Learning Objectives
- Describe nutrition problems around the world: their extent, causes, and manifestations
- Identify the signs and symptoms of micronutrient deficiencies and understand approaches to addressing these deficiencies
- Describe key interventions for malnutrition in various settings: in developing countries, during complex humanitarian emergencies, and in the context of HIV/AIDS and tuberculosis
- Identify some tools for measuring malnutrition and distinguish between growth monitoring and rapid emergency assessment
- Describe how national and international policies can shape nutrition strategies and approaches. Give examples of potential beneficial and adverse effects of such policies
Introduction
During the past few decades we have become increasingly aware of the central role that nutrition plays in all aspects of population health. We have recognized that access to adequate nutrition is a human right since the promulgation of the Universal Declaration of Human Rights in 1948, as stated in Article 25: “Everyone has the right to a standard of living adequate for the health and well-being of himself and of his family, including food ”[emphasis added]. Although it may seem intuitively obvious that such access is also a basic human need, there is value in reviewing the biologic factors that inform our understanding of this. We will come back to a more detailed discussion of these concepts later in this chapter, but keep these two fundamental truths in mind while reading the following pages. In addition, we wish to introduce another concept for you to consider while reading this chapter; all of the major causes of death of the people of this globe, be they living in high-income, middle-income, or low-income countries, are inextricably linked to the nutritional environment in which they find themselves.
The Global Context
In a century characterized by modern approaches to identifying and solving global health problems, undernutrition prevails in the world’s children, contributing to a third of all deaths in children under 5 years of age.1 An estimated 195 million children under 5 years in developing countries are stunted in growth (height-for-age), and some 120 million are wasted (weight-for-height).2 Overall, 80% of the world’s undernourished children live in just 20 countries around the world, according to the World Health Organization (WHO).3 In addition, a third of the developing world suffers from micronutrient deficiencies—deficiencies that accompany poor nutrition and are silent until their effects are advanced and, in some instances, irreversible. In these settings, infections, such as human immunodeficiency virus (HIV), tuberculosis (TB), and parasites, intensify the impact of undernutrition, and vice versa.
We can define direct causes of undernutrition as primary undernutrition, caused by inadequate food intake, or secondary undernutrition, caused by underlying diseases such as TB or HIV/AIDS. In addition, there are many indirect causes of undernutrition: poverty, the low status of women, unsanitary health conditions, wars and conflict, low national income growth, as well as poor governance and corruption. Factors underlying poor health services are human, economic, and organizational resources and their control. This is one reason that undernutrition can be seen in conflict-affected areas or in areas where a local governing authority does not have the will, the commitment, or the effectiveness to carry out services for a population. Political ideologies, ethnic discrimination, and marginalization of the poor can create pockets of undernutrition in countries where abundant nutritional sources are inequitably allocated. However, not all undernutrition is seen in developing countries or in complex humanitarian emergencies. Consider inner cities, where food may not be accessible (the “food deserts” seen in disadvantaged neighborhoods), not affordable due to poverty, or where lack of knowledge about (and unavailability of) good nutritional choices leads to poor selection of foods and poor eating habits. At the time of this writing, it is conservatively estimated that 14% of the population of the United States, in isolated rural areas as well as disadvantaged urban areas, is either chronically or intermittently food insecure if not actually malnourished.4 The U.S. Department of Agriculture (USDA) Supplemental Nutrition Assistant Program (SNAP), commonly referred to as the food stamp program, supplies food purchasing support to 46 million people each month (14.6% of the total population as of 2012),5 and various state food banks report serving between 12% and 14% of the population within their respective states.6 A somewhat disturbing set of statistics applies to the elderly population in the United States. According to one study, 18% of elderly patients living in long-term facilities were severely undernourished, with 27.5% mildly to moderately undernourished.7 Prevalence in the hospitalized population is even more alarming, varying between 40% and 60% depending on the study cited.8
Respected leaders throughout history have pointed out that one of the most meaningful measures of a society is reflected by how they treat their most vulnerable members. We should keep this in mind as we learn more about the statistics of preventable morbidity and mortality as they relate to our children and senior citizens.
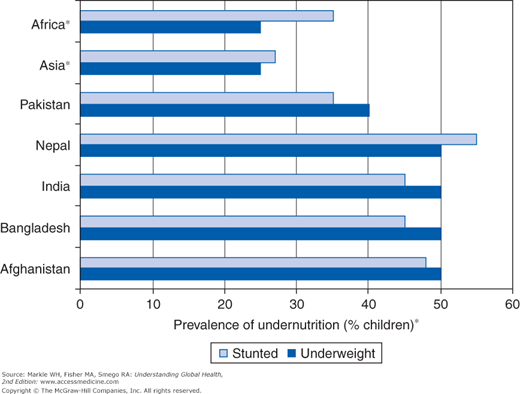
Where in the developing world does undernutrition remain a problem for 21st-century populations? The countries of South Asia (India, Bangladesh, Afghanistan, and Pakistan) have both high numbers and high rates of undernourished children, with India leading the list. In fact, although undernutrition is decreasing in Asia overall, the prevalence of undernutrition in South Asia (41% to 43%) is much higher than that in sub-Saharan Africa (SSA; 25%) (Figure 7-1).9 In SSA, undernutrition is a major contributing factor in over 60% of deaths of children under the age of 5 years, with pneumonia and diarrhea accounting for the highest percentage, closely followed by perinatal causes. Other infections, specifically TB, HIV/AIDS, and malaria, account for the rest.10 For Africa, it is estimated that 25% of children 5 years or younger are underweight (moderate to severe), and some 34% are stunted.11
Figure 7-1.
The prevalence of undernutrition in South Asian countries is much higher than in Africa. From World Bank. Repositioning Nutrition as Central to Development: A Strategy for Large-Scale Action. Washington, DC: World Bank, 2006. (Reproduced with permission.)
*Estimates are based on WHO regions.
Populations, and children in particular, do not die of undernutrition per se, but of infectious diseases that would generally not be fatal to well-nourished individuals. They are vulnerable to these infections because of the direct effects undernutrition has in weakening the natural defenses of the immune system (they are compromised hosts), as well as the indirect effects of having poor access to health services, poor sanitation, unsafe water supplies, and ignorance of basic health care practices. Poverty and lack of education exacerbate and prolong undernutrition. Although poverty is the ultimate underlying problem, the resultant undernutrition leads to possibly irreversible loss of each individual’s potential due to damage to physical and intellectual capacity, and the lack of education adds to this synergistically, resulting in a severe loss of the development of human capital. Thus a vicious cycle is created. Poor feeding practices and lack of adequate nutrition result in poorly nourished children; if they survive to be of reproductive age, they are likely to be poorly nourished parents. Stunted mothers can give birth to low-birth-weight babies. Undernutrition in the mother can result in major damage to a child’s health and well-being, much of which is irreversible, manifesting as less physical capacity, lowered intelligence, and more frequent illnesses. Those factors may result in irregular school attendance or diminished ability to learn, and ultimately in lower likelihood of employment, lowered productivity, and inability to meet the daily economic demands of life. Because this can be a generational phenomenon in households and communities, it is a difficult cycle to break. These children and adolescents rarely escape the cycle of poverty and despair into which they are born.
It is this inability of people suffering from chronic food insecurity and undernutrition that is fundamental to the loss of human capital that defines the so-called poverty trap. Jeffrey Sachs, in his book The End of Poverty,12 notes that extreme poverty occurs when there is a lack of six types of capital, starting with human capital. It is for this reason that we suggest, if indeed a poverty trap exists, chronic hunger and undernutrition are the locks on that trap. Stated another way, acknowledging that the ultimate problem underlying inequities in global health today is that of poverty, hunger is surely its cruelest manifestation.
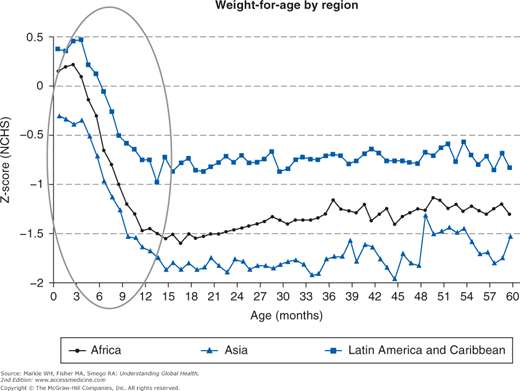
Graphs of undernutrition (weight-for-age by region) show that undernutrition happens early in life (Figure 7-2).13 Studies demonstrate that for younger children, the risk of dying increases exponentially with degree of undernutrition.14 As children get older, however, the degree of undernutrition drops off in part because younger undernourished children have died and in part due to the fact that older children are better able to fend for themselves in an environment of scarce resources. In other words, younger children are more represented in the data showing undernutrition.
Figure 7-2.
Malnutrition happens early. From Shrimpton R, Cesar G, et al. The worldwide timing of growth failure; implications for nutritional interventions. Pediatrics 2001;107(5):e75. NCHS, National Center for Health Statistics. Circled area represents a window of opportunity. (Reproduced with permission.)
Although there is some debate in the nutrition literature as to the temporal and causative relationship between undernutrition and mortality in any specific population, there is general agreement that this relationship is an exponential one. That is, as the severity of undernutrition increases, mortality rates increase exponentially rather than linearly, explaining the alarming increases in mortality we see as food insecurity evolves into overt famine. Where low rates of undernutrition exist, high mortality rates in children of refugee populations can be explained by acute illnesses such as acute diarrhea and dehydration when access to adequate infrastructure is lacking. In populations where public health services and stable home environments are able to support the necessary infrastructure, higher rates of undernutrition can be weathered when severe food insecurity and famine occur. High mortality rates can mask deteriorating nutrition status because they can occur for reasons other than undernutrition. This is only true when under-5 death rates are very high—more than 10 per 10,000 per day. Some nongovernmental organizations (NGOs) have developed models to characterize whether a situation is a food crisis, a health crisis, or a combination of both (emergencies out of control).
One solution to undernutrition begins with preventing and treating undernutrition in pregnant women and in children up to 2 years of age. Providing health and nutrition education along with micronutrient fortification and supplementation is also very important. Contrary to popular perception, school feeding programs do not intervene soon enough, although they may draw children into school and keep them there.15
In the introduction to this chapter we made mention of the concept that all of the major causes of death of the world’s population are causally related to the nutritional environment, and that the term malnutrition, although historically understood to be synonymous with undernutrition, includes the spectrum of physiologic deviations from the norm caused by overnutrition. When we incorporate this insight into the calculus of our policy decisions and widen the scope of concern in a global sense, we recognize that malnutrition is not limited to developing countries. Its presence, as the recognized biometrics of overweight, obesity, and morbid obesity, has become epidemic in developed nations, most readily apparent in poor urban slums and underserved rural areas. Sedentary lifestyle, dietary excesses, high-fat content in food, and consumption of the empty calories in processed and fast foods lead to overnutrition and obesity. These diets can also be marginal in certain nutrients; stunted growth coupled with excess body fat can be the result. The increasing stress levels of modern life have also resulted in rising morbidity and mortality. Data from the Centers for Disease Control and Prevention (CDC) indicate that nearly two thirds of the U.S. population is either overweight or frankly obese.16 To put this into perspective, consider the fact that in 1990 obesity prevalence rates in the United States for adults varied from less than 10% to 14%. In the year 2000, those numbers had increased to 15% to 25%, and in 2010, the numbers had increased to between 20% to over 30% depending on the registry we examined.17
Obesity is defined using body mass index (BMI) as a metric for maladaptive fat storage. BMI is calculated as body weight in kilograms divided by height in meters squared. Acceptable BMI varies by age and gender (Table 7-1). Some 17% of children and adolescents in the United States between 2 and 19 years old are considered obese.18 Since 1980, obesity prevalence has tripled for children and adolescents between 2 and 19 years of age.19 In 2005, the Institute of Medicine called these trends a “harmful upward trajectory.”20 Many factors are strong predictors of childhood obesity: genetics (having overweight parents), childhood characteristics (having been overweight in middle childhood), psychosocial factors (such as depression), and behavior (such as eating while watching TV and lack of regular exercise). Of specific interest, a number of studies have demonstrated a clear link between childhood obesity and the presence of a television in the child’s bedroom.21
The marked increase in the prevalence of obesity just noted is accompanied by parallel increases in deaths due to noncommunicable chronic disease, such as cardiovascular disease, diabetes, stroke, and cancer, all of which are linked to excess calories, saturated fat, salt (sodium), cholesterol, and sugars, along with inadequate fiber intake. Dietary factors also are linked to higher risks for hypertension, dental and renal disease, and osteoporosis.
We have developed our understanding that there is a difference between the specific diseases that cause the morbidity and mortality due to undernutrition or overnutrition. We can now give consideration to a distinction between diseases of infrastructure and diseases of affluence. What do we mean by this?
Most of this chapter deals with the physiologic consequences of undernutrition, and as we have discussed, undernutrition weakens a person’s ability to fight off infectious diseases that would, under normal circumstances, be reasonably well tolerated (i.e., the person becomes a compromised host). Coupled with this poor access to adequate nutrition in impoverished regions we see overcrowding due to inadequate living quarters and a lack of access to safe water supplies and adequate sanitation facilities. This creates what we might think of as a “perfect storm”; not only is the population compromised in their ability to fight off infection, but also people are more likely to encounter pathogenic organisms through exposure to contaminated water supplies and/or contact with infected individuals. Because of this association between undernutrition, on the one hand, and these communicable diseases related to inadequate public health facilities, on the other, we can consider these diseases to be diseases of infrastructure. (The proximate examples of infrastructure given here are, of course, only a part of a more complex infrastructure including issues of economic development and governance.)
At the other end of the spectrum of nutritionally related diseases, we have seen the exponential growth of the prevalence of obesity in middle- and high-income nations, with its associated chronic metabolic diseases. All of these are major risk factors for the development of coronary artery disease, explaining why coronary artery disease is the major cause of death in both men and women in developed nations. Due to this association of higher rates of obesity-related metabolic diseases and higher levels of income, we can refer to these diseases as diseases of affluence.
Paradoxically, overnourished populations have the greatest access to information and approaches that would increase their health and well-being, suggesting that populations in developed nations are as at much risk of suffering the ill effects of unhealthy nutrition due to poor choices as are populations in developing nations due to poor access. To counter food advertising and the convenience of fast foods, public health messages promote awareness of better food choices and lifestyle. Package labeling, media campaigns, and social marketing have led to some increased nutrition awareness among the public as well as among health care providers. However, food availability and affordability, ethnic preferences, and levels of education and income still negatively influence these choices.
Many low- and middle-income countries are caught in a situation referred to as nutritional transition. These countries face simultaneous public health challenges: undernutrition in some populations and obesity in others, along with diet-related noncommunicable diseases, such as cardiovascular disease, cancer, and diabetes. This phenomenon can be very costly for countries because it presents competing priorities for limited health budgets and health personnel, who may still be grappling with programs to combat traditional communicable diseases.9 The prevalence of obesity tends to follow a bimodal distribution in these countries, becoming evident at first in the more well-to-do members of the population, but invariably having a greater prevalence in the poor.22
Over- and undernutrition can coexist not only in the same country but also in the same household. In Mauritania, more than 40% of mothers are overweight while at the same time more than 30% of children are underweight. As many as 60% of households with an overweight person also had an underweight person.9
In the introduction to this chapter we presented the argument that access to adequate nutrition is a human right and a basic human need. If we accept Article 25 of the Universal Declaration of Human Rights (and subsequent contemporary documents such as the Millennium Development Project [MDP]) as our moral authority for stating that access to adequate nutrition is a human right, to what authority do we turn to assert that access to adequate nutrition is a human need?
In 1943, Abraham Maslow, considered the father of humanistic psychology, published his seminal article on his theory of human motivation.23 Commonly known as Maslow’s hierarchy of needs, he pointed out that there were five levels of human development, starting with physiologic needs, and then advancing through issues of safety, love and belonging, self-esteem, and self-actualization. Although there is significant detail to be learned about each of these levels of individual growth, a critical point to be understood about this concept is that one cannot advance to the next level of personal development until the needs of the level below are met. In other words, if the basic needs of the physiologic level are not met, and this includes access to adequate nutrition, one can never advance along the continuum of personal growth, and therefore never realize one’s full potential. To quote Maslow, “For the man who is extremely and dangerously hungry, no other interests exist but food. He dreams food, he remembers food, he thinks about food, he emotes only about food, he perceives only food and he wants only food. (This) allow(s) us to speak … of pure hunger drive and behavior, with the one unqualified aim of relief.” In the following sections we discuss the physiologic consequences of inadequate intake of calories, protein, and certain micronutrients, but we should always consider these issues in the context of the physical and psychological suffering associated with chronic hunger.
Protein-Energy Malnutrition
In an introduction to any discussion of an unhealthy diet, it is important to say a few words on what is considered to be a healthy diet. Basic caloric needs depend on age, gender, body size, and activity level, but calories alone are not sufficient. A proper balance of calories from the macronutrient carbohydrates, fats, and proteins is critically important in growth and maintenance, as is the intake of sufficient amounts of the micronutrient vitamins and minerals. The first publicly published accounts of what would be considered a balanced diet appeared in 1974 in Sweden as a food pyramid, with most of the calories (55% to 75%) being supplied by unrefined carbohydrates, 15% to 30% being supplied by fats, and 10% to 15% supplied by protein. A similar food pyramid for the United States was published in 1992. More recently, the USDA has replaced the food pyramid with My Plate, a divided plate that not only offers suggestions as to a balance of macro and micronutrients, but also offers advice on what would be considered healthy choices (e.g., whole grains and fresh fruits and vegetables, lean meats for proteins, and fat-free or low-fat calcium-rich dairy products.) In this section we describe the effects of undernutrition of these food groups and certain micronutrients, with the reminder that overnutrition (especially too much intake of calorically dense fats and oils) can be just as damaging to one’s health, albeit for different reasons.
Throughout this chapter we have been using the terms undernutrition and overnutrition, as we have become increasingly aware of the fact that overnutrition is as costly a form of malnutrition as undernutrition in terms of health outcomes. Traditionally, however, malnutrition has been understood to mean undernutrition, and very specifically undernutrition due to inadequate intake of the macronutrients carbohydrates, fats, and protein. For this reason, undernutrition has been referred to as protein-energy malnutrition (PEM). When the body’s basic maintenance needs for the caloric energy found in carbohydrates or fats, or the basic building blocks (amino acids) found in protein, exceeds its dietary intake of them, undernutrition is the result. People develop PEM for many reasons, such as inadequate food intake, poor composition of the diet, and unclean environments (poor hygiene), diarrhea, and infections. Children are especially vulnerable due to their increased needs during periods of growth and development as well as their dependence on others to help them meet those needs.
To understand the pathophysiology of the different forms of PEM, we need very briefly to review the basics of nutrition. The energy we need to grow and maintain our own bodies, and to perform the functions of life, are obtained through the ingestion of calories. (A calorie is defined as the amount of energy required to raise the temperature of 1 cubic centimeter of water 1 degree Centigrade. When we refer to dietary calories, we are actually talking about a kilocalorie, or 1,000 calories. This is usually written as Calorie, although conventional usage tends to omit the capital “C.”) Most of our caloric needs is met by the ingestion of carbohydrates (sugars and starches), which supply 4 calories per gram, and fats (mostly triglycerides), which supply 9 calories per gram. Proteins are a special case. They also supply 4 calories per gram, but because humans can only synthesize 10 of the 20 naturally occurring amino acids needed to make our own internal proteins, we normally use only about 25% of ingested protein for energy. The remaining 75% is recycled. We use the amino acids in ingested proteins that we cannot synthesize (the essential amino acids) to synthesize our own protein in order to preserve the integrity of our internal environment. When diets are lacking in adequate high-quality protein (that containing adequate amounts of the essential amino acids), a particularly pernicious form of undernutrition occurs (see later). This explains why we have referred to undernutrition as protein-energy undernutrition.
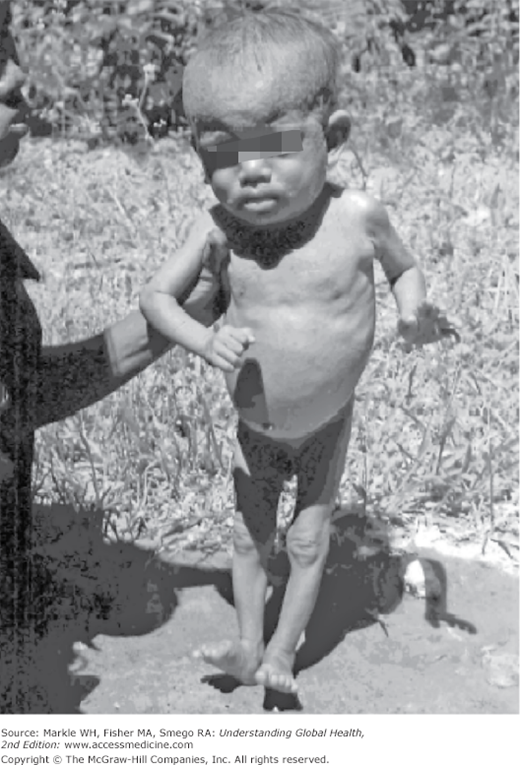
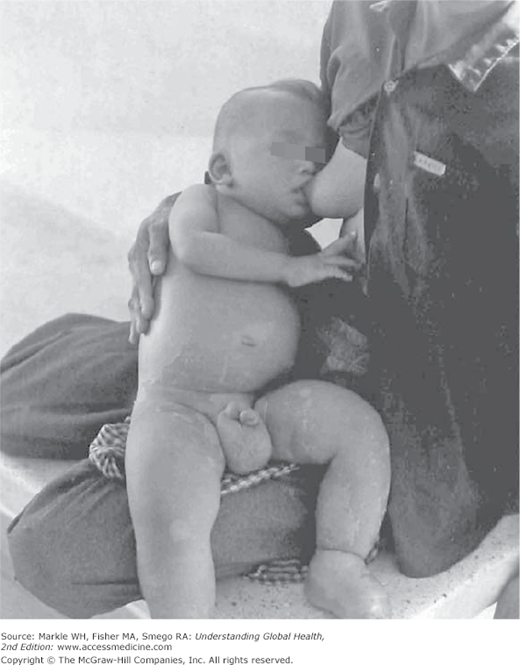
Classically, three types of PEM have been described: marasmus, kwashiorkor, and marasmic kwashiorkor.
Marasmus (the term comes from the Greek word for “withering”) is due to prolonged caloric deprivation or frank starvation. It is characterized by severe wasting of fat and muscle, which results in an old-person skin-and-bones appearance (Figure 7-3). This is the most common form of PEM seen in nutritional emergencies where food shortages are severe. In contrast to the relative anorexia seen in children with kwashiorkor (who may be getting enough calories but not enough protein), children with marasmus are hungry. Marasmus may also be the result of chronic or recurring infections with decreased food intake.
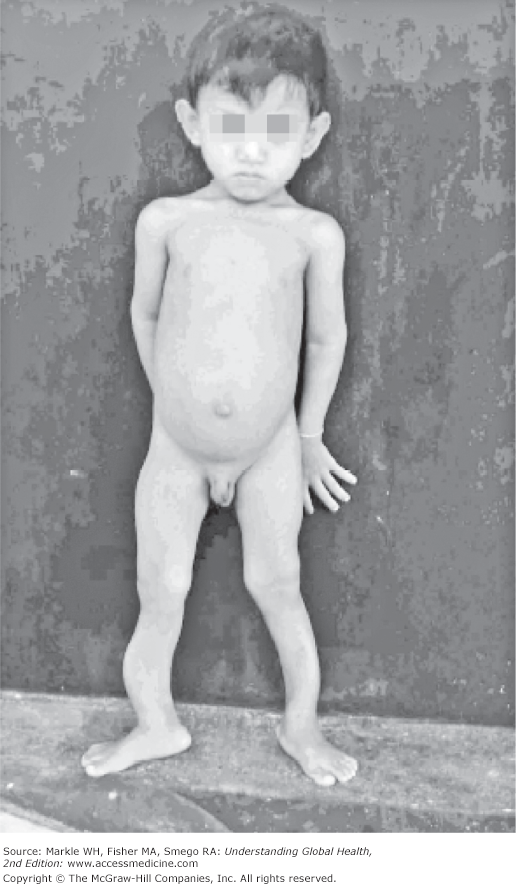
Kwashiorkor comes from the Ghanaian term meaning “the sickness that the older child gets when the next baby is born”; the older child is displaced from breastfeeding by the newborn, who is offered the breast first. The older child is left to forage from the family table or may be given complementary foods for which he or she is not yet ready. Because breast milk is frequently the only source of high-quality protein available in these settings, the child quickly becomes protein deficient and unable to synthesize his or her own internal proteins for normal body function. One of these proteins is the albumin found in blood plasma. Due to the resultant hypoalbuminemia, kwashiorkor is accompanied by edema, mostly in the feet and legs, along with flaky skin, sparse light-colored (even red) hair, apathy or irritability, and poor appetite. Because of the edema, children may look “fat” and appear to be well fed to the untrained observer or to the parent who is not aware of the silent effects of undernutrition in their child. Children with severe kwashiorkor may have hair that falls out easily and skin that looks burned or ulcerated and peels easily (Figure 7-4). In addition, they may have cardiac, renal, and gastrointestinal failure due to their inability to adequately maintain the protein in their internal organs. The third form of PEM, marasmic kwashiorkor, has both wasting and edema.
Chronic PEM has both short-term effects, such as lowered resistance to infections, and long-term effects, such as growth retardation, reduced intellectual development, and increased death rates, especially among children 1 to 5 years old, who are more vulnerable to respiratory infection and diarrhea. These children are also more vulnerable to TB, which is highly prevalent in many developing countries. Undernutrition is closely associated with TB in developing countries and often is considered a clinical sign of TB because TB has an increased metabolic demand (as do many chronic diseases such as AIDS and cancer). Undernutrition can lead to immune compromise, which then sets the stage for an opportunistic infection. To quantify the degree of undernutrition, public health specialists and health care providers speak of wasting and stunting in terms of muscle mass (weight) and height, respectively. In children 6 to 59 months old, wasting (low weight-for-height [WFH]) is defined as more than 2 standard deviations (SDs), or Z scores, below the reference values set by the WHO or the National Center for Health Statistics (NCHS); the term excludes edema. Almost 25% of children younger than 5 years in developing nations suffer from wasting. This puts them at great risk for death or severe growth impairment and delayed psychological development. Populations in which 10% to 14.9% of children are wasted are said to have a high (serious) risk of death. Usually the crude mortality rates (CMRs) in those populations are 2 to 4.9 deaths per 10,000 per day. Populations that are considered critical have wasting percentages of 15% or higher; CMRs tend to be more than 5 deaths per 10,000 per day. The prevalence of wasting in any population is considered a good measure of acute undernutrition.
Stunting (low height-for-age) occurs when children fail to reach their linear growth potential. As with wasting, stunting is associated with poverty, poor feeding practices, and risk of illnesses. Its prevalence varies widely, from less than 5% (United States and Chile, for example) to 59% (Afghanistan), around the world. India alone has an estimated 61 million stunted children, accounting for 30% of all the stunted children under 5 years in the world. Stunting is a manifestation and long-term consequence of chronic undernutrition. Stunted children may never reach their full growth potential, even when nutritional interventions are introduced. The prevalence of stunting in any population is considered a good measure of chronic or past undernutrition.
Micronutrient Deficiencies
Micronutrients are vitamins and minerals required in very small quantities (micrograms or milligrams per day) for good health. For example, the average person requires only about one teaspoon of iodine during his or her entire lifetime. Because the human body does not produce most of these micronutrients, they have to be obtained from foods in the daily diet, as supplements added to food (i.e., food fortification), or in the form of capsules, powders, tablets, or injections. Although these micronutrients are only required in small amounts, the absence of any one of them will lead to severe disability and eventual death because they are important either as building blocks to grow and maintain our anatomy, or as critical cofactors in the basic biochemical reactions necessary for our physiology. Among the many micronutrients, the ones of greatest interest and importance are iron, iodine, and vitamin A, followed by zinc, vitamin D, and folic acid. Although deficiency of vitamin C (scurvy), vitamin B1 (beriberi), and vitamin B3 (pellagra) have in the past caused substantial morbidity and mortality in affected populations, they are relatively uncommon today (although not unheard of). Micronutrient deficiencies have several causes: poverty, poor diet, lack of clean water and adequate sanitation, illness, and malabsorption. Unlike PEM, micronutrient deficiencies may not be readily apparent. In fact, micronutrient deficiencies may be silent until major signs and symptoms appear. Fortunately, solutions to micronutrient deficiencies are relatively easy, inexpensive, available, and politically feasible.
Of the billions of people in the world, WHO and UNICEF estimate that some 2 billion are at risk for iron deficiency, 1.6 billion for iodine deficiency, and 0.8 billion for vitamin A deficiency. Each day some 300 mothers die in childbirth due to iron deficiency, 4,000 children die from the effects of vitamin A deficiency, and 50,000 infants are born with reduced mental capacity due to iodine deficiency.24 Correction of readily apparent macronutrient deficiency without recognition (and correction) of concurrent micronutrient deficiency can lead to acute syndromes of disabling, potentially irreversible morbidity, and mortality. Country-specific data on micronutrients as well as overall nutritional status can be found in Macro International’s Demographic and Health Surveys that collect and analyze data to monitor and evaluate populations, health, and nutrition programs.25
Iron deficiency is the most common micronutrient deficiency in the developing world and usually manifest by anemia. Anemia can also be seen in inflammatory processes, inherited disorders of hemoglobin, and deficiencies of vitamins A, B12, and folate. However, at least 50% of cases of anemia are due to iron deficiency. Iron deficiency can be caused by inadequate dietary intake, insufficient iron absorption, or periodic bleeding, as in menstruation. Anemia in women of childbearing age is defined as a hemoglobin concentration less than 12 g/dl (at sea level). The diagnosis of iron deficiency anemia is usually established by measuring the concentration of serum ferritin, iron, transferrin, or total iron-binding capacity.
Often the cause is poor nutritional intake and lack of adequate iron sources in the diet, although chronic occult blood loss due to intestinal parasites can contribute significantly as well. Early childhood and the childbearing years in women (due to monthly blood loss and sequential pregnancies) are the two most vulnerable periods in life for iron deficiency. Iron depletion in the full-term infant occurs by about 6 months of age and may be marked by age 1 year when anemia is apparent. The consequences of iron deficiency may be anemia, lowered immunity to fight infection, adverse pregnancy outcomes, reduction in work capacity or school performance, and behavioral and learning difficulties in the child.
Correction of iron deficiency can be a targeted intervention in which vulnerable populations are screened and then provided iron supplements, or it can be a universal approach in which everyone is given iron supplements in areas where iron deficiency anemia is prevalent. Routine iron supplementation for pregnant women is a standard practice in most of the world. Hookworm infection can account for a large portion of iron deficiency. In these instances periodic deworming programs, coupled with sanitation and hygiene practices, can decrease the worm burden in the local population. When nutrition education is added to such programs, including at the time of growth monitoring, better food choices and feeding practices can help communities to be self-vigilant and self-monitoring and less reliant on rescue micronutrients from outside providers. Promotion of exclusive breastfeeding, delayed introduction of tea water given to infants, and iron fortification of commonly consumed foods (e.g., flour, cereals) can make a difference in lowering the incidence of iron deficiency in the community.
When the prevalence of anemia among nonpregnant women of reproductive age is equal to or greater than 20%, WHO recommends a weekly regimen of 60 mg of elemental iron along with 2,800 micrograms (2.8 mg) of folic acid for all menstruating women. This weekly regimen should be taken for 3 months, followed by 3 months off treatment, in an alternating pattern.26 When the woman is anemic, she should take 120 mg elemental iron daily along with 400 micrograms (0.4 mg) of folic acid daily until her hemoglobin returns to normal. Then she should resume the intermittent regimen as described.26 Preschool children living in areas where the prevalence of anemia is equal to or greater than 20% should receive weekly 25 mg of elemental iron; school-age children should take 45 mg of elemental iron each week. If they are anemic, they should take elemental iron daily until their hemoglobin reaches normal levels. Where hookworm infection is higher than 20%, it is best to combine iron supplementation with antihelminthics in children older than 5 years. At least annual universal antihelminthic treatment should be administered, irrespective of infection status.27
Lack of iodine in the diet of a pregnant mother has several adverse effects on the growing fetus: it may result in stillbirth or infant death or may manifest as mild mental retardation or even cretinism, which includes severe brain damage, deafness, and dwarfism. Iodine deficiency reduces intelligence, education potential, and productivity. The average reduction in IQ is 13.5 points with iodine deficiency; in cretinism, this reduction is far greater.28
Iodine deficiency is the greatest cause of preventable brain damage in fetuses and infants, with over 130 countries and 2 billion people affected worldwide. If the allocation of iodine deficiency were visualized as a pyramid, it would show 2 billion people at risk at the bottom of the pyramid, 655 million with goiter, 26 million with brain damage, and 6 million with cretinism.
Iodine deficiency must be corrected before conception. This can be accomplished through food fortification, such as salt iodization. Major advances have been made over the last 15 years.29 In 1990, only 46 countries had iodized salt programs, whereas in 2007, 120 countries had such programs and 54 countries still had problems with iodine deficiency.30 Universal iodization of salt is a known safe way to control iodine deficiency for most of the world. The public health challenge is in getting the job done. Fortification also reduces the short-term effects on children and adults, such as lethargy and motor and mental impairment. Additional economic and social benefits include improved health and work capacity, improved efficiency of education, reduced health care expenditure, and improved quality of life.
Vitamin A deficiency affects about 19 million pregnant women and 190 million preschool-age children in over 90 countries, but mostly from the WHO regions of Africa and Southeast Asia.31 Some 40% of preschool children are estimated to be vitamin A deficient. Infants and children have increased vitamin A requirements to support rapid growth and to help them combat infections. Inadequate intake of vitamin A can result in vitamin A deficiency, which can be manifest as night blindness as the earliest sign, to increased morbidity and mortality from measles, diarrhea, and respiratory infections. Overall, 6% and 8% of deaths in children under 5 in Africa and Asia, respectively, are solely due to vitamin A deficiency. When vitamin A deficiency is combined with undernutrition, iron and zinc deficiencies, and inadequate breastfeeding, this combination accounts for 7% of under-5 deaths.
Vitamin A deficiency is the leading cause of preventable blindness in young children and increasingly recognized as a contributor to maternal mortality. Up to half a million children become blind each year due to vitamin A deficiency. Of those who develop blindness, half die within 1 year, in part because of their impaired ability to combat infection, particularly measles. Of the 190 million children with vitamin A deficiency, 13.5 million have night blindness, 3.1 million have xerophthalmia, and nearly half a million are blind.32 Clinically, there is dryness of the cornea and conjunctiva (xerophthalmia), with scars and ulceration, Bitot’s spots (keratinization), and ultimately keratomalacia. This is because vitamin A is used to regenerate epithelial cells including the retina.
Vitamin A deficiency is usually seen in community clusters, meaning that cases of xerophthalmia are surrounded by groups of affected mothers and young children. This phenomenon reflects community dietary practices and shared risks of undernutrition and infection. As children grow older, their tastes change, they are able to search more widely for food on their own, and they are less likely to have vitamin A lacking in their diet. Vitamin A deficiency may also be seasonal when dietary need is mostly supplied through vegetable sources, as availability may be high during harvest time but essentially absent during the months that just precede harvest.
Diarrhea, liver disease (hepatitis, cirrhosis), and intestinal infections with worms decrease the body’s ability to absorb vitamin A. The infection-undernutrition cycle is the downward spiral of decreased food intake, decreased nutrients, and decreased ability to fight infection. This is sometimes seen in cases of measles. Metabolic needs for vitamin A are higher during growth, infection, and pregnancy. Any kind of corneal ulceration, especially when associated with measles, is an indication to provide vitamin A immediately, on the presumption that vitamin A deficiency exists.
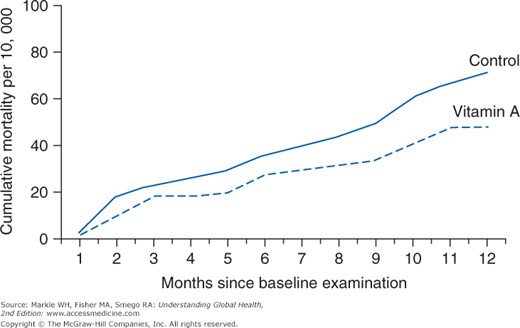
Treatment is urgent and not expensive. In the mid-1980s, research in Indonesia—the Aceh trial—demonstrated that 2 cents’ worth of vitamin A decreased child mortality by 34% (Figure 7-5).33 Studies between 1986 and 1992 from India, Nepal, and Africa confirmed that preschool mortality could be reduced by 25% to 30%. The Nepal Nutrition Intervention Project studied 44,000 rural women, half of whom were pregnant. Results showed that a weekly dietary supplement of vitamin A or beta-carotene could reduce maternal mortality by 40%.34 Public health surveys for night blindness and other manifestations of eye problems are one way of determining the prevalence of vitamin A deficiency in populations at risk. Trained interviewers and observers and large samples of children are necessary for such surveys. Among children younger than 5 years in SSA, about two fifths are at risk for vitamin A deficiency, and adequate vitamin A programs could avert 645,000 deaths each year. Vitamin A supplements can decrease infant mortality by 25%; reduce HIV-related morbidity, measles, and kwashiorkor mortality in children; and decrease maternal mortality by 40%. Vitamin A is often distributed at the time of immunization campaigns called national immunization days, as well as with other child survival interventions, such as deworming and nutrition education. Recent meta-analyses show that vitamin A does not alter seroconversion (antibody response) to measles vaccination, an important point because vitamin A is often co-administered at the time of measles vaccination.35 One way to prevent vitamin A deficiency is breastfeeding because breast milk is a rich source of vitamin A. Exclusive breastfeeding for the first 6 months is strongly recommended. Dietary counseling is important for mothers of children who are beyond the breastfeeding years.
Figure 7-5.
Mortality of 1- to 5-year-old children in vitamin A–supplemented versus control villages in Aceh, Indonesia, 1982–1984. From Sommer A, Tarwotjo I, Djunaedi E, et al. Impact of vitamin A supplementation on childhood mortality: a randomized controlled community trial. Lancet 1986;1:1169. (Reproduced with permission.)
Vitamin A occurs naturally in animal products (dairy, egg yolks, liver) as well as vegetable sources (palm oil, dark green leafy vegetables) and colored fruit (such as papayas and mangos) that are rich in carotenoids and beta-carotene. Vegetable sources of vitamin A are less bioavailable than animal sources, partly because the plant sources are provitamins that must be metabolically converted to the active form, but also because diets that are lacking in animal sources tend to have very little fat, and fat is necessary in the diet to facilitate absorption of this fat-soluble vitamin. Foods such as sugar, cooking oil, and flour can also be fortified with vitamin A. Children and women after childbirth can be given supplements for 6 months: 200,000 IU for children and 300,000 IU for the mother 4 to 8 weeks postpartum. Finally, dietary diversification can help guarantee that vitamin A is consumed in adequate amounts. UNICEF now supplies between 600 and 800 million 2-cent vitamin A capsules to more than 75 countries around the world, essentially covering some 300 to 400 million children each year.
High-dose vitamin A supplementation is recommended in infants and children 6 to 59 months of age in settings where vitamin A deficiency is a public health problem,36 and especially where night blindness prevalence is equal to or greater than 1%. Children 6 to 11 months old, including those who are HIV positive, should receive 100,000 IU once; children 12 to 59 months should be given 200,000 IU every 4 to 6 months.
In three settings vitamin A supplementation is not recommended by WHO: for newborns, for infants 1 to 5 months of age, and for HIV-positive pregnant women. Neonatal vitamin A supplementation and supplementation in infants 1 to 5 months of age is not recommended as a public health intervention to reduce infant morbidity and mortality.37,38 The quality of the available evidence for mortality-related outcomes was found to be moderate. Mothers should continue to be encouraged to exclusively breastfeed infants for the first 6 months to achieve optimal growth, development, and health. Vitamin A supplementation in HIV-positive pregnant women is not recommended as a public health intervention for the prevention of mother-to-child transmission of HIV, nor is it recommended for postpartum or pregnant women.39 It should be noted that concerns have been raised regarding increased progression to death for HIV-positive mothers and infants because of universal maternal or neonatal vitamin A supplementation in HIV-endemic areas.40
Zinc is an essential element for growth, in both humans and plants, and for proper immune function and mucosal integrity. Lack of zinc in the human diet increases risk for diarrhea, respiratory infection, and developmental delays. In its severe form, zinc deficiency is characterized by acrodermatitis, gastrointestinal discomfort, diarrhea, and slow growth.
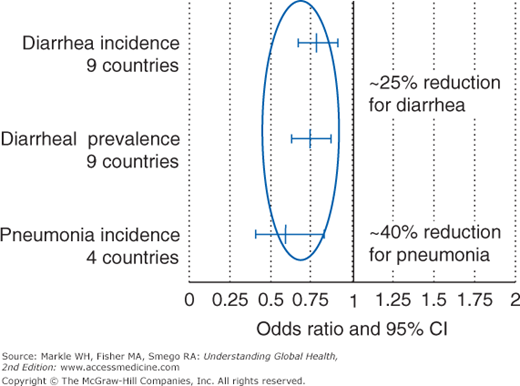
Many studies have demonstrated scientifically that daily zinc supplements reduce diarrhea and pneumonia in preschoolers (Figure 7-6).41 In addition, zinc supplementation (taken as 20-mg tablets) decreases the frequency and the volume output of diarrhea and shortens the time to recovery. The effervescent tablets can be dissolved in breast milk or oral rehydration solution. Zinc supplementation for 10 to 14 days has a preventive effect on childhood illnesses in the 2 to 3 months after treatment.
Figure 7-6.
Effects of daily zinc supplement use on diarrhea and pneumonia in preschoolers. From Zinc Investigators’ Collaborative Group. Prevention of diarrhea and pneumonia by zinc supplementation in children in developing countries: pooled analysis of randomized controlled trials. J Pediatr 1999;135:689–697. (Reproduced with permission.)
Zinc is found in breast milk, meats, and crustaceans. It is generally low in most vegetables, grains, and fish. Years of over cultivation of the soil and mismanagement of land can deplete zinc in the soil, leading to low zinc levels in plants, crop yields, and seeds, contributing to the deficiency cycle.
Vitamin D is needed for bone growth. Bone softening and ultimately rickets are the result of defective mineralization of growing bone—an imbalance of calcium and phosphorus. Nutritional rickets typically affects children younger than 2 years, during the period of rapid growth when demands for calcium and phosphorus are high. Vitamin D–deficient children will fail to thrive, be short in stature, be developmentally delayed, and have gait abnormalities (Figure 7-7).
Vitamin D deficiency can be prevented in all breastfed babies by the daily administration of 400 IU of vitamin D for the first 2 months of life. All formulas have at least 400 IU/L. A multivitamin tablet that contains that amount should be given if the formula intake is less than 500 ml per day or if the child does not get regular sunlight exposure (30 to 60 minutes each week). In nutritional rickets caused by vitamin D deficiency, calcium supplementation is essential. Daily oral administration of 2,000 to 5,000 IU vitamin D for 3 to 6 months or 300,000 to 600,000 IU intramuscularly every 3 to 6 months is the standard of care. It takes about 3 to 6 months for the physical changes to resolve, and some deformities may still require orthopedic correction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree