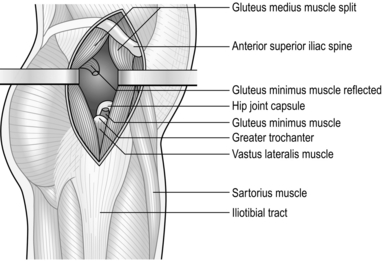
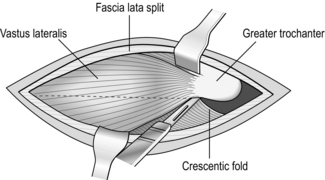
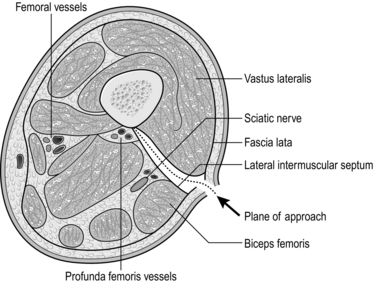
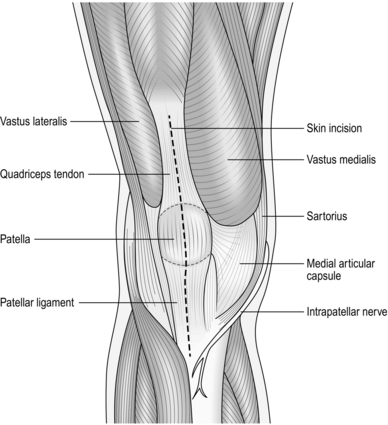
32 1. The hip joint is deeply placed and relatively inaccessible. 2. It may be exposed by several routes that are variations of the anterior, posterior and lateral approaches, which themselves afford good access for most purposes. 3. The anterolateral approach is an extensile approach and provides adequate access for drainage of a potentially septic hip, as well as more complex procedures such as total hip arthroplasty. 4. The lateral approach is usually used for open reduction and internal fixation of femoral fractures. 1. Order 2 units of cross-matched blood. 2. A general anaesthetic is preferable, especially in a child. However, if the general condition of the patient precludes it, use an epidural or spinal anaesthetic. 3. Place the patient supine on the operating table with a sandbag under the buttock of the side to be operated on. 4. Have an unscrubbed assistant elevate the leg. 5. Clean the skin distally from the umbilicus to the knee, including the anterior abdominal wall, perineum and as much of the buttock as possible. 6. Place a waterproof sheet under the affected leg and over the opposite leg, tucking it under the buttock. 7. Place a large drape over the waterproof sheet so that the whole of the unaffected leg and foot and the lower part of the operating table are covered. Pull the top edge firmly into the groin to exclude the genitalia from the field. 8. If possible, use a split sheet to shut off the groin. If this is not possible, fold a medium-sized towel corner-to-corner and place the centre of the long side firmly in the groin. Take one corner under the leg and the other over the iliac crest, and clip the corners together onto the skin at the posterior end of the iliac crest. 9. With the scrubbed assistant, hold a medium towel outstretched by the corners under the leg from the lower third of the thigh to beyond the foot. Direct that the leg be lowered carefully into it and turn the bottom end over the foot before carefully wrapping the lower thigh, leg and foot in the towel. Bandage the towel firmly on to the leg with an open-weave bandage or stockinette. 10. Cover the patient’s head and trunk with a large drape. 11. Place the leg through the hole in a large split sheet. Pull the sheet firmly into the groin and around the buttock but leaving the anterolateral aspect of the thigh exposed from the iliac crest distally. 12. Cover the exposed skin with a large adhesive drape wrapped around the thigh. 1. Make a straight incision extending from the anterior superior iliac spine directed towards the tip of the greater trochanter. This follows the junction between the gluteus medius and the tensor fascia lata. 2. Incise the fascia overlying the interval between the two muscles and develop the plane proximally towards the anterior superior iliac spine. Insert a self-retaining retractor, such as the Norfolk and Norwich type, between the two. 3. It should now be possible to see the tendon of the gluteus minimus and the capsule of the hip joint. 4. Retract the gluteus minimus posteriorly and incise the capsule of the hip joint, draining any accumulated intra-articular fluid. Send a sample for bacteriological analysis. 1. This exposure may be carried proximally to expose the hip joint if required. 2. Use the distal part of the approach alone for access to the proximal part of the femur and the femoral neck, when treating fractures in this region. 1. Cross-match 2 units of blood. 2. Operate with a general anaesthetic if possible, or with epidural or spinal anaesthesia. 3. If you are operating for fixation of a femoral neck fracture, place the patient supine on the orthopaedic operating table with a radiolucent perineal post to allow access for an image intensifier or portable X-ray machine. Operative fixation of femoral neck fractures is, however, beyond the scope of this chapter. 4. Straightforward exposure of the femur is usually carried out with the patient in the lateral position. A traction table and X-ray control are not necessary. 5. Clean the skin from the level of the umbilicus to the knee, including the perineum and buttock and the circumference of the thigh. 6. Hang a large drape over the sound side from the groin to beyond the toes. 7. Hang another large drape over the affected leg from the mid-thigh to beyond the toes. 8. Cover the trunk above the iliac crest with a third large sheet. 9. Cover the remaining part of the thigh with two small towels, leaving only a rectangle of skin 30 cm long by 20 cm wide exposed on the lateral side of the thigh. The anterior superior iliac spine is situated at the top corner of this rectangle. 10. Hold the towels in place with a transparent adhesive drape. 1. Palpate the posterosuperior corner of the greater trochanter and make a straight longitudinal incision from that point for 15 cm distally, through the skin and subcutaneous fat. 2. Split the fascia lata longitudinally, posterior to the insertion of the tensor fascia lata muscle, in the line of the incision. Insert a self-retaining retractor to expose the vastus lateralis. 3. Identify the aponeurotic attachment of the vastus lateralis to the anterolateral surfaces of the femur, just below the greater trochanter. 4. Identify the posterior attachment of the vastus lateralis. Insert two Trethowan bone spikes and lift the body of the vastus lateralis forwards, releasing it from its attachment to the linea aspera (Latin: asper = rough), cauterizing vessels as you go. 5. Reflect the muscle subperiosteally from the anterolateral aspect of the femur and strip the muscle from the anterior and lateral aspects of the femur with a periosteal elevator. Insert the tip of your index finger between the vastus lateralis and the anterior surface of the femur and palpate the lesser trochanter on the posteromedial aspect of the bone. 6. Pass a Lane’s lever carefully around the femoral shaft with the tip absolutely in contact with the bone, so that it lies between the lesser trochanter and the femoral neck. This exposes the anterior and lateral surface of the upper femoral shaft and the base of the femoral neck. 7. Strip the posterior portion of the muscle from the bone in similar fashion and insert a second Lane’s lever around the underside of the femoral shaft. 1. The femoral shaft may be approached from the anterior, medial or lateral aspects. 2. The posterolateral approach is the most convenient and most commonly used. 1. Have 2 units of cross-matched blood available. 3. For operations on the distal two-thirds of the thigh, it may be possible to use a tourniquet but this may compromise the exposure. 4. Place the patient supine on the operating table with a sandbag under the buttock of the affected side. 5. Elevate the leg and clean the skin from the iliac crest and buttock – or the tourniquet, when used, to the upper tibia. 6. Place a large sheet across the operating table and over the sound leg, and pull the upper edge firmly into the groin to cover the genitalia. 7. Place the long edge of the ‘shut-off’ towel in the groin, or immediately below the tourniquet, and pull it firmly round the thigh; fasten it with a towel clip on the lateral side. 8. Place a medium-sized drape on the table with its upper edge at the level of the knee joint and carefully lower the leg on to the towel. 9. Fold the distal edge of the towel proximally over the foot and then wrap the towel around the leg. 10. Bandage the towel firmly to the leg with an open-weave bandage or stockinette. 11. Cover the trunk with a large sheet and clip it to the underlying sheet on either side of the thigh. 12. Pass the leg through the hole in a split sheet. Clip the margins of the split to the skin at the upper limit of the operating field. 13. Wrap a large transparent adhesive drape round the thigh to cover the exposed skin. 1. Palpate the tendon of the biceps femoris at the level of the lateral femoral condyle and also the posterior margin of the greater trochanter. 2. Incise the skin along the whole or part of the line joining these two points to gain access to the appropriate part of the thigh. 3. Incise the fascia lata in the line of the incision and locate the lateral intermuscular septum immediately anterior to the biceps femoris. 4. Insert a finger between the septum and the bulk of the vastus lateralis lying anteriorly and continue the dissection down to the bone in this plane with a knife. 5. Ligate the perforating branches of the profunda femoris vessels as you encounter them. 1. Most operations on the knee joint are carried out from the front, but many do not require a full and formal exposure of the whole joint, and a more limited exposure is adequate. 2. The posterior approach is used to gain access to the popliteal fossa and occasionally to the posterior part of the knee joint. 1. Make a straight incision 15 cm long in the midline, extending proximally from the upper margin of the tibial tubercle. 2. Deepen the incision to expose the patellar ligament, the anterior surface of the patella and the quadriceps tendon, and the distal fibres of the rectus femoris (Fig. 32.4). 3. Reflect the skin and subcutaneous fat as a single layer medially, to expose the junction of the quadriceps tendon and the vastus medialis, the medial border of the patella and the patellar ligament. 4. Make an incision along the medial edge of the quadriceps tendon and through the capsule along the medial margin of the patella and medial edge of the patellar ligament into the joint. 5. If required, evert the patella, retract it laterally, and flex the knee at the same time (Fig. 32.5). Extend the incision proximally into the rectus femoris if this proves to be difficult.
Orthopaedics and trauma
lower limb
APPROACHES TO THE HIP AND PROXIMAL FEMUR
ANTEROLATERAL APPROACH
Prepare
Access (Fig. 32.1)
LATERAL APPROACH TO THE PROXIMAL FEMUR
Prepare
Access (Fig. 32.2)
APPROACHES TO THE UPPER LEG
POSTEROLATERAL APPROACH (Fig. 32.3)
Prepare
Access
APPROACHES TO THE KNEE
ANTERIOR APPROACH (Fig. 32.4)
Prepare
Access
Orthopaedics and trauma: lower limb