Overview and Classification of Systemic Vasculitides
Surya V. Seshan, MD
TERMINOLOGY
Synonyms
Primary systemic vasculitides
Definitions
Pathological
Vasculitis is defined as inflammation of blood vessels with demonstrable structural injury such as disruption of elastic lamina ± fibrinoid necrosis
Often, occlusive changes due to inflammatory infiltrate or thrombosis are evident
Clinical
Clinical definition is not possible due to organ-specific or multisystemic disease
Rapid or prolonged evolution of clinical features over time may impede or delay definitive diagnosis
Thorough correlation with pathophysiologic mechanisms, serology, and imaging studies is essential
History
Vasculitis 1st described by Kussmaul and Maier in 1866; termed “periarteritis nodosa”
Giant cell arteritis described by Hutchinson in 1890
Multiple vessel involvement and transmural arterial inflammation led to term “polyarteritis nodosa” by Ferrari in 1903 and later by Dickson in 1908
Takayasu arteritis described by Takayasu in 1909
Granulomatosis with polyangiitis (Wegener) described by Klinger and Wegener in 1931 and 1934, respectively
Allergic granulomatosis and angiitis described by Churg and Strauss in 1951
Introduction of term “necrotizing angiitis” and attempt to classify vasculitis by Zeek in 1952
Vasculitis and mucocutaneous lymph node syndrome described by Kawasaki in 1966
Introduction of the term “microscopic polyangiitis” in 1994 by Jennette et al
Classification Considerations
No ideal classification
Vasculitides may be primary or secondary to systemic disease
Vasculitides can be localized to 1 organ or affect multiple organ systems
Consensus conferences have developed classifications and criteria based on demographics, clinical characteristics, and pathology
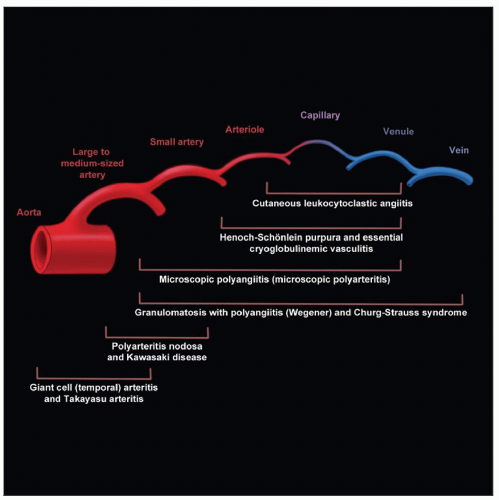
CHAPEL HILL CONSENSUS CONFERENCE NOMENCLATURE OF SYSTEMIC VASCULITIDES (1994)
General
Most widely used classification system
Developed definitions and standardized diagnostic terminology
Classification is based on size of arterial vessel involved and type of inflammatory reaction
While size-specific vasculitides are identified, significant overlap in size exists between diagnoses, and ANCA testing may be helpful
Cutaneous leukocytoclastic angiitis is a separate category except for those with immune complex deposits or associated with positive ANCA serology
Pulmonary renal syndromes of pauci-immune small vessel vasculitides may have similarities and can be distinguished by ANCA serology
Pathological correlation with clinical and laboratory features may identify specific therapeutic groups
Large Vessel Vasculitis
Giant cell (temporal) arteritis
Granulomatous arteritis of the aorta and its major branches, with predilection for extracranial branches of carotid artery
Often involves temporal artery
Usually occurs in patients older than 50 and often is associated with polymyalgia rheumatica
Takayasu arteritis
Granulomatous inflammation of aorta and its major branches usually occurring in patients < 50 years
Medium-sized Vessel Vasculitis
Polyarteritis nodosa (classic polyarteritis nodosa)
Necrotizing inflammation of medium-sized, or small arteries without glomerulonephritis or vasculitis in arterioles, capillaries, or venules
Kawasaki disease
Arteritis involving large, medium-sized and small arteries, and associated with mucocutaneous lymph node syndrome
Coronary arteries are often involved
Aorta and veins may be involved
Usually occurs in children
Small Vessel Vasculitis Including Capillaries, Venules, Arterioles, and Arteries
Granulomatosis with polyangiitis (Wegener)
Granulomatous inflammation involving respiratory tract and necrotizing vasculitis affecting small to medium-sized vessels
Necrotizing glomerulonephritis is common
Churg-Strauss syndrome
Eosinophil-rich and granulomatous inflammation involving respiratory tract and necrotizing vasculitis affecting small to medium-sized vessels; associated with asthma and eosinophilia
Microscopic polyangiitis (microscopic polyarteritis)
Necrotizing vasculitis with few or no immune deposits, affecting small and medium-sized vessels
Necrotizing glomerulonephritis is very common
Pulmonary capillaritis often occurs
Henoch-Schönlein purpura
Vasculitis with IgA-dominant immune deposits, affecting small vessels
Typically involves skin, gut, and glomeruli, and is associated with arthralgias or arthritis
Essential cryoglobulinemic vasculitis
Small vessel vasculitis with cryoglobulin immune deposits
Associated with cryoglobulins in serum
Skin and glomeruli are often involved
Cutaneous leukocytoclastic angiitis
Involves cutaneous leukocytoclastic angiitis without systemic vasculitis or glomerulonephritis
OTHER CLASSIFICATION SYSTEMS
American College of Rheumatology (1990)
Criteria for diagnosis of vasculitides
Clinical criteria were developed to standardize cohorts of patients in almost all primary systemic vasculitides
Presence of 3 or more criteria were associated with high degree of sensitivity and specificity for diagnosis in appropriate context
Application of criteria for individual patients may not be entirely helpful
International Pediatric Consensus Conference (2006)
Childhood vasculitis
Criteria for childhood PAN include histopathological evidence of necrotizing vasculitis or angiographic abnormality along with 1 clinical finding
Birmingham Vasculitis Activity Scores (BVAS)
BVAS and vascular damage index (VDI) are applied to assess clinical activity and severity in patients with vasculitis
EPIDEMIOLOGY
Incidence
Depends on specific types of vasculitis and associated primary or secondary systemic diseases
Ethnicity and Distribution
Takayasu arteritis and Kawasaki disease most common in Asia and Far East countries
Granulomatosis with polyangiitis (Wegener) and Churg-Strauss syndrome have predilection for North America and Northern Europe, mainly in Caucasians
Higher incidence of microscopic polyangiitis in Asia
ETIOLOGY/PATHOGENESIS
Etiology
Immune complexes
Mixed cryoglobulinemia
Lupus erythematosus
Henoch-Schönlein purpura (presumed)
Possibly other vasculitides
Autoantibodies
ANCA
Polyangiitis
Granulomatosis with polyangiitis (Wegener)
Churg-Strauss syndrome
Possibly other vasculitides
Idiopathic
Takayasu arteritis
Kawasaki disease
Giant cell arteritis
Other factors
Infections
Bacteria, viruses, fungi, rickettsia, parasites
Drug reaction
CLINICAL IMPLICATIONS
Clinical Presentation
General constitutional symptoms are common with all forms of vasculitis in initial or acute stage
Specific signs and symptoms depend on several factors
Single or multiple organ system involvement
Size and type of vessel involved
Pathogenetic mechanisms
Pathological findings
Severity of disease
Specific presenting symptoms of complications of vasculitis
Vascular narrowing
Stenosis
Occlusion
Aneurysm formation with rupture
Symptoms can be acute, subacute, or chronic
Clinical features of vasculitis can mimic vasculitis-like diseases, vasculopathies, and, rarely, nonvascular diseases
Renal findings in vasculitis
Hematuria
Proteinuria
Acute renal insufficiency or failure
Rapidly progressive renal failure
Slowly progressive renal failure
Chronic renal failure
Benign or malignant hypertension
Laboratory Findings
Acute phase response is associated with active vasculitis
Rise in C-reactive protein
Elevated erythrocyte sedimentation rate
Increased plasma viscosity
Complete blood counts
Varied granulocytosis or lymphocytosis
Thrombocytosis
Anemia
Specific organ function tests
Kidney, lung, heart, liver, pancreas, endocrine
Serologic tests
Various types of infections
Autoantibodies
Antineutrophil cytoplasmic antibodies
Antinuclear antibodies
Rheumatoid factor
Antiglomerular basement membrane
Other less frequent but specific antibodies
Complement levels
C3, C4, C1q
Urinalysis
Hematuria
Proteinuria
Casts
Cells
Imaging Findings
Most useful in large and medium-sized vessel vasculitides
Specific types of vessel involvement contribute toward definitive diagnosis
Each diagnostic category may have several vascular patterns by imaging studies
Variety of imaging modalities may be used to identify specific vascular abnormal patterns
Plain x-ray
Angiography
Computed tomogram
Magnetic resonance
Doppler studies
Tc-99m DMSA scanning
Prognosis
Vasculitides range from self-limiting to relapsing disease involving different organs
Significant diagnostic delays occur due to frequent clinical overlap and nonspecific findings leading to worse prognosis
Varied morbidity and mortality
Specific organ involvement
Severity of vasculitis
Complications
Sequelae of vasculitis contribute to further organ damage (stenosis, occlusion)
Infectious complications secondary to immunosuppressive treatment are not uncommon
Treatment
Ideally, therapeutic approaches should be based on etiology &/or pathophysiology of the vasculitides
Corticosteroid therapy alone is useful for giant cell arteritis and Churg-Strauss syndrome without renal involvement
Clinical heterogeneity and varied immune-mediated pathogenetic mechanisms prompt empirical form of initial therapy
A number of treatment protocols are in use for primary and secondary vasculitides
Cyclophosphamide and steroids in small vessel vasculitides
Plasmapheresis and anti-CD20 antibody in severe disease
Several immunosuppressive agents including oral steroids, methotrexate, and azathioprine are employed for maintenance of remission
MACROSCOPIC FINDINGS
General Features
Large and medium-sized vessel vasculitides display distinctive gross characteristics from specimens obtained following excision during surgery or autopsy specimen
Gross findings of renal vasculitides of all sizes include segmental or total infarction and progressive atrophy in renal artery stenosis
Cortical petechial hemorrhages in small vessel vasculitides
MICROSCOPIC FINDINGS
General Features
Several variables have to be considered before histopathological diagnosis is rendered
Selection of appropriate tissue for biopsy
Sample size
Age of disease process
Prior immunosuppressive therapy
Nonspecific and specific findings
Types of vascular inflammation in vasculitis
Neutrophil rich
Eosinophil rich
Lymphocytic
Granulomatous
Necrotizing
Focal, segmental
Circumferential
Other findings
Endothelial injury and necrosis
Disruption of internal &/or external elastic lamina
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree