, Kyu Eun Lee1 and June Young Choi1
(1)
Department of Surgery, Seoul National University Hospital, Seoul, Korea, Republic of (South Korea)
Abstract
The operating theater is prepared as a non-sterile atmosphere and all instruments are manipulated to carry out the operations in sterile environments. There are two assistants to assist the operator and a scrub nurse. The operation setting is as below.
Electronic supplementary material
The online version of this chapter (doi:10.1007/978-3-642-37262-9_2) contains supplementary material, which is available to authorized users.
2.1 Basic Equipment and Instruments of Open Thyroidectomy
2.1.1 The Operating Theater
The operating theater is prepared as a non-sterile atmosphere and all instruments are manipulated to carry out the operations in sterile environments. There are two assistants to assist the operator and a scrub nurse. The operation setting is as below.
Fig. 2.1
The operating theater of open thyroidectomy
2.1.2 Thyroid Pillow (Emtas, Seoul, Korea)
Thyroid pillow is made for stable and comfortable positioning of patient.
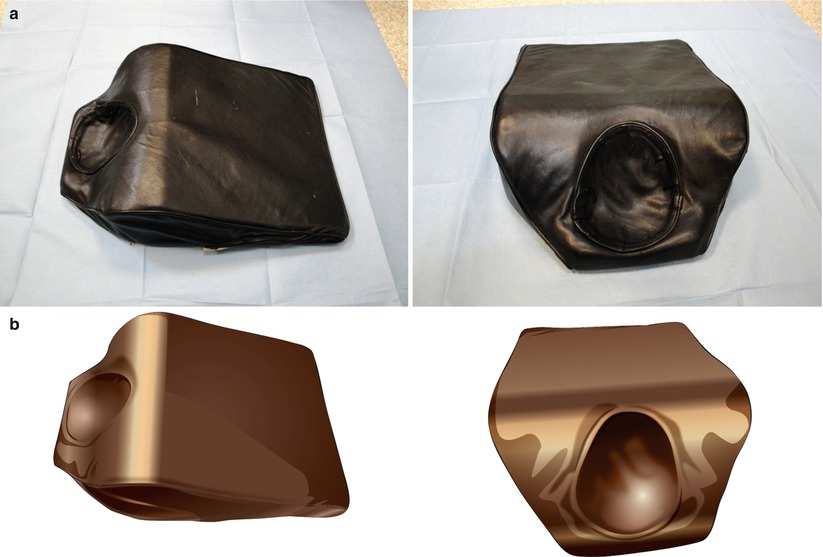
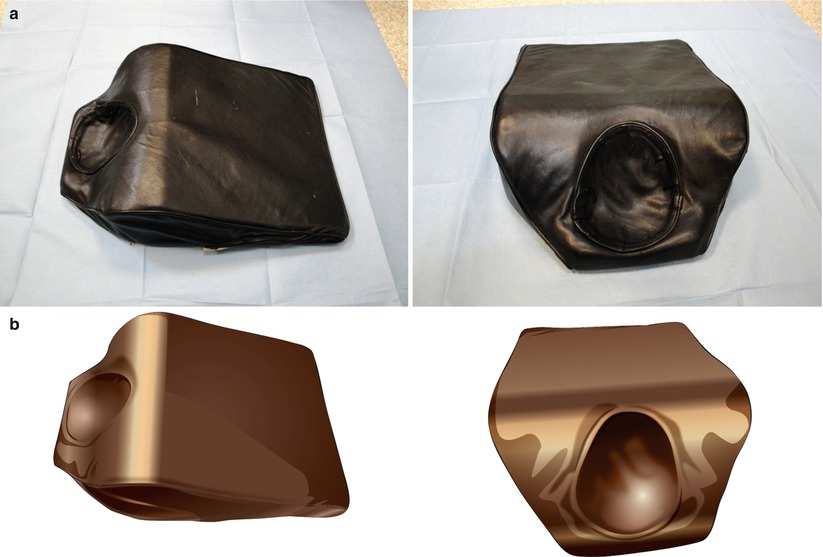
Fig. 2.2
Thyroid pillow. (a) photos, (b) illustrations
2.1.3 Harmonic® (Ethicon Endo-Surgery)
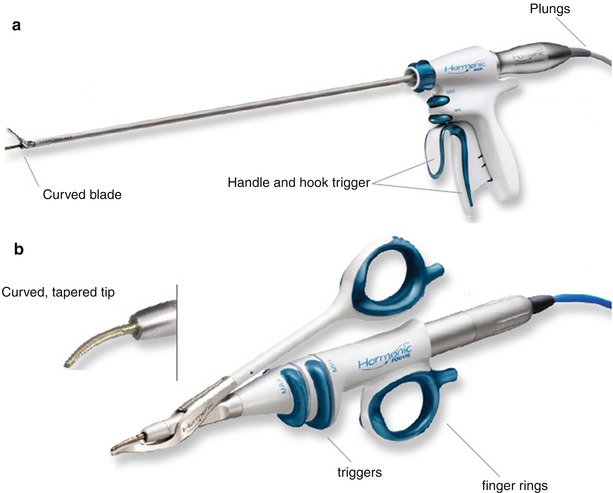
Fig. 2.3
Harmonic®. (a) Harmonic Ace, (b) Harmonic Focus
2.1.4 Basic Instruments
1.
Retractors: Army-Navy retractor, Cushing (or Middeldorpf) retractor, and deep Cushing retractor
2.
Metzenbaum, Mixter clamps, right-angle clamps, mosquito hemostats, peanut, Allis clamps, Adson tooth forceps, Potts forceps, needle holder, and thyroid clamps
3.
Bovie electrocautery
4.
Jackson-Pratt drain
2.2 Patient Preparation
2.2.1 General Considerations
Most preoperative evaluations of patient take place on an ambulatory basis. Those preoperative evaluations are required to be checked before admission by the surgeon at the outpatient clinic. Patients with significant comorbidity should be evaluated by referring an anesthesiologist before the operation. Most patients are admitted 1 or 2 days before the operation. After admission, preoperative examinations of patient are reexamined by the surgeon and further examinations such as computed tomography and US-guided marking can be done preoperatively.
2.2.2 Education and Informed Consent
The surgeon should educate and inform patient about the potential risk of a neck scar, recurrent laryngeal nerve injury, hypocalcemia, bleeding, pain, possibility of transfusion, reoperation, and other alternatives available before the operation.
2.2.3 Diet Restriction and Fluid Supplement
NPO past midnight is recommended for all patients before thyroidectomy. This standard order is based upon the belief of reduction of gastric contents and acidity. In general, at least 6 h of cessation of solid food and 2 or 4 h of cessation of fluids are required. Intravenous fluid supplement is given 2–3 h before induction.
2.2.4 Skin Preparation
Preoperative skin preparation of patient is required to prevent surgical site infection (SSI). Skin preparation can be performed with an antiseptic solution according to the routine maneuver of each center.
In male patients, shaving off a beard is required. Hair removal can be accomplished with electric clippers or shaving solutions rather than with a razor to avoid skin injury.
In patients for endoscopic and robotic surgery, shaving of axillary hair is also required before the operation.
2.3 Procedures of Open Thyroidectomy
2.3.1 Patient Positioning
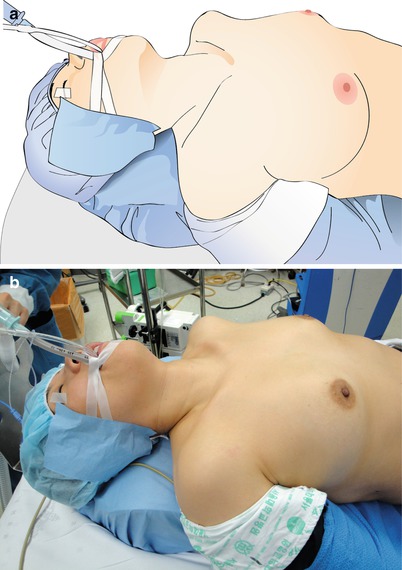
Fig. 2.4
Position of patient. (a) illustration, (b) photo
The patient should be placed in the supine position on the operating table with the arms tucked close to the side. A folded sheet or a thyroid pillow is placed vertically under the patient’s shoulders to extend the head and neck.
This neck extension should be performed with great caution and with the assistance of the anesthesiologists to ensure that endotracheal tube is secured and the neck is not overextended.
It is helpful to have the operating table placed in a reverse Trendelenburg position to decrease the cervical venous pressure.


Fig. 2.5
An adhesive tape to cover both ears and hairs
The patient’s hair may be covered with a mesh cap to avoid contamination of the field. An adhesive tape may be applied to cover up both ears.
2.3.2 Skin Preparation and Draping
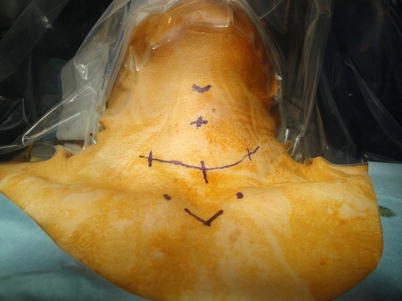
Fig. 2.6
Draping of the operative field
The operative field is then prepared with a routine surgical maneuver.
The anterior cervical region is prepared bilaterally from the angles of the mandible, posteriorly to the anterior borders of the trapezius, and inferiorly over the anterior chest wall to the line between the nipples.
When the surgical prep solution is completely dry, the operative field is defined with disposable operative drapes.
We cover the patient’s head and face with a transparent plastic sheet that is made adherent to the skin to see through the patient’s face and the endotracheal tube.
And a large sterile drape is covered over the patient’s shoulder, anterior chest wall, and lower body to complete the draping.
2.3.3 Skin Incision and Dissection
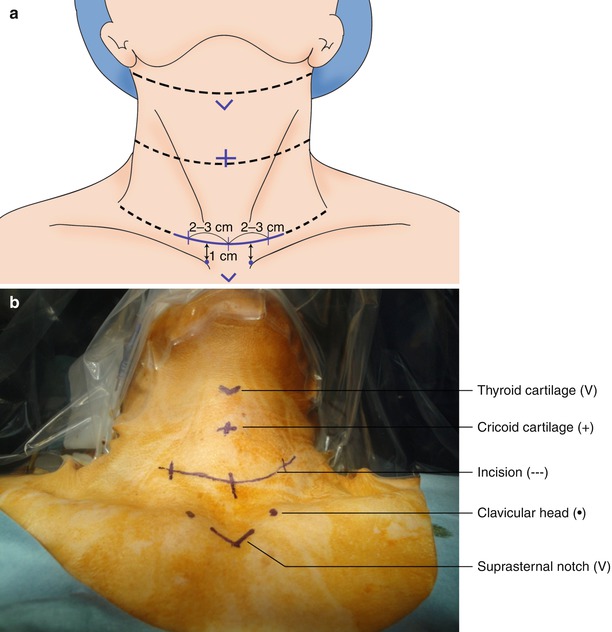
Fig. 2.7
Landmarks and incision. (a) illustration, (b) photo
After marking the landmarks as illustrated, a transverse skin incision is made approximately a fingerbreadth above the suprasternal notch. We make 4–6 cm long incision for thyroidectomy. Longer incision should be made in patients with large goiters or nodules.


Fig. 2.8
Adhesive film to protect skin
We apply transparent adhesive film (Tegaderm®) on the incision to protect the skin from excessive strains and electrocautery burns.


Fig. 2.9
Flap dissection (superior part)
Carry the incision down to the platysma muscle. This muscle is easier to identify in the lateral portions of the incision. When the longitudinal fibers of this muscle are seen, transect them with precision because the upper flap will be dissected in a plane along the deep aspect of the platysma. Two or three Allis clamps are placed on the fascia of the platysma to retract the flap vertically while countertraction with the operator’s finger exposes a natural bloodless plane. If the plane of dissection is carried down to the cervical fascia, a number of anterior jugular veins are encountered that can produce unnecessary bleeding. Blood staining of tissues may complicate the operation unnecessarily, so care should be taken to leave a thin layer of fat on these veins.
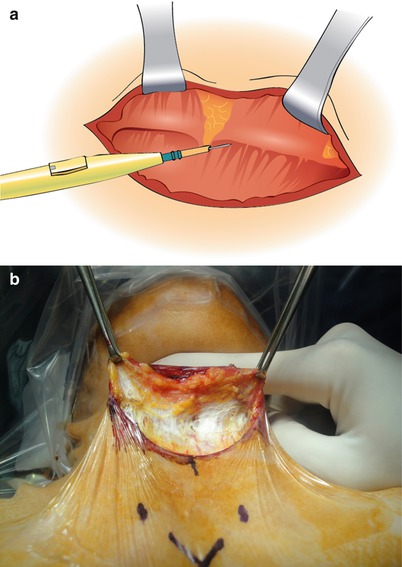
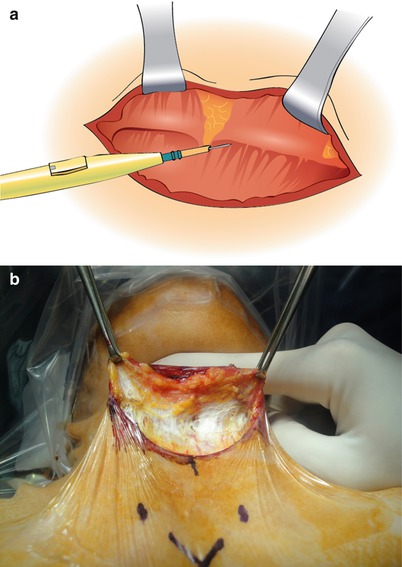
Fig. 2.10
Flap dissection (continued). (a) illustration, (b) photo
Electrocautery can be used to create flaps in this subplatysmal plane superiorly to the uppermost aspect of the thyroid cartilage in the midline.
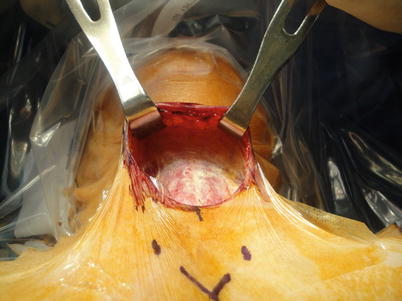
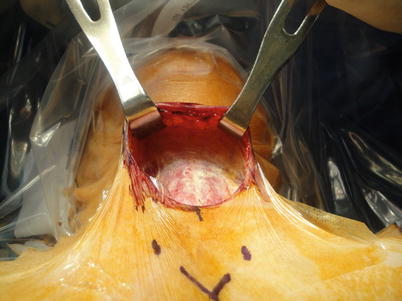
Fig. 2.11
Completed flap dissection
Then the lateral portions of the flaps are developed. Adequate exposure can be obtained with wide dissection of these subplatysmal musculocutaneous flaps. A blunt dissection using an operator’s finger or a peanut sponge is helpful to avoid unnecessary bleeding.


Fig. 2.12
Flap dissection (inferior part)
After the superior flaps are made, the inferior flaps are created to the level of the suprasternal notch and the clavicular heads.
2.3.4 Midline Incision and Isthmectomy
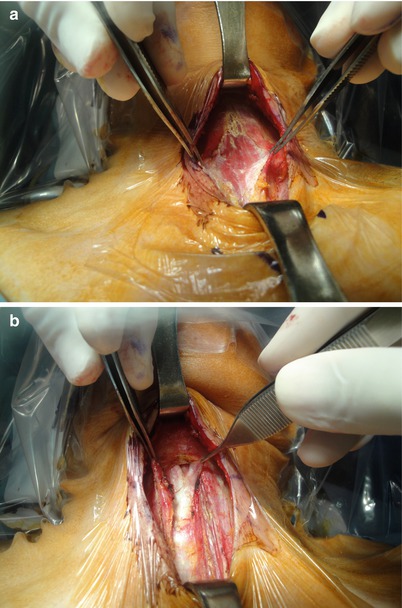
Fig. 2.13
Division in the midline. (a) Division between the strap muscles, (b) exposure of the trachea after isthmectomy
The midline is best identified by palpating the prominence of the thyroid cartilage and the trachea. The cervical fascia is opened in the midline from the thyroid cartilage to the suprasternal notch to expose the full length of the strap muscles. The sternohyoid muscle and underlying sternothyroid muscle are also separated in the midline from the thyroid cartilage to the suprasternal notch. When the midline incision is made, the isthmus of the thyroid gland will be visible, and as the next step, the fatty tissue inferior to the isthmus is divided to identify the trachea. At this point, great care should be taken not to injure the trachea. The isthmus is then divided in the midline with the electrocautery or the ultrasonic sheers (the HarmonicⓇ). The operator should make sure that there is no lesion in the isthmus before the isthmectomy by preoperative ultrasound or computed tomography. Isthmectomy can give more room in the operative field, and dissection of the posterior surface of the thyroid off the trachea enables better mobilization of the gland to the medial part.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


