinal content with the help of saline irrigation. Close the enterotomy. 6. With complicated meconium ileus – in the presence of a twisted gangrenous segment or an associated atresia – resect the compromised bowel, evacuate intestinal contents and, ideally, anastomose the remaining intestine. If this is not possible, then create a double-barrelled stoma. 7. In Hirschsprung’s disease, the intestine is in continuity but there is usually a change of calibre in the sigmoid colon. Under these circumstances, the best option is to perform either a right transverse colostomy or an ileostomy in the terminal ileum. This allows the baby to be fed and the length of affected bowel can be assessed at leisure.
Paediatric surgery
GENERAL CONSIDERATIONS IN PAEDIATRIC SURGERY
INTRODUCTION
ASSESSMENT OF THE ‘SURGICAL’ CHILD
ASSESSMENT OF THE ‘SURGICAL’ NEWBORN
PRE-NATAL DIAGNOSIS
NEONATAL TRANSPORT
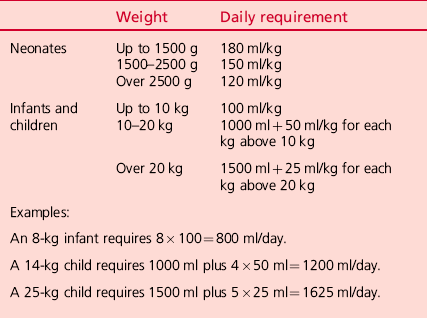
INTRAVENOUS FLUIDS – THE STANDARD MAINTENANCE
Postoperative fluid requirement
GENERAL PAEDIATRIC SURGICAL TECHNIQUES
THE ABDOMINAL OPERATION IN INFANTS AND CHILDREN
Prepare
Access
Closure
LAPAROSCOPY IN INFANTS AND CHILDREN
Preoperative preparations (in addition to those for laparotomy)
Access
Closure
INTESTINAL ANASTOMOSIS (Fig. 34.1)
Prepare
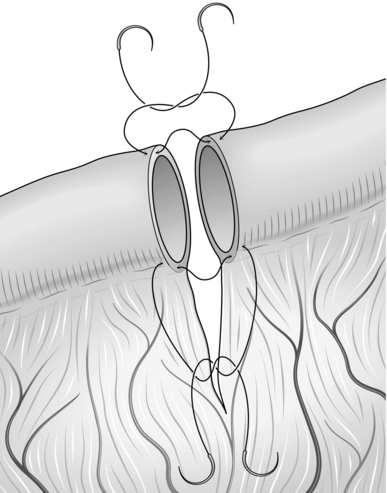
Action
STOMA FORMATION
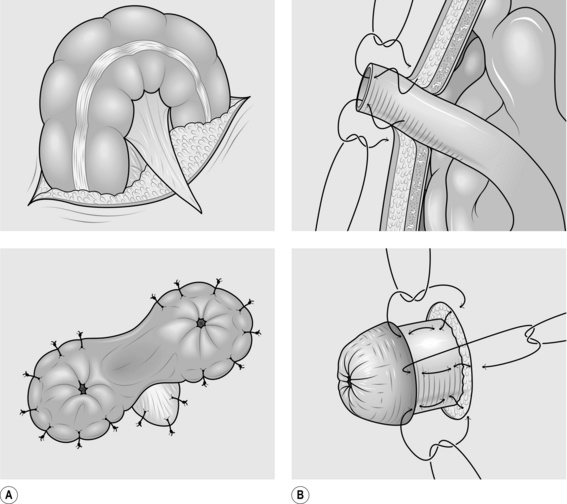
LOOP COLOSTOMY (Fig. 34.2)
Action
Aftercare
TERMINAL ILEOSTOMY
Prepare
Action
Complications
CONDITIONS PRESENTING MAINLY IN THE NEWBORN OR NEONATAL PERIOD
NEONATAL INTESTINAL OBSTRUCTION
Appraise
Action
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Paediatric surgery