Osmotic Tubulopathy
Shane M. Meehan, MBBCh
Key Facts
Terminology
Tubular epithelial swelling and isometric vacuolization, associated with exposure to parenteral carbohydrate solutions or contrast media, and acute kidney injury
Etiology/Pathogenesis
Parenteral infusion of hyperosmolar agents
Carbohydrate: Dextrans, mannitol, sucrose
Contrast agents
Mechanism includes direct toxic and ischemic tubular injury
Clinical Issues
Acute oliguric renal failure
Diagnosis is by kidney biopsy
Microscopic Pathology
Diffuse or focal clear cell change with luminal narrowing of proximal tubules
Uniform isometric vacuolization of proximal tubular epithelium
Top Differential Diagnoses
Tubular calcineurin inhibitor toxicity
Ischemic tubular injury
Tubulopathy associated with nephrotic syndrome
Diagnostic Checklist
Cell swelling with luminal narrowing or obliteration rather than attenuation
Electron microscopy reveals endosomes and lysosomes, and preserved surface microvilli
TERMINOLOGY
Abbreviations
Osmotic tubulopathy (OT)
Synonyms
Osmotic nephrosis, contrast nephropathy, (radio)contrast-induced acute kidney injury, intravenous immunoglobulin-associated tubular toxicity
Definitions
Tubular epithelial swelling and isometric vacuolization, associated with exposure to parenteral carbohydrate solutions or contrast media, and acute kidney injury
ETIOLOGY/PATHOGENESIS
Causes
Parenteral infusion of hyperosmolar agents including
Parenteral carbohydrate solutions
Mannitol: Used as plasma expander and for treatment of cerebral edema
Dextran: Used as plasma expander
Hydroxyethyl starch (HES): Used as plasma expander and in perfusion preservation of kidney transplants (UW solution)
Glucose, sucrose, and maltose: Stabilizing agents
Intravenous immunoglobulin (IVIg): Sucrose and maltose used as stabilizing agents
Radiologic contrast agents: Iodine-containing agents, ionic or nonionic, high and low osmolality
Pathogenesis
Hyperosmotic solutions are filtered and then absorbed by proximal tubules by pinocytosis
Solute is retained in endosomes and not broken down
Intracellular oncotic gradient is thus created and results in water absorption and hydropic swelling
Accumulation of pinocytotic vesicles is dose related
Vacuoles arise by fusion of vesicles with lysosomes
Experimentally, vacuolar change appears in minutes and disappears in days after exposure
Direct toxicity from disruption of cellular integrity and possible oxidative injury
Secondary afferent arteriolar vasoconstriction and efferent vasodilation reduces glomerular filtration rate
Risk Factors
Age > 65 years
Preexisting chronic renal failure and diabetic nephropathy
Concurrent exposure to nephrotoxic agents
Coexistent ischemic or hypoxic renal injury, especially in kidney transplants
Dehydration
Quantity and osmolarity of administered solution, especially for contrast media and mannitol
CLINICAL ISSUES
Epidemiology
Incidence
Incidence varies with agent administered and presence of associated risk factors
Presentation
Acute deterioration of function of native and transplanted kidneys with exposure to inciting agents
Renal failure may develop and resolve without clinical symptoms or signs
Renal failure is typically oliguric
Renal dysfunction begins within days of infusion and reverses after cessation of infusion
Persistent impairment is rare
High osmolal gap (measured osmolality minus calculated osmolality)
Diagnosis is by kidney biopsy
Treatment
Prevention by hydration using iso-osmolar fluids
Renal replacement therapy necessary in up to 40% of patients
Plasma exchange for removal of dextran
Prognosis
Recovery after cessation typically takes days to weeks
Prolonged renal failure over months may be observed
End-stage renal failure is rare
Significant increase in mortality associated with acute renal failure
MACROSCOPIC FEATURES
Gross Examination
Enlarged and pale kidneys
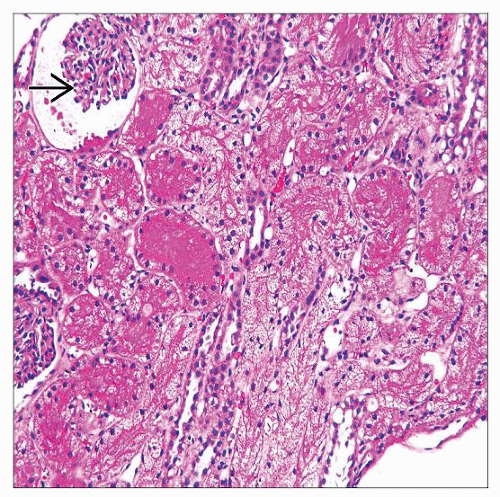
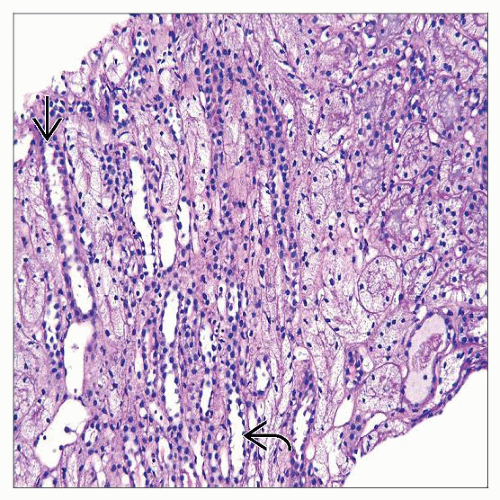
MICROSCOPIC PATHOLOGY
Histologic Features
Diffuse or focal clear cell transformation with lumenal narrowing or solidification of proximal tubules
Uniform isometric vacuolization of proximal tubular epithelium of convoluted and straight segments
Vacuoles impinge on nuclear membrane imparting scalloped appearance
Vacuoles are 1-4 microns in diameter and appear empty
Earliest vacuoles in cell apex
Vacuoles may persist with protracted renal failure
Preservation of brush border on PAS staining
Cellular necrosis and sloughed cells are uncommonly seen
Immunofluorescence studies are negative
Immune complex deposits are not seen with IVIg usage
Electron microscopy
Abundant cytoplasmic vacuoles and lysosomes
Surface microvilli are preserved
Vacuolization of parietal epithelium of Bowman capsule, podocytes, and interstitial cells may be seen
Mild cortical interstitial edema with scattered inflammatory cells may be evident
Distal tubules and collecting ducts are unaffected
Lesions are seen in native and transplanted kidneys
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree