FIGURE 68-1 Inappropriate shock for supraventricular tachycardia. Misclassification by the morphology discrimination algorithm is seen due to clipping (inset) of the electrogram. (Reproduced with permission from Hayes DL, Asirvatham SJ, Friedman PA. Cardiac pacing, defibrillation and resynchronization: a clinical approach. 3rd ed.: Wiley-Blackwell; 2012.)
EXPERT OPINION
The arrhythmia seen is an SVT. The device compares the morphology of the far field EGM during tachycardia with that of a template stored during normal rhythm and finds that eight of the last eight complexes do not “match.” The far field electrogram records the EGM between the pulse generator and the right ventricular coil, although other vectors are programmable. In contrast, the near field electrogram records the signal between the right ventricular tip and ring (or tip and coil) and generally contains less morphology information.
Since the morphology during tachycardia does not match the template, the device classifies the rhythm as ventricular fibrillation (VF) and delivers therapy. On closer examination, the top of the EGM appears to be “cut-off,” or in other words, truncated. Figure 68-2 shows clipped and unclipped EGMs from the same patient. Saturation of the amplifiers results in clipping of the EGM that distorts the EGM resulting in misclassification of the SVT by the morphology algorithm as a VT with subsequent inappropriate shock delivery.
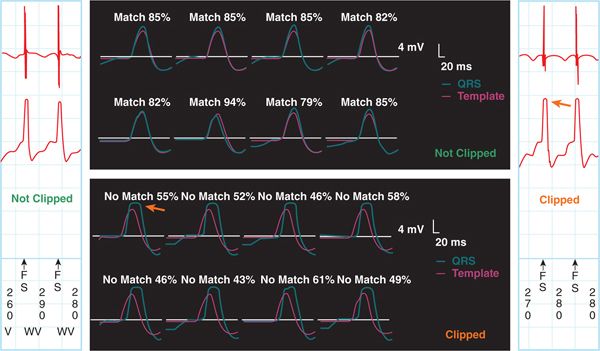
FIGURE 68-2 Morphology error due to clipping. Unclipped electrograms are shown on the left and top. (Left) The top electrogram is the near field channel, the bottom electrogram is far field, and the markers are at bottom. The letters “WV” indicate that SVT is diagnosed by the wavelet algorithm and therapy withheld. The electrogram matches with that of the template, and the rhythm is classified appropriately as SVT. (Right) Shown is the clipped electrogram. Clipping results in distortion of the electrograms, which do not match with that of the template (bottom) despite no physiologic change in the signal itself. It can be prevented by reprogramming the dynamic gain. (Reproduced with permission from Hayes DL, Asirvatham SJ, Friedman PA. Cardiac pacing, defibrillation and resynchronization: a clinical approach. 3rd ed.: Wiley-Blackwell; 2012.)
SVT-VT discrimination algorithms are designed to prevent inappropriate therapy for SVT. Morphology algorithms compare EGMs during tachycardia to a template acquired during normally conducted rhythm. If the tachycardia EGM differs from the template by more than a programmed threshold, the rhythm is classified as VT. Morphology is the only noninterval based single chamber algorithm for SVT-VT discrimination, and it is generally the most accurate. However, misclassification can occur due to truncation of EGM as seen in this case. This can be avoided by adjusting the amplitude gain so that the sensed EGM falls within 25% to 75% of the dynamic range. Other causes of morphology misclassification include:
• SVT with rate related aberrancy. To prevent this, a template can be acquired during atrial pacing at a rapid rate (eg, 120 bpm) and template updates disabled.
• Errors in alignment of EGM.
• Myopotential distortion of the EGM. This is a unique situation in which noise on the far field signal can result in inappropriate shock.
• Changes in morphology over time due to lead maturation or bundle branch block. These can be avoided by periodic automatic updating of the template.
• Recurrent arrhythmia shortly after shock delivery. The EGM is often distorted in the minutes immediately following shock delivery. While morphology is not applied during redetection, if an episode terminates and a new arrhythmia develops, the algorithm may be applied before physiologic recovery of the EGM.
UNNECESSARY VERSUS INAPPROPRIATE SHOCK
Delivery of ICD shock for rhythms other than ventricular tachycardia (VT) or VF is termed “inappropriate shock.” Recent studies have shown that programming the device to delay shocks for nonsustained VT or VF and programming antitachycardia pacing (ATP) can improve outcomes. The term “unnecessary shock” encompasses inappropriate shocks and therapy delivered for VT that would have responded to ATP or self-terminated given time. Optimal programming of ICDs prevents unnecessary shocks.
PROGRAMMING TO PREVENT UNNECESSARY SHOCKS
The detection and treatment of arrhythmia by an ICD involves a series of steps, each of which provides an opportunity to minimize shocks (Figure 68-3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree