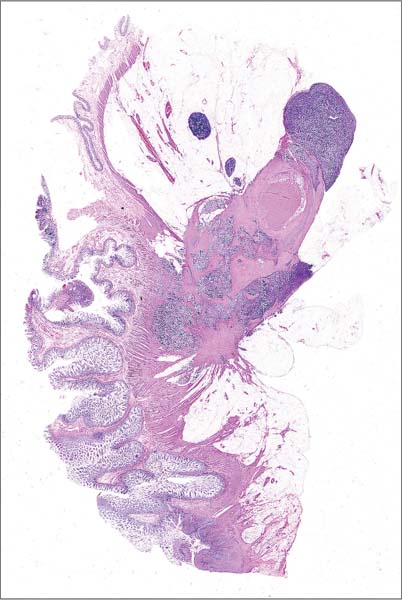
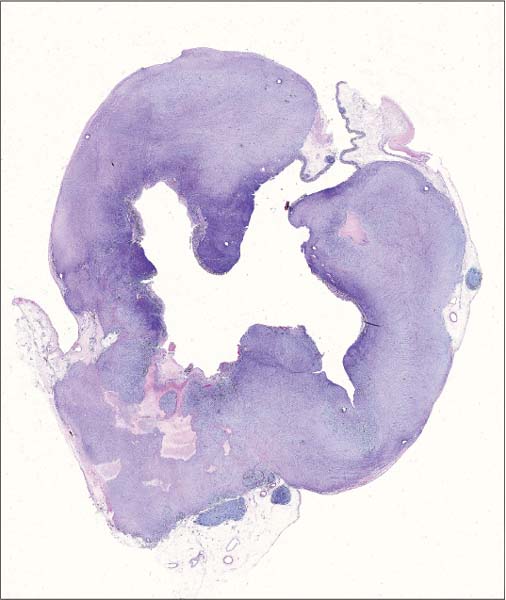
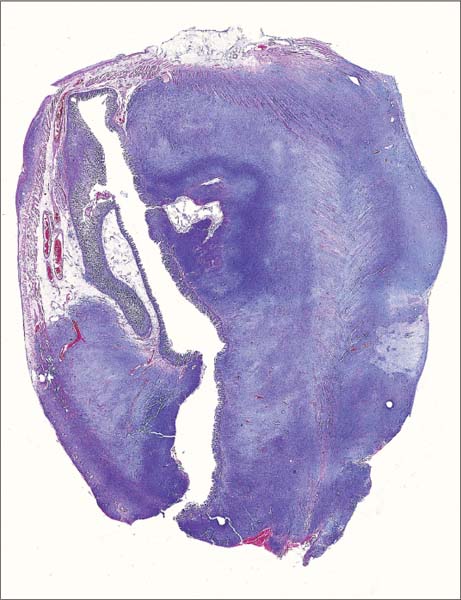
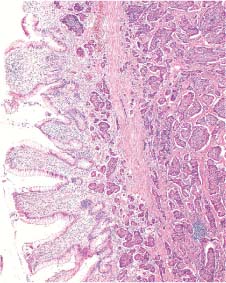
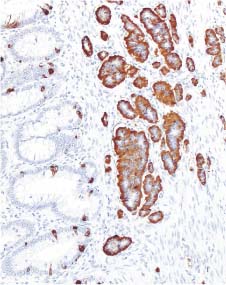
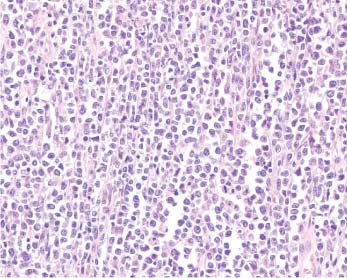
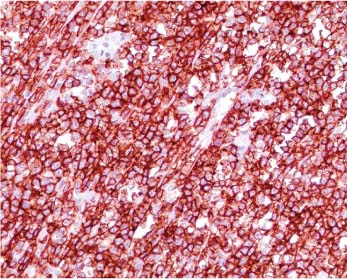
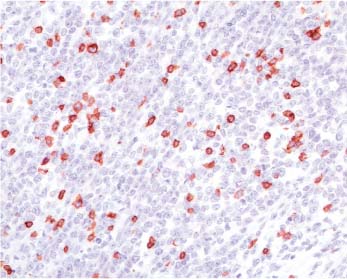
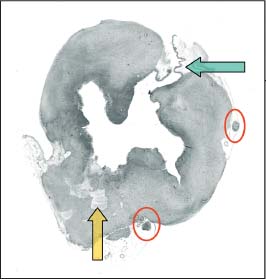
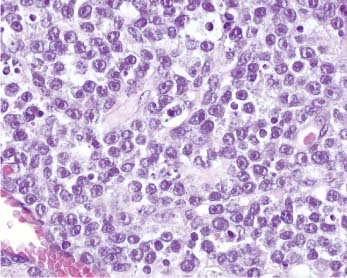
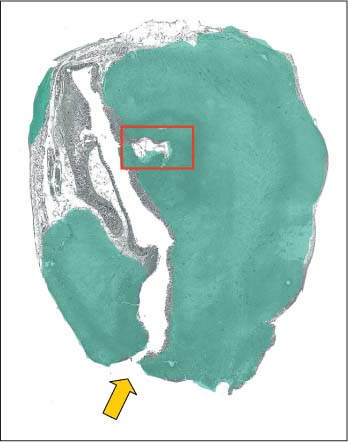
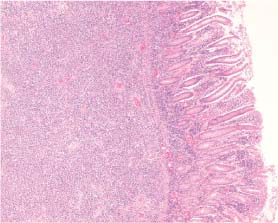
4 Other Intestinal Neoplasms Patient data: 53-year-old man presenting with abdominal pain. Radiologic examination revealed stenosis of the terminal ileum. Surgical treatment: Ileocecal resection, no preoperative treatment. Specimen: 30-cm-long segment of the large intestine and an 8-cm part of the terminal ileum with a 5-cm infiltrating tumor mass with a yellow cut surface, in the area of the ileocecal valve. Histopathologic diagnosis: Carcinoid tumor with lymph node metastasis (1/14). Follow-up: Died of the disease 49 months after the operation. The large section in Figure 4.1 demonstrates multiple round foci of tumor tissue invading all the layers of the wall of the small intestine. The section in fact corresponds to the ileocecal region and also contains structures of the colon (located in the left upper corner of the image). Microscopy revealed structures of carcinoid tumor corresponding to the red-colored areas in Figure 4.1c. The tumor originated in the mucosa of the small intestine, as demonstrated in Figure 4.1a, which is a microscopic magnification of the area marked with the yellow rectangle in the schematic image (Fig. 4.1c). The tumor cells exhibited a strong immunohistochemical reaction with the endocrine marker chromogranin A (Fig. 4.1b). Some lymph nodes free of metastasis were also present in the specimen (marked with green arrows in Fig. 4.1c). The intestinal wall was thickened as a result of hypertrophy of the lamina muscularis propria, a typical phenomenon associated with carcinoid tumor. A deep ulceration is also seen at the distal end of the specimen. Fig. 4.1a Fig. 4.1b Fig. 4.1c Schematic guide to the details in the large section in Fig. 4.1. Fig. 4.1 Large-section histology image of carcinoid tumor of the ileocecal region. Patient data: 70-year-old-woman presenting with anemia. Colonoscopy revealed a large tumor mass in the cecum. The preoperative endoscopic biopsy contained mainly necrotic debris, thus raising suspicion of malignancy. Surgical treatment: Ileocecal resection, no preoperative treatment. Specimen: 50-cm-long segment of the large intestine together with an 8-cm part of the terminal ileum and tumorous appendix. A 10-cm infiltrating tumor was found in the cecum, and several tumor masses were found in the mesenterium. Histopathologic diagnosis: Diffuse malignant non-Hodgkin’s B-cell lymphoma of follicular origin, intermediate grade. Follow-up: Died of the disease 7 months after the operation. The large histologic section in Figure 4.2 demonstrates the typical appearance of a malignant lymphoma in the intestine: a diffuse, monotonous infiltrate leading to thickening of the intestinal wall due to discohesive growth of the tumor cells. The same monotonous histologic picture, seen in Figure 4.2a, could be obtained by magnifying any part of the tumor. This lymphoma was made up of atypical B-lymphocytes (as shown by immunohistochemical reaction with the B-cell marker CD20, Fig. 4.2b) and contained only a few reactive T-lymphocytes (Fig. 4.2c, immunohistochemical reaction with CD3). The green arrow in Figure 4.2d indicates the zone of transition between the normal intestinal structures and the tumor, the yellow arrow indicates areas of tumor necrosis. These areas may explain the results of the preoperative histologic examination in this case. Interestingly, there are reactive lymph nodes free of lymphoma in the immediate vicinity of the tumor (encircled in Fig. 4.2d). Fig. 4.2a Fig. 4.2b Fig. 4.2c Fig. 4.2 Large-section histology image of a primary malignant lymphoma of the colon. Fig. 4.2d Schematic guide to the morphologic details in the large section on Fig. 4.2. Patient data: 88-year-old woman with previously diagnosed malignant lymphoma who presented with abdominal pain. On laparotomy, diffuse purulent peritonitis was detected and several independent tumor masses were seen in the small intestine. As a cause of peritonitis, intestinal perforation was found in one of the tumor-infiltrated segments. Surgical treatment: Partial intestinal resection. Specimen: 27-cm-long segment of the small intestine with a 6-cm-large tumor mass 3cm from the margin. Additional smaller tumor masses were also present. Perforation in the area of the largest tumor and peritonitis. Histopathologic diagnosis: Diffuse malignant non-Hodgkin’s B-cell lymphoma of large-cell type, high-grade. Follow-up: Died of the disease 12 months after the operation. The large histologic section in Figure 4.3 demonstrates another case of malignant lymphoma, this time infiltrating the wall of the small intestine. The diffuse thickening of the intestinal wall is very well seen. As indicated by the yellow arrow in the schematic image (Fig. 4.3b), the intestinal wall was perforated due to ulceration and necrosis of the tumor tissue. Necrotic areas were also present in other parts of the tumor; the most obvious of them is marked with a red rectangle in the schematic image. Figure 4.3a is a microscopic magnification of a detail from the tissue of the high-grade lymphoma with large atypical cells containing prominent nucleoli. Fig. 4.3a Fig. 4.3b Schematic guide to the morphologic details in the large section in Fig. 4.3. Fig. 4.3 Large-section histology image of a malignant lymphoma of the small intestine. Patient data: 61-year-old man presenting with episodes of abdominal pain. Colonoscopy revealed a large tumor mass in the cecum. Preoperative biopsy did not contain any tumor structures. Surgical treatment: Right hemicolectomy, no preoperative treatment. Specimen: Right hemicolectomy with 25-cm-long segment of the large intestine together with a 4-cm part of the terminal ileum and a 9-cm infiltrating tumor mass in the area of the ileocecal valve. Tumor mass in the mesenterium. Histopathologic diagnosis: Diffuse malignant non-Hodgkin’s B-cell lymphoma, intermediate grade. Follow-up: 17 months, no signs of disease recurrence. The large histologic section in Figure 4.4 demonstrates a primary malignant lymphoma of the colon infiltrating the ileocecal region. The massive infiltration of the blue-stained tumor tissue is well seen in the mesenterium. There are large areas of tumor necrosis (indicated by the yellow-colored areas in Fig. 4.4e). The mucosa was only partly preserved and mostly ulcerated. Figure 4.4a is a microscopic magnification of the area indicated with the red rectangle in Figure 4.4e and demonstrates the intestinal mucosa on the right side of the image and the tissue of the lymphoma on the left side. Absence of a reaction with the epithelial marker cytokeratin Cam5,2 (illustrated in Fig. 4.4b) indicates a non-epithelial tumor (the rest of the normal epithelium is stained brown). Figure 4.4c, d is a high-power microscopic magnification of the lymphoma and also proves the aggressive nature of the tumor, which shows perivascular and intramuscular infiltration. Note the enlarged reactive lymph node (marked with a blue arrow in Fig. 4.4e). Massive necrosis of the tumor tissue may appear in lymphomas as well as in carcinomas and can lead to the formation of pseudolumen, as was already demonstrated in Case 3.14.
Case 4.1 Carcinoid Tumor of the Ileocecal Region

Practical points
Case 4.2 Primary Malignant Lymphoma of the Colon
Practical points
Case 4.3 Intestinal Lymphoma
Practical points
Case 4.4 Intestinal Lymphoma with Massive Necrosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree