Chapter 28 Oral health disorders
Introduction
Holistic dentistry is defined as the practice of dental medicine, the core principle of which is: oral health and the body’s health are intimately connected.1 Holistic dentistry focuses on the whole person and supports their physical, social, psychological, emotional and spiritual wellbeing. It is health promoting and emphasises lifestyle advice such as behaviour modification, dietary changes, stress management, exercise, appropriate sunshine exposure, environmental advice, and integrates appropriate complementary therapies where necessary to improve dental and oral health. Good communication and providing clear education guidelines to dental patients to promote good dental care, especially healthy behaviour patterns (e.g. regular teeth brushing and flossing) to encourage adherence to oral hygiene, is an important aspect of dental treatment.
Lifestyle factors, other than dietary factors, can play an important role in the prevention and management of oral health and dentists and health practitioners are in a unique position to reinforce lifestyle advice to complement dental care. Many dentists worldwide are already reinforcing the importance of maintaining good oral health through a healthy diet, regular brushing, teeth flossing and mouth washes. A small growing number of dentists in Australia and worldwide are practising holistic dentistry, however very few integrate complementary therapies that include acupuncture and homeopathy.1–4
Communication with dental practitioners
Communication plays an important role in the practitioner-patient relationship and contributes to positive health outcomes. Dentists who communicate with patients about their dental fears can help to significantly alleviate dental anxiety. A trial of anxious patients (n = 119) who completed Spielberger’s State Anxiety Inventory (STAI-S) pre- and post-treatment, were randomly allocated to intervention (dentist informed of anxiety score) and control (dentist not informed) groups. Communication was able to reduce the patients‘ level of anxiety and significantly reduce anxiety scores during dental procedure.5 The study concluded that providing the dentist with information regarding the high level of a patient’s dental anxiety prior to treatment and involving the patient with this, helped reduce the patient’s overall anxiety with dental treatment.
Relationship between oral and general health
What is less well recognised is that dental health may actually impact and affect physical health and medical diseases that can then go on to affect the rest of the body. A new growing body of evidence now suggests that oral health can potentially impact on general health.6 For example, periodontal disease appears to be associated with increased risk of cardiovascular disease (CVD).
Periodontal disease (PD) and risk of diseases
PD and CVD
Recent research suggests that PD may have a systemic effect and increase the risk of CVD, including coronary heart disease, myocardial infarction, peripheral vascular disease and stroke.6–11 The exact mechanism to explain this correlation is not clear, but may be linked to bacterial infections associated with PD and atherosclerotic plaque formation.12
PD and diabetes mellitus
There is also an association of PD with poorly controlled diabetes in patients with Type 2 diabetes mellitus (T2DM). Improved periodontal health may benefit diabetes and metabolic control in type 2 diabetes mellitus.13, 14, 15 For example, in a study, non-surgical periodontal treatment involving a full-mouth scaling and root planing led to a statistically significant improvement in plaque index, gingival index, probing pocket depth, clinical attachment levels and bleeding on probing, and improved HbA1c levels and glycaemic control in type 2 diabetic patients compared with the control group that received no periodontal treatment. Similarly, a recent randomised control trial (RCT) also demonstrated improved glycaemic control with periodontal treatment in type 2 diabetic patients.16 However, the difference in improved glycaemic control for type 1 diabetics was not as significant compared with control group following PD treatment.17 The benefits appear to be confined to type 2 diabetics.
Prevention
Tooth brushing
According to a Cochrane review of 42 trials involving 3855 participants, compared to manual toothbrushes, powered toothbrushes with a rotation oscillation action provides better protection against gum inflammation (gingivitis) and plaque removal.20
Chewing gum
Mastic or chewing gum can play an important role in prevention of caries. The benefits of chewing gum are based on its ability to stimulate salivary flow which helps promote food clearance from the mouth and reduce bacterial growth in saliva, such as Streptococcus mutans, and consequent plaque formation on teeth.21, 22 A study found the total number of bacterial colonies was significantly reduced during the 4 hours of chewing mastic gum compared to the placebo gum and significantly reduced plaque index and gingival index compared to the placebo group.23
Chewing gums containing sugar substitute products such as xylitol are very effective for preventing dental caries by stimulating the salivary flow, although an antimicrobial effect cannot be excluded. Xylitol appears to be superior to the other sugar alcohols such as sorbitol, mannitol, maltitol, lactitol and the products Lycasin and Palatinit for caries control. Xylitol is a polyol sugar alcohol and is naturally sourced from plums, strawberries, raspberries and rowan berries. A number of trials suggest xylitol is more effective than those sweetened with sorbitol for reduction of caries24, 25, 26 however, another review of all clinical trials concluded that chewing sugar-free gum 3 or more times daily for prolonged periods of time may reduce caries incidence irrespective of the type of sugar alcohol used. 27 Xylitol is not fermented by bacteria and causes a fall in plaque pH by having an inhibitory effect on mutans streptococci.
One study found a significant statistical reduction in the number of bacteria mutans streptococci found in saliva and plaque with a chewing program using xylitol-only chewing gums compared with xylitol-sorbitol chewing gum or control in 8-year old children over a 39-month period.28 Another study suggested a different mechanism for xylitol chewing gum benefit in preventing caries in children.29 This study demonstrated 5 grams of xylitol-containing chewing gums in children over a 14-day period reduced the glucose-initiated lactic acid formation in supragingival plaque by up to 22% compared with baseline and the control group. The authors concluded reducing lactic acid formation may play a more important role in reducing plaque formation, as the numbers of salivary mutans streptococci were unaffected in this study.29
Chewing gum combined with vitamin C
An RCT of chewing gum containing vitamin C (60mg) and gum containing vitamin C and carbamide (30mg + 30mg) were compared to placebo.30 A significant reduction in the total calculus score was observed after the use of vitamin C (33%) and vitamin C + carbamide (12%) gums compared with no gum use, especially in the heavy calculus formers. Vitamin C also reduced the number of bleeding sites (37%) and a reduced amount of visible plaque was observed after use of vitamin C and non-vitamin C gum. Carbamide added to vitamin C in chewing gum did not offer more benefit.30
Halitosis
Mouth rinses for halitosis
A Cochrane review of 5 RCTs found mouth rinses containing antibacterial agents such as chlorhexidine and cetylpyridinium chloride may play an important role in reducing the levels of halitosis-producing bacteria on the tongue, and mouth rinses containing chlorine dioxide or zinc can be effective in neutralisation of odoriferous sulfur compounds.31 However, there is sufficient evidence to suggest that alcohol-based mouth rinses should be avoided due to their association with oral and pharyngeal cancer, and should not be recommended.32–36
Sunlight
Sunshine is the main source of vitamin D produced by the body in response to direct skin exposure to ultraviolet B (UVB). Consequently, nil or minimal exposure to sun can contribute to vitamin D deficiency as seen in many community groups with dress codes (e.g. wearing veils), those living in geographically prone areas, especially over winter (southern or northern latitudes), those working indoors (e.g. office work), institutionalisation, prolonged hospitalisation and the bed-bound (e.g. stroke, elderly), and particularly in dark-skinned people who need longer sun exposure.38, 39 Vitamin D plays an important role in dental health (see the section on vitamin D below).
Environment
Mercury exposure
Dental amalgam is the most commonly used material in restorative dentistry. Dental amalgam is an alloy of silver, tin, copper and mercury.40 Mercury vapour absorption through the lungs (by dental practitioners or patients) or accidental oral ingestion of mercury from cracked teeth containing amalgams (by patients) are the main sources of mercury exposure in dentistry. The safety of mercury exposure from amalgam fillings has been explored in Australia.41 The findings of the National Health and Medical Research Council (NHMRC) working party concluded there was a lack of evidence to confirm dangers associated with mercury toxicity from amalgams and no studies exploring health outcomes amongst dental patients with and without amalgams and neurotoxicity. Based on current evidence, the NHMRC working party also concluded there is no role for removal protocols and concomitant therapeutic regimens, such as chelation therapy, for patients attributing symptoms to mercury from dental amalgam restorations. The NHMRC working party claim that the release of mercury is at a slow rate from dental amalgams, generally of a few micrograms per person per day among adults dependent upon variables such as number and shape of fillings, eating habits, and bruxism. For the current mean numbers of amalgam fillings in Australian children and adults (0.5 and 8, respectively), daily mercury absorption per person is about 0.3μg and 3.5μg, respectively, which is tenfold and twofold (respectively) higher than dietary sources of mercury retained in the body.19
However, there have since been more studies exploring effects of amalgam in children. A study of 507 children (aged 8–10 years) with at least 1 carious lesion on a permanent tooth and no previous exposure to amalgam were randomised to receive routine dental care during the 7-year trial period, 1 group receiving amalgam restorations (n = 253) and the other group receiving resin composite restorations (n = 254). Baseline mean creatinine-adjusted urinary mercury levels were 1.0–1.5mg/g higher in the amalgam group than in the composite group (P<0.001) at the 7-year follow-up. This study found no significant differences in measures of memory, attention, visuomotor function or nerve-conduction velocities for the groups over the 7 years of follow-up.42
A recent RCT of 534 children (aged 6–10 years) involving 5 community health settings compared neuropsychological and renal function of children whose dental caries were restored using amalgam or mercury-free materials.43 Children with no prior amalgam restorations and ≥2 posterior teeth with caries were randomised to receive dental restoration during a 5-year follow-up period using either amalgam or resin composite (non-amalgam) materials. The researchers found higher mean urinary mercury levels in children with amalgams at 5- and 7-year follow-up respectively but no significant differences in IQ, memory, attention/concentration and motor and visuomotor performance in either group.
Amalgam use in children and renal concerns
A study of 403 children in Shanghai found minimal differences in mean urinary mercury concentration for children with and without amalgam fillings, and no differences for either renal function biomarker, or on neurobehavioural, neuropsychological, or intelligence tests.44
However, in the New England Children’s Amalgam Trial there was a significantly increased prevalence of microalbuminuria among children in the amalgam group in years 3–5 (adjusted odds ratio [OR] 1.8; 95% confidence interval [CI], 1.1–2.9) compared with the composite group (p = 0.04) with no differences in levels of renal tubular markers — alpha1-microglobulin (A1M), gamma-glutamyl transpeptidase (gamma-GT) and for N-acetyl-beta-D-glucosaminidase (NAG).45 A sub-study of the New England Children’s Amalgam Trial collected 82 pairs of urine samples from children aged 10–16 years and found the creatinine-corrected excretions of albumin, gamma-GT, and NAG were significantly higher in daytime samples than in overnight samples, with a non-significant trend for A1M.46 Another study also found significantly higher levels of mercury in blood and urine and higher urinary excretion of NAG, gamma-GT and albumin in persons with dental amalgams than those without.47 Albuminuria and urinary excretion of NAG significantly correlated with the number of fillings. The authors concluded from:
… the nephrotoxicity point of view, dental amalgam is an unsuitable filling material, as it may give rise to Hg toxicity‘ and based on the mercury levels in blood and urine ‘renal damage is possible.47
There is considerable international controversy over the safety of mercury amalgam (fillings). In 2008, Norway, Denmark and Sweden totally banned the use of mercury products, including fillings, in their countries.48, 49, 50
Mercury in food
It is well recognised that mercury enters the food chain from naturally occurring mercury (as sulfides) or from air pollutants (e.g. industrial or vehicle exhaust pollution) deposited in sea, rivers and lakes and is transformed into methyl mercury by bacteria in the water. The methyl mercury is ingested by small fish and algae and consequently accumulates and builds up in larger and older predatory fish that are at the top of the food chain. Foods Standards Australia New Zealand (FSANZ) advises pregnant women, women planning pregnancy and young children should limit their intake of shark (flake), broadbill, marlin and swordfish to no more than 1 serve per fortnight with no other fish to be consumed during that fortnight due to risks of mercury toxicity.51 Those at risk of mercury toxicity are children, the unborn infant of pregnant women and newborns who are breastfeeding (exposure via the breast milk) from mothers who frequently (more than once a week) eat large predator species of fish. The developing nervous system of a fetus and children are particularly susceptible to the ill effects of high methyl mercury levels that can cause a multitude of symptoms such as nausea, vomiting, lack of appetite, weight loss, kidney failure, skin irritations, respiratory distress, swollen gums, mouth sores, neurological symptoms such as paraesthesia, numbness, seizures, tremors and incoordination, and mental retardation.52
Conclusion on mercury
Concerns associated with direct mercury toxicity via accidental inhalation and ingestion are real. Amalgams may be best avoided in pregnant women and young children, especially those with kidney disease or renal impairment, although there are very few studies exploring long-term health concerns. Dentists and dental health practitioners may also be at risk, although there are strict guidelines for discarding solid waste from lost or extracted teeth with amalgam fillings and amalgam-contaminated waste, which are carefully contained and in most instances incinerated. Proper collection of mercury-contaminated solid waste using high-frequency suction (while wearing a mask) prevents the release of mercury vapour during combustion. The use of rubber dams stops contaminated saliva secretions and amalgam debris from entering the oral cavity of the patient, minimising mercury exposure.53
Cadmium (Cd) exposure
Periodontal disease
Environmental cadmium (Cd) exposure is known to adversely affect bone remodelling and is associated with higher odds of periodontal disease. Analysis of data from the 3rd National Health and Nutrition Examination Survey (NHANES III) of 11 412 participants included in the study found 15.4% of participants had periodontal disease with a mean urine Cd concentration significantly higher among participants with periodontal disease [0.50; 95% CI, 0.45–0.56] compared with participants without periodontal disease [0.30; 95% CI, 0.28–0.31].54 After adjusting for tobacco exposure, there was a further significant threefold increase in creatinine-corrected urinary Cd concentrations from the 25th (0.18 mug/g) to the 75th (0.63 mug/g) percentile associated with a significant 54% greater risk of prevalent periodontal disease (OR = 1.54; 95% CI, 1.26–1.87).
Smoking
Cigarette smoking, cigar and pipe use in smokers significantly increases the risk of developing a range of dental health problems, including increased risk of caries, gingivitis, tooth loss, ulcer formation, oral cancers and PD.55 In general, smokers are 4–20 times more likely to develop periodontitis compared with persons who never smoked and, amongst current smokers, 74.8% of their periodontitis was attributable to smoking.56, 57 Smoking is a major preventable risk factor for PD and chronic destructive PD.
Smoking can adversely affect dental health by various mechanisms, such as defects in neutrophil function and host defences from nicotine leading to bacterial invasion and plaque formation, impairment of inflammatory and immune responses, increased alveolar bone loss, pocket formation and attachment loss, including adverse local and systemic effects (e.g. heart and lung disease).58, 59 Smoking also reduces wound healing following local trauma and dental treatment.
Smokers are also exposed to various chemicals and heavy metals, such as cadmium and lead from cigarette smoking, which are associated with PD and may aggravate existing renal impairment.60
Smoking cessation can significantly reduce the risk of PD and increase the likelihood of tooth retention but it may take decades for this to happen.61
Sleep and dental pain
Oral pain that impacts on sleep is a common presentation to dentists. Other than oral pain, dentists may also be confronted with pain from orofacial and temperomandibular junction (TMJ) disorders. Pain is well known to disrupt numerous aspects of normal physical and psychological life, including work, social activities and sleep.62, 63, 64
Mind–body therapy
Dental anxiety
Dental anxiety is a common problem. High dental anxiety can be overwhelming for an individual and is strongly associated with poor oral health, particularly due to treatment avoidance. Studies of 272 adult private dental practice patients were assessed for anxiety, frequency of oral health care visits in the last 10 years and their preferred method to alleviate anxiety.65
Mind–body techniques such as cognitive behaviour therapy (CBT), self-help techniques, relaxation and music therapy and exercise can be useful and effective for the management of panic and fear [see Chapter 4, anxiety].66, 67, 68 Many of these techniques can also help address psychological symptoms associated with dental anxiety and fear.
Psychological interventions — general
A Cochrane systematic review identified 4 studies that assessed psychological interventions aimed at increasing compliance of oral hygiene in adult patients with PD.69
Brief relaxation and music distraction
A prospective RCT compared a brief relaxation method with music distraction and a control group.70 Ninety patients with dental anxiety were randomised to either of the 3 groups. Both brief relaxation and music distraction reduced dental anxiety significantly. Brief relaxation was significantly superior to music distraction over the control group. Patients in the control group demonstrated no significant change in anxiety level.
A trial of 44 adult subjects requiring surgery for root canal treatment procedure were randomised to a music group, which listened to selected sedative music using headphones throughout the root canal treatment procedure, or a control group where subjects wore headphones but without the music.71 Heart rate, blood pressure and finger temperature were measured before the study and every 10 minutes until the end of the root canal treatment procedure. The level of anxiety experienced by the patient was measured before the study and at the end of the treatment procedure. The results revealed that there were no significant differences between the 2 groups for baseline data and procedure-related characteristics, except for gender. The music group showed a significant increase in finger temperature and a reduction in anxiety score over time compared with the control group. The authors concluded the findings:
Virtual image audio-visual eyeglass system
Virtual image, audio-visual (AV) eyeglasses may play a role in dental anxiety and pain. In a study of 27 patients, the participants completed a Dental Fear Survey and the Fear of Pain Questionnaire-III before dental treatment.72 They were randomised to either watch and listen to a standard video using AV eyeglasses or not (control group). The AV eyeglass group demonstrated rescued anxiety and discomfort compared with control group. Patients showed a preference to use AV equipment compared to the traditional approach of no glasses and there was a significant reduction in treatment time in the first half of the dental procedure. Clinicians experienced no significant technical interference with their dental work by using the AV eyeglasses. The authors concluded AV virtual image eyeglasses may be beneficial in the reduction of fear, pain and procedure time for most dental patients.72
Hypnosis and dental anxiety
Pre-existing anxiety and cognitions about dental procedures can predict dental anxiety. Hypnosis may be helpful for some patients, but not all. A study found that patient characteristics such as hypnotisability, trait anxiety and negative cognitions can predict which people develop dental anxiety and who will be more responsive to hypnosis.73 Rapid hypnotic induction techniques by oral health practitioners (dentists or dental nurses) can be useful for treating anxious patients prior to procedures.74 Children may be more receptive to hypnosis. A double-blind, control trial of 29 children (ages 4–13) were randomised to both hypnosis group and a no hypnosis group before a local anaesthetic injection for a dental procedure.75 Each subject was evaluated during utilisation of hypnosis before injection, and once without. Subjects were videotaped during the procedure and behaviour rated independently by 2 paediatric dentists, using the North Carolina Behaviour Rating Scale (NBRS). They found hypnosis significantly reduced pulse rate and crying, especially in the 4–6 year-old children.
Behavioural therapy for dental fear
Behaviour therapy may offer more benefit in reducing dental fear compared with hypnosis. In a study with 22 women (mean age of 31.8 years) who suffered dental fear and avoided dental care (median time of 9.5 years), participated in a clinical study and were randomly assigned to 1 of 2 groups; hypnotherapy (HT) versus behavioural treatment based on psychophysiological principles (PP).76 Both therapies involved 8 sessions followed by standardised conventional dental test treatments. Pre- and post-treatment measures were dental fear, general fear, mood, and patient behaviour. PP group statistically significantly reduced dental fear and improved mood during dental situations compared with HT group. General fear levels insignificantly reduced. Overall 11 of the 22 patients completed the conventional dental treatment without complications, indicating that they were more relaxed during the treatment.
Relaxation oriented therapy (ROT) versus cognitively oriented therapy (COT)
A study of 112 adults that were found to be fearful of dental treatments reported that those who received COT by a trained psychologist prior to specialist care were more likely to complete the treatment program, but those who received ROT were more likely to experience significantly less generalised anxiety and fear, and dental fear during the procedure.77 Dropouts were related to lower motivation (willingness to engage in dental treatment), and failed treatment was related to higher levels of general fear and anxiety. This study concluded that both COT and ROT interventions were effective in helping to reduce dental phobic reactions and to complete dental care, and that motivation was a significant predictor of treatment outcome.
An additional study compared ROT and COT with nitrous oxide sedation (NOS). Sixty-five patients with severe dental fear were randomly assigned to COT, ROT or NOS over 10 weekly sessions of individual therapy.78 Overall there were low dropout rates. All patients who completed the therapy sessions completed dental treatment and anxiety scores on dental fear tests significantly reduced in all treatment groups. There were no major differences between each group or with the advent of any serious adverse events. Furthermore, on following up these participants at 1 year after initiating the trial with 62 patients, it was reported that 95% of the participants had attended dental treatment with continued favourable effects with respect to dental fear and general distress. The relaxation group established the greatest reductions on the dental fear measures.79 All patients judged the 3 interventions namely, COT, ROT and NOS as beneficial for dental fear. Of the participants, 80% judged the treatment given in the year after the dental fear treatment as successful and all 3 treatment groups scored in the normative range for general distress both at the end of treatment and at follow-up.
In a further 5-year follow-up study of 43 patients, it was observed that the majority (81%) of the participants assessed the dental fear treatment they received 5 years previously to have been useful for dental fear and general psychological distress for participants in all 3 treatment groups.80
Diet
It is well established that nutritional intake plays a vital and significant role in oral and bone health. A number of reports have demonstrated that poor nutrition significantly affects teeth during development, exacerbates PD and dental diseases, craniofacial development (from in utero), risk of oral cancer and oral infections.81, 82
Dairy intake — calcium and vitamin D
Low dietary calcium intake is associated with reduced bone mass and increased risk of osteoporosis. Best sources of calcium foods include dairy products (milk, yoghurts and cheese), fish (sardines with bones), green leafy vegetables and fruits. The recommended dietary allowance for calcium is 800mg/day.83 Vitamin D deficiency is associated with rickets in children, osteoporosis; osteomalacia (reduced mineralisation of bone) and is common in the elderly and dark skinned people. The best source of vitamin D is from sun exposure. (Refer to Chapter 30 on osteoporosis for more information on calcium and vitamin D.)
Early childhood caries (ECC)
Data from the Third National Health and Nutrition Examination Survey (NHANES III) of 2- to 5-year-old children, found those consuming best dietary practices (uppermost tertile of the Healthy Eating Index [HEI]) were 44% less likely to exhibit severe ECC compared with children with the worst dietary practices (lowest tertile of the HEI).84
Sugars
Dental caries are more prevalent if sugars are consumed more frequently, particularly if retained in the mouth for long periods of time.85 Sucrose forms glucan in the mouth that facilitates firm bacterial adhesion to teeth and limits diffusion of acid and buffers in the plaque.
Soft drinks
Five to 6 servings per week of soft drinks, particularly cola, are recognised as a risk factor and linked to low bone mineral density and osteoporosis according to a population study of over 2500 adults.86 The harmful effects of soft drinks on general, dental and oral health are well confirmed.
Acidic diet and caries
It is well recognised that an acidic diet promotes caries. A study of 309 children’s diets found that large consumption of high-acidic beverages (e.g. fruit juices), vinegar, fruit, vitamin C supplements with low consumption of water and milk is associated with increased risk in caries and erosion.87 A recent Australian study investigated the erosive potential of beverages in schools.88 This study found that the majority of the tested beverages sold from school canteens exhibited erosive potential.
Table 28.1 lists the acidity of common drinks. A pH less than 5.0 should generally be reduced or avoided. Water and milk are preferred drinks to maintain good oral health.
Table 28.1 Acidity of common drinks
| Beverages | Acidity pH |
|---|---|
| Water | 7.0 |
| Milk | 6.8 |
| Flat mineral water | 5.3 |
| Soda water | 5.1 |
| Apricot yoghurt | 5.1 |
| Beer and/or wine | 4.0 |
| Sparkling mineral water | 3.9 |
| Orange juice | 3.6 |
| Apple juice | 3.4 |
| Diet coke | 3.0 |
| Ribena | 2.8 |
| Lemonade and Fanta® | 2.7 |
| Powerade | 2.7 |
| Coca cola® and Pepsi® | 2.3 |
| Vinegar | 2.2 |
| Lemon juice | 2.0 |
Nutritional supplements
Vitamins
Vitamin D
Vitamin D has a pivotal role in bone metabolism, it controls intestinal calcium absorption plus its deposition into bone.89 The main source of vitamin D is sunlight exposure (see Figure 28.1). Ninety percent of vitamin D is produced in the skin from sunshine exposure (UVB) with only 10% from dietary sources. Dietary sources include fatty fish (e.g. mackerel), cod liver oil, sun-exposed mushrooms and liver. The majority of women with osteoporosis have vitamin D deficiency and resulting bone loss.90 The Geelong Vitamin D Study on postmenopausal women found that the majority of the participants were vitamin D deficient during winter.91
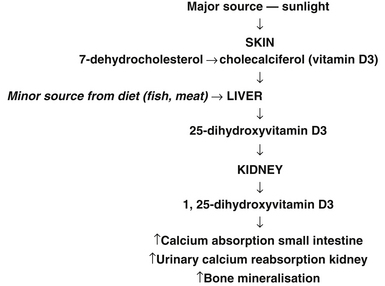
Figure 28.1 Major sources of sunlight
(Source: adapted from Nowson CA, Diamond TH, Psco JA, et. al. Australian Family Physician. 2004;33(3):133–8)
Vitamin D deficiency is likely to be the commonest nutritional deficiency in many countries, and may well be the most important one.92–97 Risk factors for vitamin D deficiency include dark skin colour, dress codes (e.g. wearing veils), migrants, infants of migrant families, living in geographical prone areas, especially over winter (southern or northern latitude), institutionalisation, bed-bound, intellectual disability, prolonged and exclusive breastfeeding, restricted sun exposure, and certain medical conditions. Vitamin D deficiency has re-emerged as a public health issue particularly affecting infants and young children, potentially causing hypocalcemia, seizures, rickets, limb pain, tooth loss and poor dentition and risk of fracture.98–104 Breastfed infants of mothers who were vitamin D deficient during pregnancy were at high risk of vitamin D deficiency.105
A position statement released recently by the Australian and New Zealand Bone and Mineral Society and Osteoporosis Australia and the Endocrine Society of Australia is summarised in Figure 28.2.106
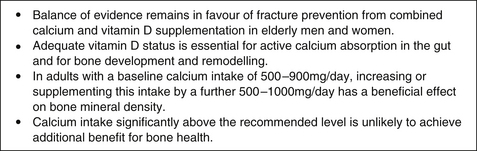
Figure 28.2 Position statement: calcium and bone health
(Source: Australian and New Zealand Bone and Mineral Society and Osteoporosis Australia and the Endocrine Society of Australia, 2009)106
Improved bone mineral density (BMD)
A large RCT of elderly people over a 5-year period demonstrated vitamin D combined with calcium supplementation has long-term benefit on BMD compared with calcium alone or control group, particularly in subjects with sub-optimal vitamin D levels.107 Moreover, it is well documented that throughout the lifecycle the skeleton requires optimum development and maintenance of its integrity to prevent fracture. The data is promising for the use of combined calcium with vitamin D and the use of vitamin K.108
Periodontal disease (PD)
Numerous articles indicate vitamin D and calcium deficiency are associated with bone loss and increased inflammation, which are well recognised symptoms of PD. Whilst studies suggest calcium and vitamin D may benefit periodontal health and calcium deficiency may be a risk factor for periodontal disease, there are no RCTs done to date to test this hypothesis.109
Vitamin D and calcium enhances tooth retention
A placebo-controlled trial of 145 healthy subjects aged over 65 years were randomised over a 3-year period to calcium or vitamin D supplementation to assess bone loss from the hip. Furthermore, participants were further followed up for 2-years after discontinuation of study supplements and teeth were counted at 18 months and 5 years.110 During the trial, subjects were less likely to lose 1 or more teeth (13%) whilst taking calcium and vitamin D supplements compared with a larger proportion of subjects (27%) whilst taking placebo. At the 2-year follow-up period, of those with total calcium intake >1000mg/day, 31 of 77 subjects (40%) lost 1 or more teeth compared with a larger proportion of 40 of 68 subjects (59%) who consumed less calcium.
Recommended dosage is calcium citrate 800mg/day or calcium carbonate 1000mg/day.
Vitamin B complex
Vitamin B may help wound healing post-surgery for PD. A randomised, double-blind, placebo-controlled trial of 30 patients with moderate to severe chronic periodontitis found that vitamin B complex at a dose of 50mg/day supplementation, in combination with surgery for 30 days following access flap surgery for PD, resulted in significantly better wound healing and clinical attachment levels up to 180 days compared with placebo and surgery.111
During the decades of the 1980s and 1990s several case reports of peripheral neuropathy associated with high-dose pyridoxine appeared in the scientific literature, where the consumption in most of the reported cases was of dosages that ranged from 1–5g per day.112 Vitamin B6 is usually safe at intakes up to a maximum of 200mg/day in adults for short-term supplementation. However, vitamin B6 can cause neurological disorders, such as loss of sensation in legs and imbalance, when taken in high doses (50 mg or more per day) over a long period of time. Vitamin B6 toxicity can damage sensory nerves, leading to numbness in the hands and feet as well as difficulty walking. Symptoms of a pyridoxine overdose may include poor coordination, peripheral neuropathy, staggering, numbness, decreased sensation to touch, temperature, and vibration and tiredness for up to 6 months. It is important to note though that there is a requisite to avoid overuse of single vitamin products (e.g. oral and injectable forms of vitamin B6) or concomitant use of multivitamin products that could lead to some patients routinely exceeding the upper limit for vitamins and hence risk severe toxicity.113
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


