The distribution of infectious diseases often occurs in a non-random fashion leading to what may be referred to as clusters, outbreaks or epidemics. Investigation of outbreaks like that described in Box 13.1 is part of the core business of field epidemiology and it relies on multidisciplinary approaches to identifying and controlling disease. The outbreak of toxigenic E. coli O104:H4 is a dramatic example of the seriousness of contamination in the food supply, and how spread of infectious diseases can be controlled through rapid investigation and intervention.
Detection of event: A local health department requested assistance from the German federal government with investigation of 3 cases of haemolytic uraemic syndrome (HUS, a rare condition that affects the kidneys) in northern Germany on 19 May 2011. On investigation, it became obvious that the outbreak had started weeks earlier and the number of cases of gastroenteritis and HUS peaked on 22 May 2011.
Descriptive epidemiology: In total, 3816 cases were reported in Germany. The majority of patients had bloody diarrhoea with 22% progressing to develop HUS and 36 (4.2%) died. The rates of infection were highest in northern Germany and most of those affected were adults (median age 42 years) and women (68%). The estimated incubation period was 8 days from exposure to illness. Cases also occurred in several other countries in Europe and North America, but the majority of these had acquired their infection while visiting Germany.
Investigation: The investigating teams conducted multiple studies to understand the source of infection, including: explorative hypothesis-generating interviews, 30 cohort studies, several case–control studies, testing of potentially contaminated foods and microbiological studies. Initial interviews of patients did not reveal the food causing the outbreak – contaminated fenugreek seed sprouts – as they were difficult to remember. The particular strain of Escherichia coli responsible – serotype O104:H4 – had not been seen in animals previously and was rare in humans; importantly, it showed characteristics of multiple pathogenic types of E. coli and resulted in an unusually high proportion of people developing HUS.
Containment: The outbreak was rapidly brought under control once sprouts were identified as the food vehicle. The fenugreek seeds originated from Egypt and were sprouted at a small farm in northern Germany. Once the vehicle was identified and removed from the food supply the only new cases were due to secondary transmission within households.
Implications: The outbreak resulted in significant societal concern and had major implications for trade of food and agricultural produce. Early reports suggested the outbreak was linked to Spanish cucumbers. These were later shown to be false, but costs to agriculture were estimated to be hundreds of millions of Euro.
Historically, the study of epidemic infections helped develop methods for epidemiology, especially retrospective cohort and case–control studies, and, as shown in Box 13.2, epidemiology still plays a central role in outbreak investigation. Investigations of outbreaks still have a high public profile today, particularly because of the globalisation of trade and increasing ease of international travel. Emerging and re-emerging infections have become prominent over the last two to three decades and the threat of global epidemics, or pandemics, has mobilised resources to plan for, detect and combat such catastrophes. Many examples earlier in this book focussed on ‘chronic’ or ‘non-communicable’ diseases. Now we will discuss infectious diseases, although not exclusively, because other agents such as toxins and chemicals can also result in ‘outbreaks’ of non-communicable intoxications, injuries and cancer.
Epidemiology is central to investigating and correctly managing outbreaks of disease. In particular, epidemiology is used to:
detect clustering in surveillance data that may represent an increase in cases of disease warranting investigation
identify and count cases that may be related to an outbreak or cluster
develop and conduct cohort or case–control studies to identify sources of illness during or after an outbreak has occurred
characterise the risks to populations potentially exposed to a source of illness
monitor the effectiveness of risk communication in outbreak settings
Outbreaks, epidemics and clusters
What do we mean by an epidemic or an outbreak? The two terms are often used interchangeably, although they are perceived differently in the media and by the public. Epidemic comes from the Greek words epi (upon) and dēmos (the people) and means an increase in disease in a region or time period that is clearly above what would normally be expected. Most diseases are endemic, in that they are commonly present at a baseline level in a given geographic area or population group. Increases above the endemic baseline or incursions of diseases into new areas may signal the occurrence of an epidemic.
An outbreak is defined as ‘an epidemic limited to a localised increase in the incidence of a disease, e.g. in a village, town or closed institution’ (Porta, 2014, p. 206). Outbreak may also be used to refer to a small epidemic arising in an area that has had no cases for a long time. In general, outbreaks include two or more cases, but a single case of a rare disease, such as botulism, could represent an outbreak.
When a disease affects a large number of people and crosses international boundaries it is called a pandemic. Historically, pandemics have caused great loss of human populations, notably plague in the late middle ages and ‘Spanish’ influenza at the end of World War I. The organism causing the most recent pandemic as declared by the World Health Organization (WHO) under the International Health Regulations – H1N1 influenza virus – first appeared in Mexico in April 2009 and quickly spread to over 200 countries by the end of the year. H1N1 infections resulted in less-severe disease than health departments had planned for, but did result in more serious outcomes in young adults and pregnant women.
Finally, it is important to understand the use of the word cluster, which is an aggregation ‘of relatively uncommon events or diseases in space and/or time in amounts that are believed or perceived to be greater than could be expected by chance’ (Porta, 2014, p. 47). Health agencies often use this term where there is no obvious source of disease identified, and it may be used for both infectious and non-communicable diseases, such as cancer.
Epidemiology of infectious diseases
Infectious disease epidemiology is often presented as a different discipline from the epidemiology we have been describing, but the fundamental principles are similar and causal reasoning is conceptually simpler for infectious diseases where the agent or ‘pathogen’ is a necessary cause of the disease. The major difference for most infectious conditions, and other outbreaks we discuss here, is the urgency with which investigations take place and the direct link to management activities. This is often extreme and demands robust, practical methods for identifying people who are exposed and infected, along with a constant focus on controlling the outbreak before all information has been gathered.
Infectious or communicable diseases are defined as ‘An illness due to a specific infectious agent or its toxic products that arises through transmission of that agent or its products from an infected person, animal or reservoir to a susceptible host, either directly or indirectly through an intermediate plant or animal host, vector, or the inanimate environment’ (Porta, 2014, p. 51). The burden of infectious diseases in terms of incidence and mortality in industrialised countries has declined dramatically since the 1950s when the use of powerful antibiotics, vaccines and other interventions became routine (van Panhuis et al., 2013). In low-income countries, there is still an ongoing epidemiological transition from a pattern of high mortality rates due to infectious diseases of childhood to one of non-communicable diseases later in life (Dye, 2014; GBD 2013 Mortality and Causes of Death Collaborators, 2015). Despite these major changes in burden of disease, infectious diseases remain highly prevalent and important in all countries of the world. Some of the major concerns with infectious diseases globally include:
the threat of antimicrobial resistance leading to untreatable infections;
the emergence of new highly pathogenic and virulent strains;
the resurgence of diseases once thought controlled because of lowered vaccination rates;
the opportunity to eliminate, and potentially eradicate diseases such as smallpox, Guinea worm, polio and measles;
the regular occurrence of high-profile outbreaks of infectious diseases that threaten community health, trade and security; and
the synergistic effects of infectious diseases on the burden of non-communicable diseases.
Acute infections affect all sectors of society and the public health impacts are substantial. Even common infections, such as gastroenteritis and respiratory infections, result in considerable lost productivity. Periodically, epidemics of vaccine-preventable diseases recur, even in countries with very high vaccine coverage; for example, pertussis (whooping cough), rubella and measles. There are also many infections that have recently emerged or re-emerged and for some we have made little headway with prevention or treatment, for example Hendra virus transmitted from horses and bats in Australia, novel coronaviruses in the Middle East, and varicella-zoster infection, which causes shingles and is common among the elderly.
 More about SARS
More about SARS
Many of these emerging infections are zoonotic in origin, in that they have reservoirs in animal populations (Jones et al., 2008), and a high proportion are due to pathogenic viruses, such as rapidly evolving RNA viruses including those that cause AIDS, SARS and influenza. Emergence is based on many factors including population growth, expanding trade and travel, mass-produced food, intensive livestock production, environmental change, resistance to antimicrobial drugs, human encroachment on wilderness and forest, and global warming (Sleigh et al., 2006). The SARS multicountry epidemic of 2003 was an example of a global threat due to emergence of a new infectious disease that had origins in live animal markets in Asia, which were also subsequently identified as a potential risk for transmission of highly pathogenic H5N1 influenza (Samaan et al., 2011).
In addition, infectious diseases are a particular problem for vulnerable populations, such as the very young, the elderly or those who are immunocompromised due to disease or medical treatment. In some instances, those who are vulnerable may be predisposed to infection or, when infected, they may experience worse outcomes. Many people in these categories are regular visitors to the hospital environment where they are at risk of opportunistic infections, some of which have become highly resistant to antimicrobial agents. WHO (2015) has declared the emergence of antimicrobial resistance a global health concern resulting in many countries developing plans for antibiotic stewardship, monitoring of usage and surveillance of antibiotic resistant organisms.
The public health impacts of infectious diseases are substantial: epidemics capture the public and media attention, but the majority of burden arises from infections that are endemic. Sometimes outbreak alerts trigger worldwide alarm and politically complex national and international responses, as has been noted recently with Ebola virus in West Africa and Middle East Respiratory Syndrome (MERS) caused by a novel coronavirus. Increasingly, small or large outbreaks threaten economically important industries, as seen with Hendra virus in Australia in 1994 that had impacts on the horse racing industry, Nipah virus in Malaysia in 1998–1999 affecting pig farming, SARS in Hong Kong and Canada in 2003 affecting services and tourism, and regular outbreaks of food-borne disease affecting various food businesses.
A causal model
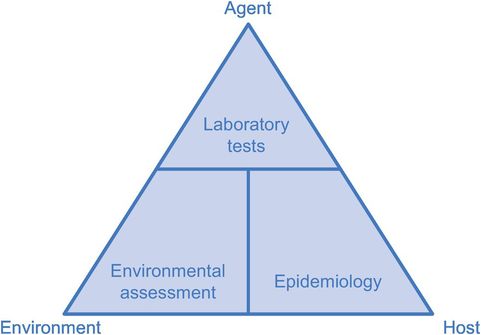
Simple ecological models of the ‘agent–host–environment’ interplay have served infectious disease epidemiology well, providing a neat structure for linking the variety of factors that determine whether disease occurs. Figure 13.1 shows the interaction between an infectious agent and its potential host, the transmission process (how the disease is spread) and how all of these may be influenced by the environment. The relationship between the agent, host and environment are largely understood by laboratory testing, epidemiology and environmental surveys, respectively.
The infectious agent
There are many different types of infectious agent: bacteria, viruses, fungi, protozoa, helminths (parasitic worms), etc. In almost every natural habitat there will be agents potentially infectious to humans. Animal contact is particularly important in the genesis of human infections and many (perhaps most) infections afflicting us have been traced back to the beginnings of agriculture and animal farming.
Infection is the entry of a microbial agent into a higher-order host and its multiplication within the host. When a lower organism lives on an external surface of another organism it is called an infestation rather than an infection; for example, lice and scabies. Infections do not necessarily lead to overt disease and the principal characteristics of microbial agents that influence their ability to cause disease are defined below.
Infectivity is the ability of an organism to invade and multiply in a host and is assessed by the proportion of exposures that result in infection. One measure of infectivity is the secondary attack rate, which measures the number of cases of infection that develop among susceptible contacts of an infected case. Polio virus is a highly infectious agent infecting most susceptible people who are exposed, but only a small proportion will develop symptoms or chronic sequelae from their infection. Its pathogenicity, the power of an organism to produce overt illness, measured as the proportion of those infected who develop clinical or overt illness, is therefore relatively low. Measles virus is highly infectious like polio, but is much more pathogenic in that most people infected develop symptoms. Virulence, the ability of an organism to produce serious disease, is measured by the proportion of those infected who develop severe disease. If death is a criterion of severity, this can be measured by the case–fatality ratio (CFR, see Chapter 2). The intensity of an infection, the number of organisms infecting an individual, is especially important for parasitic infections, such as hookworms or schistosomes, where the burden of parasites often predicts the severity of disease.
The natural habitat of the agent is known as its reservoir and this may be human, animal or in the environment. Agents with human reservoirs include the pertussis bacterium, the malarial parasite and the roundworm. For some agents such as Vibrio cholera, the cause of cholera, it is unclear what the reservoir is between epidemics. The source of an infectious agent is the person, animal or object from which the host acquires the infection. If human, this may be someone who is sick or convalescent, or a long-term carrier of infection who was never clinically sick themselves, as can happen with hepatitis B, typhoid and HIV.
Laboratory testing (chemical, microbiological, serological or genetic) is a critical element in understanding the agent. A detailed discussion is beyond the scope of this book, but it is important to realise that, combined with epidemiology, new genomic testing of infectious agents has revealed striking new insights into their transmission as the genetic code of the agent from the putative source can now be compared with that of the infected humans. In investigations of acute outbreaks, laboratory testing of foods and water, animals, humans and the environment is critical to identify the source of infection.
In a study of typhoid in Nepal, the diversity of typhoid genotypes revealed that while human-to-human transmission occurred, this was overwhelmed by indirect transmission, possibly via contaminated water (Baker et al., 2011).
The host
The host is a human or animal that an agent enters and in which it multiplies. A host’s reaction to infection can be extremely variable, depending on the interplay between the characteristics of the agent, including the dose received, and the immune status of the host. The immune response of the very young and the old may not be as protective as that of a young healthy adult. If the host has been exposed to the agent before there may be natural immunity, or immunity may be induced artificially by vaccination. A person who is not immune to a particular agent is often referred to simply as a ‘susceptible’. These factors, and others to do with the biology, maturation and replication of the agent, influence the incubation period which is the time between initial infection and the onset of clinical disease as shown by signs and symptoms. For control of infectious diseases it is also important to know the latent period, the time from entry into the host until the onset of infectiousness, which may be longer or shorter than the incubation period. If it is shorter, then infected persons may pass on the infection before they become ill, as with hepatitis A, and if it is longer they will be ill before they are very infectious, as for SARS. These features are known for the majority of infectious diseases and are an important determinant of infection dynamics. They are useful tools in the investigation and control of epidemics and are always the focus of attention for new emerging infectious diseases. Infections transmitted before someone becomes ill, or by someone who does not become ill, are the most difficult to control and the most likely to cause explosive epidemics in susceptible populations.
Transmission
Transmission of an agent is its spread from a reservoir or source to a new host by one or more of three possible routes: direct, indirect or airborne. For example, SARS is usually transmitted by (large) respiratory droplets reaching close contacts, but some cases have spread infection to scores of persons with whom they had little or no direct contact (Li et al., 2004). The mode of transmission has a profound effect on how infectious diseases are managed, both in the clinical setting and in the community. As an example, ordinary masks and gloves are used in hospitals as precautions against heavy respiratory droplets, but are inadequate against airborne infections which require fitted masks or respirators, eye shields and negative-pressure ventilation. Some modes of transmission are shown in Figure 13.2 and discussed in more detail below.
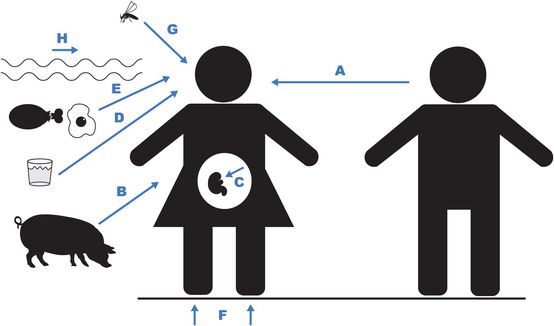
Direct transmission arises from ‘close personal contact’ by touching infectious secretions or excreta from another person (A) or animal (B). This includes touching or inhaling the large (10–100 μm) respiratory droplets produced by a person suffering from a respiratory infection sneezing, coughing or talking. These heavy droplets contain mostly water and pass through the air to fall on surrounding objects within 1 metre of the source (Fernstrom and Goldblatt, 2013). Examples of direct transmission include sexual, skin, eye, congenital and most respiratory infections, including measles and influenza. Sometimes vertical transmission (as opposed to the usual horizontal transmission (A)) occurs directly from mother to unborn child (C) for diseases such as listeriosis where serious bacterial meningitis or septicaemia can result from eating contaminated foods.
Indirect transmission always involves a vehicle, which may be inanimate, such as bedding, clothes or utensils (collectively called ‘fomites’), water (D) or food (E), or the soil (F). Alternatively, the infection may be transmitted via a vector (G), such as a mosquito responsible for malaria or dengue.
Airborne transmission (H) became an outmoded concept in the nineteenth century after Snow had shown that London cholera was waterborne, disproving the prevailing theory of an infectious airborne ‘miasma’ rising from the river. Later, Pasteur and others demonstrated the existence of germs and showed that they could be transmitted directly through the air. In the 1930s, the laboratory production of ‘bioaerosols’ of tiny infectious droplet nuclei that could be inhaled, as well as careful epidemiological studies on TB and Q fever in the 1940s and 1950s, eventually resurrected the concept of airborne infection as an important mode of transmission (Langmuir, 1961). Bioaerosols may also be produced in abattoirs when cutting open the body cavities of infected animals, in air-conditioning cooling towers, or by germ warfare. WHO uses a particle size of <5 μm in diameter to define particles that may be airborne and infectious over large distances. These include pathogens such as Mycobacterium tuberculosis, for which this mode is obligate (it is transmitted only in this way), and pathogens that can infect by multiple routes but are mostly transmitted by droplet nuclei (their preferential pathway), such as measles and chickenpox (Fernstrom and Goldblatt, 2013).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


