Chapter 11 Orbital Blood Supply
Internal Carotid Artery
The internal carotid artery runs upward through the neck and enters the skull through the carotid canal, located in the petrous portion of the temporal bone just superior to the jugular fossa. Within the anterior portion of the canal, only thin bone separates the artery from the cochlea and the trigeminal ganglion. The internal carotid artery leaves the canal and immediately enters the cavernous sinus, where it runs forward along the medial wall beside the sphenoid bone; it then exits through the roof of the sinus. Within the sinus, the abducens nerve is closely adherent to the lateral border of the internal carotid.1 Throughout its pathway—up the neck, into the skull, and through the cavernous sinus—the internal carotid is surrounded by a plexus of sympathetic nerves from the superior cervical ganglion. The second and third cranial nerves accompany the vessel as it leaves the sinus; the optic nerve lies medial and the oculomotor nerve lies lateral to the internal carotid. The ophthalmic artery branches from the internal carotid artery just as it emerges from the cavernous sinus medial to the anterior clinoid process of the sphenoid bone. It is usually the first major branch from the internal carotid artery.2
Clinical Comment: Sclerosis of the Internal Carotid Artery
Compression of the optic nerve caused by sclerosis of the internal carotid artery was found in some postmortem studies, with pathologic changes such as atrophy, evident in the optic nerve. Visual field defects may be caused by this compression and should be one of the differential diagnoses when optic nerve head atrophy accompanies a field defect.3
Ophthalmic Artery
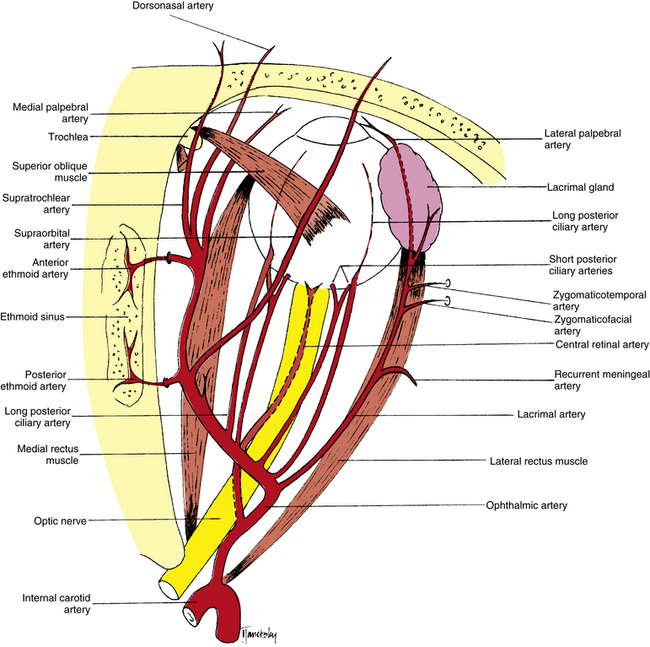
The ophthalmic artery enters the orbit within the dural sheath of the optic nerve and passes through the optic canal, below and lateral to the nerve2 (Figure 11-1). A network of sympathetic nerves surrounds the vessel.4 Once in the orbit the ophthalmic artery emerges from the meningeal sheath, runs inferolateral to the optic nerve for a short distance, and then crosses either above or below the nerve. Together with the nasociliary nerve, the ophthalmic artery runs toward the medial wall of the orbit.5 The artery continues forward between the medial rectus and superior oblique muscles, giving off branches to various areas. Just posterior to the superior medial orbital margin, it divides into its terminal branches, the supratrochlear and dorsonasal arteries. In general, the intraorbital arteries are located in the adipose compartments and perforate the connective tissue septa as they pass between sections.6 The ophthalmic artery is the main blood supply to the globe and adnexa but is supplemented by a few branches from the external carotid supply.
Marked variability is evident in the order of the origin of the branches of the ophthalmic artery, and the sequence appears to correlate with whether the artery crosses above or below the optic nerve. The most common patterns of distribution are shown in Table 11-1.7 Many anatomic variations can occur in the branches and their courses; those most often reported are included here.
Table 11-1 Order of Origin of Branches of Ophthalmic Artery
| Order of Origin | SEQUENCE OF BRANCHES WHEN OPHTHALMIC ARTERY: | |
|---|---|---|
| Crosses Above Optic Nerve | Crosses Below Optic Nerve | |
| 1 | Central retinal and medial posterior ciliary | Lateral posterior ciliary |
| 2 | Lateral posterior ciliary | Central retinal |
| 3 | Lacrimal | Medial muscular |
| 4 | Muscular to superior rectus and levator | Medial posterior ciliary |
| 5 | Posterior ethmoid and supraorbital, jointly or separately | Lacrimal |
| 6 | Medial posterior ciliary | Muscular to superior rectus and levator |
| 7 | Medial muscular | Posterior ethmoid and supraorbital, jointly or separately |
| 8 | Muscular to superior oblique and medial rectus, jointly or separately | Muscular to superior oblique and medial rectus, jointly or separately |
| 9 | To areolar tissue | Anterior ethmoid |
| 10 | Anterior ethmoid | To areolar tissue |
| 11 | Medial palpebral or inferior medial palpebral | Medial palpebral or inferior medial palpebral |
| 12 | Superior medial palpebral | Superior medial palpebral |
| Terminal | Dorsonasal and supratrochlear | Dorsonasal and supratrochlear |
Modified from Hayreh SS: The ophthalmic artery. III. Branches, Br J Ophthalmol 46:212, 1962.
Central Retinal Artery
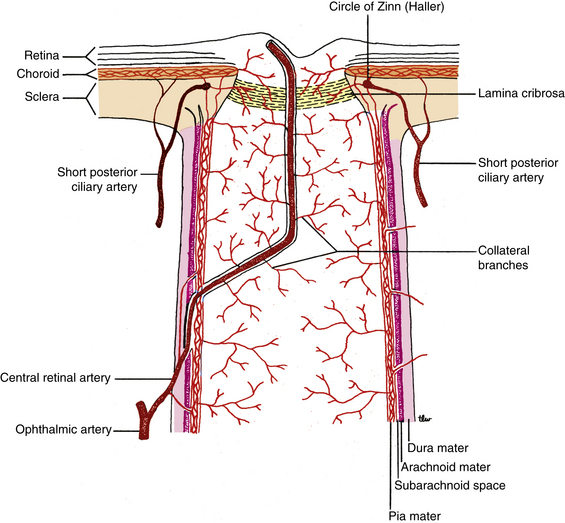
One of the first branches of the ophthalmic artery, the central retinal artery, is among the smallest branches. The central retinal artery leaves the ophthalmic artery as it lies below the optic nerve (see Figure 11-1). The artery runs forward a short distance before entering the meningeal sheath of the nerve about 10 to 12 mm behind the globe (Figure 11-2). While within the optic nerve, the central retinal artery provides branches to the nerve and pia mater.7 (Often, these branches are called collateral branches.) As the central retinal artery runs forward within the optic nerve, a sympathetic nerve plexus (the nerve of Tiedemann) surrounds the artery.8 The central retinal artery passes through the lamina cribrosa and enters the optic disc just nasal to center, branching superiorly and inferiorly. These branches divide into nasal and temporal branches, then continue to branch dichotomously within the retinal nerve fiber layer. The retinal blood vessels are discussed in Chapter 4.
Lacrimal Artery
One of the largest branches, the lacrimal artery, leaves the ophthalmic artery just after it enters the orbit (see Figure 11-1); rarely, it branches before the ophthalmic artery enters the optic canal.9 The lacrimal artery and the lacrimal nerve run forward along the upper border of the lateral rectus muscle. Within the orbit the lacrimal artery may supply branches to the lateral rectus muscle.
A recurrent meningeal artery (see Figure 11-1) might branch from the lacrimal artery and course back, leaving the orbit through the lateral aspect of the superior orbital fissure and then forming an anastomosis with the middle meningeal artery, a branch from the external carotid artery circulation.10 Other branches, the zygomaticotemporal artery and the zygomaticofacial artery, exit the orbit through foramina of the same name within the zygomatic bone (see Figure 11-1) and anastomose with branches from the external carotid in the temporal fossa and on the face.7
Posterior Ciliary Arteries
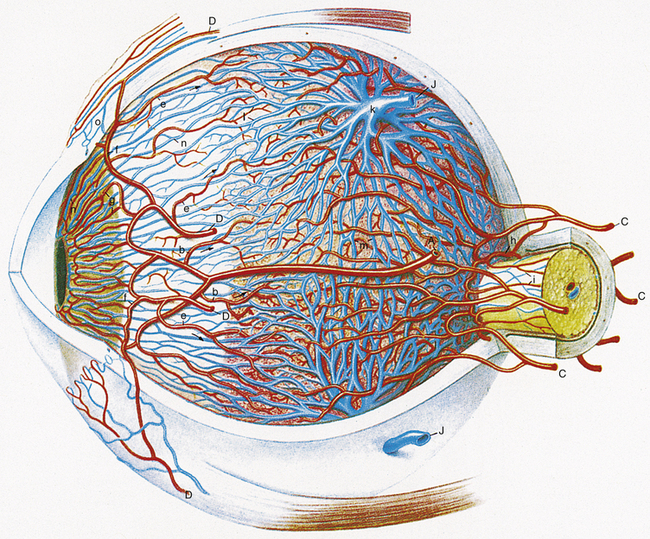
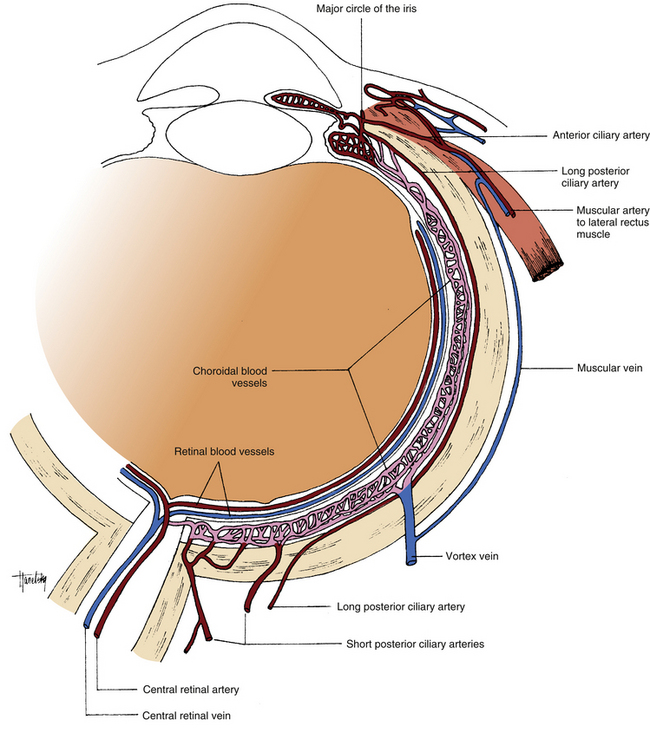
The posterior ciliary arteries are branches of the ophthalmic artery, and much variation can occur in their distribution.11 The short posterior ciliary arteries arise as 1, 2, or 3 branches that then form 10 to 20 branches. They enter the sclera in a ring around the optic nerve and form the arterial network within the choroidal stroma (Figure 11-3). Other branches from the short posterior ciliary arteries anastomose to form the circle of Zinn (Zinn-Haller) (see Figure 11-2), which encircles the optic nerve at the level of the choroid.12,13 The most superficial nerve fibers that occupy the surface of the optic disc are supplied by capillaries from the retinal vasculature with no apparent direct choroidal supply.13–15 The peripapillary network, formed by branches from the short posterior ciliary arteries and from the circle of Zinn, supplies the remaining prelaminar region of the optic nerve.14–17 These vessels do not anastomose with the peripapillary choriocapillaris.14 The laminar region is supplied by the short posterior ciliary arteries either directly or as branches from the circle of Zinn.14–18

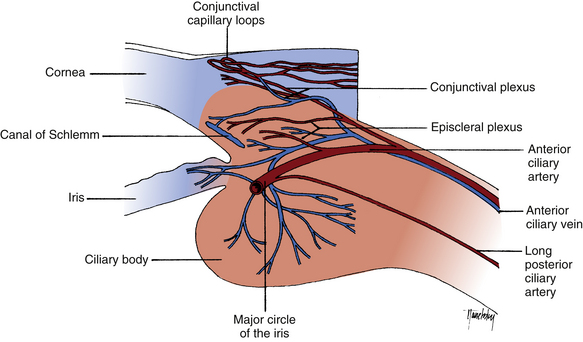
FIGURE 11-3 Uveal blood vessels.
(From Hogan MJ, Alvarado JA, Weddell JE: Histology of the human eye, Philadelphia, 1971, Saunders.)
Clinical Comment: Anterior Ischemic Optic Neuropathy
ANTERIOR ISCHEMIC OPTIC NEUROPATHY (AION) results from nonperfusion or hypoperfusion of the ciliary blood supply to the optic nerve head.14 The oval that forms the circle of Zinn can be divided into superior and inferior portions by the entry points of the medial and lateral short ciliary arteries forming it. This may be the anatomic basis for the altitudinal visual field loss that characterizes nonarteritic AION. The inferior field is more often affected, but there is no adequate explanation for the preferential involvement of the superior part of the ring of vessels.19
Clinical Comment: Cilioretinal Artery
A CILIORETINAL ARTERY may arise either from the vessels entering the choroid or from the circle of Zinn; thus this vessel, located within the retina, arises from the ciliary circulation and not from the retinal supply. Various studies report a cilioretinal artery occurring in 15% to 50% of the population and usually entering the retina from the temporal side of the optic disc to supply the macular area20,21 (Figure 11-4). If occlusion of the central retinal artery occurs, the direct blood supply to the macular area will be maintained in those individuals with such a cilioretinal artery.
Two long branches of the posterior ciliary arteries enter the sclera: one lateral and one medial to the ring of short ciliary arteries. These are the long posterior ciliary arteries, which run between the sclera and the choroid to the anterior globe (Figure 11-5). Here the arteries enter the ciliary body and branch superiorly and inferiorly.14 These branches anastomose with each other and with the anterior ciliary arteries to form a circular blood vessel, the major arterial circle of the iris (Figure 11-6). This circular artery is located in the ciliary stroma near the iris root and is the source of the radial vessels found in the iris. Before forming the major circle, branches from the long posterior ciliary arteries supply the ciliary body and the anterior choroid, where they form a network that anastomoses with the choroidal vessels from the short posterior ciliary arteries (see Figure 11-3).