1–4 cups
Red and orange vegetables: All fresh, frozen, and canned red and orange vegetables, cooked or raw (e.g., tomatoes, red peppers, carrots, sweet potatoes, winter squash, and pumpkin).
Beans and peas: All cooked and canned beans and peas (e.g., kidney beans, lentils, chickpeas, and pinto beans). Does not include green beans or green peas.
Starchy vegetables: All fresh, frozen, and canned starchy vegetables (e.g. white potatoes, corn, and green peas).
Other vegetables: All fresh, frozen, and canned other vegetables, cooked or raw (e.g., iceberg lettuce, green beans, and onions).
1–2.5 cups
3–10 ounce-equivalents
At least half of all grains eaten should be whole grains
Processed/packaged baked goods and snack foods.
2–3 cups
2–7 ounce-equivalents
Use sparingly
*The number of daily servings in a food group varies depending on caloric needs. Maximum sodium limit is 2,300 mg/day.
Table 2.2 General Diet
Suggested Menu Pattern for General Diet
| Breakfast |
| ½ c. fruit 1 oz-equivalent protein 2 oz-equivalent grains 1 c. dairy products 1 tsp. oil |
| Lunch |
| 2 oz-equivalent protein 1 c. vegetables 1 oz-equivalent grains 1 c. dairy products 1 tsp. oil |
| Supper |
| 2 oz-equivalent protein 1 c. vegetables 2 oz-equivalent grains ½ c. fruit 1 c. dairy products 3 tsp. oil |
| Snack Ideas |
| ½ c. fruit ½ cup vegetable 1 oz-equivalent grain |
*Based on 1,800 calorie diet, includes up to 160 calories from solid fats and added sugars
Table 2.3 Suggested Menu Plan for General Diet
| Breakfast |
| ½ c. orange juice 1 egg ½ c. oatmeal 1 slice whole wheat toast 1 tsp. soft margarine 1 tsp. jelly 1 c. fat-free milk Hot beverage Sugar, pepper (optional) |
| Lunch |
| 2 oz. roasted chicken breast ½ c. mashed potatoes with fat-free gravy ½ c. mixed vegetables 1 oz. wheat roll 1 tsp. soft margarine 1 c. fat-free milk Water |
| Supper |
| 2 oz. tuna on 2 slices whole wheat bread, 2 tsp mayonnaise 2 tomato slices 1 c. leafy greens salad 1 Tbsp. sunflower oil and vinegar dressing ½ c. fruit cocktail 1 c. fat-free milk Water |
| Snack Ideas |
| ½ c. cantaloupe ½ c. carrot sticks 3 c. popcorn, lower fat, trans-fat free, no added salt |
NUTRITION GUIDELINES FOR PREGNANCY AND LACTATION
These nutrition recommendations are based on the Dietary Guidelines for Americans, but they provide increased amounts of protein, vitamins, and minerals needed by the pregnant or lactating woman. The suggested food plan includes foods in amounts that will provide the DRIs recommended by the National Academy of Sciences for the pregnant or lactating woman, depending on food choices. Special attention should be given to intakes of iron, folate, zinc, protein, calcium, vitamin D, and fiber to ensure adequacy. Most doctors recommend pregnant women take a daily prenatal vitamin and mineral supplement in addition to eating a healthy diet. According to the Dietary Guidelines for Americans 2010, pregnant women should consume 600 mg/day of synthetic folic acid (from fortified foods or supplements) in addition to food forms of folate from a varied diet. It is not known whether the same level of protection could be achieved by using food that is naturally rich in folate. Pregnant women should also limit white (albacore) tuna to 6 ounces per week and avoid tilefish, shark, swordfish, and king mackerel because of their high mercury content.
Diet Principles
1. Weight gain during pregnancy should be individualized according to a woman’s prepregnancy body mass index (BMI). The recommended weight gain during pregnancy for normal-weight women is 25–35 pounds. Underweight women are advised to gain 28–40 pounds; and overweight women 15–25 pounds. If excessive weight gain is a problem, the client’s portion sizes and intake of “extra” foods will need to be evaluated.
2. High caffeine consumption is associated with delayed conception, spontaneous miscarriage, and low birth weight. Pregnant and lactating women are advised to limit caffeine consumption to less than 300 mg per day. This would translate into less than 16 ounces of coffee per day.
3. Because of possible harmful effects on the developing fetus, it is advisable to avoid alcohol during pregnancy. It is also suggested to limit alcohol while breastfeeding.
4. Pregnant women should be advised to limit herbal supplements until they are proven safe during pregnancy.
5. For management of gestational diabetes, refer to the Gestational Diabetes Meal Plan in Chapter 6.
6. With rare exceptions, breastfeeding is the optimal feeding method for infants. It has been proven to improve the health of both the mother and her infant. Exclusive breastfeeding is encouraged for the first 6 months of an infant’s life and breastfeeding with complementary foods from 6 months until at least 12 months of age is ideal.
Table 2.4 Pregnancy/Lactation
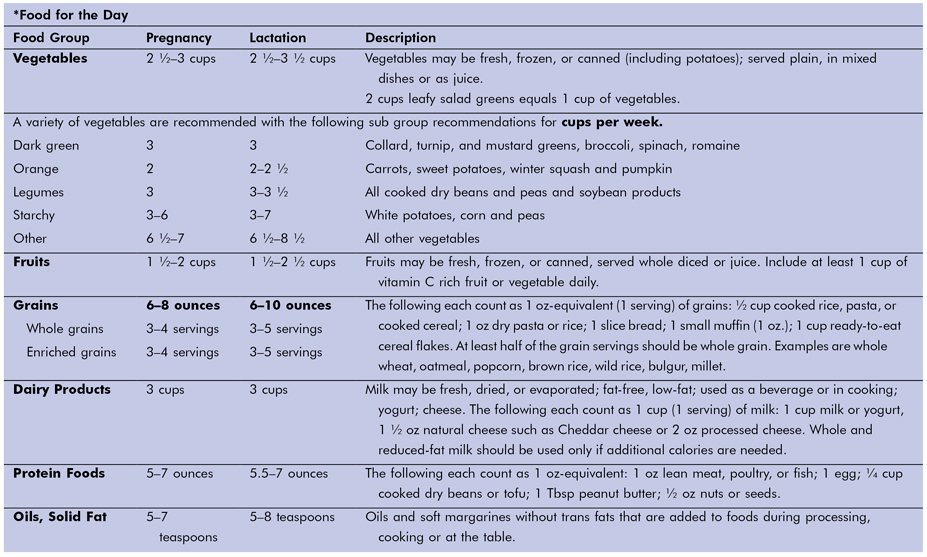
*For help in determining individual needs, go to www.ChooseMyPlate.gov for Daily Food Plans for Pregnancy and Breastfeeding.
RECOMMENDATIONS FOR FEEDING NORMAL INFANTS
At no other time in the lifecycle is nutrition delivery more important for health, growth, and development than during the first year of a child’s life. (1) These recommendations will provide the quantities of nutrients recommended by the American Academy of Pediatrics (AAP) for infants.
Diet Principles
The AAP and American Dietetic Association (ADA) strongly recommend breastfeeding as the preferred feeding for all infants over formula feeding. (2) As recommended by the AAP, exclusive breastfeeding for a minimum of 4 months and preferably 6 months is best. Breastfeeding should be continued the first 12 months of age and longer if it is desired by both the mother and infant. If families decide not to breastfeed their infant, iron-fortified formula is recommended.
Breast-Fed Infant: Birth to 12 Months
1. During the first 24 hours after birth, the newborn infant should breastfeed 8 to 12 times or more every 24 hours and usually for 10 to 15 minutes per breast. To assure the establishment of a good milk supply, frequent breastfeeding in the first few days is essential. Breastfeeding minimizes weight loss after birth and decreases bilirubin concentrations in infants. Health professionals need to be knowledgeable about both the science and art of breastfeeding and fully understand their patients to ensure breastfeeding success. Following the ten steps to successful breastfeeding provides a structure to support mothers choosing to breastfeed.
2. Breastmilk empties from the stomach faster than infant formula. Mothers many times compare their infants to bottle-fed infants. They believe that because their child eats very frequently, that they do not have a sufficient milk supply. As the infant becomes older, he or she breastfeeds more efficiently; the frequency and duration of feedings decreases.
3. The composition of human milk varies among individuals depending on the time of day, the stage of lactation, the time into feeding, and the diet of the mother. Foremilk is different than hindmilk. The first measure of colostrum is not only nourishing but also protects the infant by providing immunity and protection from infection; and it differs from transitional and mature milks. Milk and its changing concentrations of protein, fat, carbohydrates, minerals, and other properties continue to change over time. (4)
4. The recommendation for feeding infants with human milk is made because human milk has been studied and proven to be beneficial to infant nutrition, gastrointestinal function, the immune system, and has the potential beneficial influence on the development of the brain and spinal cord and also the prevention of the chronic diseases of childhood such as rotavirus.
5. If families decide not to breastfeed their infant, iron-fortified formula is recommended. However, because of the beneficial properties of human milk, the introduction of formula should be considered if: (a) it is used as a substitute or supplement for human milk in infants whose mothers choose not to breastfeed; (b) it is a substitute for human milk for infants that breastfeeding is medically contraindicated such as those with inborn errors of metabolism; and (c) it is a supplement for breastfed infants when the intake of human milk is not great enough to support adequate weight gain.
Table 2.5 Ten Steps to Successful Breastfeeding
Adapted from American Academy of Pediatrics and American College of Obstetricians and Gynecologists. Peripartum care: the transition to lactation. In: Breastfeeding Handbook for Physicians. Elk Grove Village, IL: American Academy of Pediatrics; 2006: 67–80.(4)
| Step 1 | Have a written breastfeeding policy that is routinely communicated to all healthcare staff. |
| Step 2 | Train all healthcare professionals in skills necessary to implement this policy. |
| Step 3 | Inform all pregnant women about the benefits and management of breastfeeding. |
| Step 4 | Help mothers initiate breastfeeding within 1 hour of birth. |
| Step 5 | Show mothers how to breastfeed and how to maintain lactation even if they should be separated from their infants. |
| Step 6 | Give newborn infants no food or drink other than human milk, unless medically indicated. |
| Step 7 | Practice rooming-in—allow mothers and infants to remain together 24 hours a day. |
| Step 8 | Encourage breastfeeding on demand. |
| Step 9 | Give no artificial treats or pacifiers to breastfeeding infants. |
| Step 10 | Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from the hospital or clinic, and give each mother a phone number to call for breastfeeding assistance. |
Bottle-Fed Infant: Birth to 12 Months
1. The most common human milk substitute is standard cow’s milk formula. These formulas are made from cow’s milk that is altered by removing the butterfat, adding vegetable oils and carbohydrate, and decreasing the protein. Standard formulas vary in their ratio of caseine to whey. The current requirements for protein in infant formulas range from 1.7 to 3.4 grams per 100 calories. Taurine, a free amino acid present in human milk, is often added to standard formulas. Iron-fortified formula is recommended and requires minimal vitamin or mineral supplementation if prepared with adequately fluoridated water.
2. Infant formulas are available in three forms. The three forms are: concentrated liquid, ready-to-feed, and powder. Ready-to-feed formulas provide 20 kcal/fluid ounce. When reconstituted as directed, both concentrate and powder also provide 20 kcal/fluid ounce. Each manufacturer must ensure by analysis that all 29 essential nutrients are present in each batch of formula as referenced in the Infant Formula Act and make a quantitative declaration for each nutrient on the label. In the United States, this “label claim” must be accurate until the end of the shelf life of the formula. Some vitamins degrade very little over the shelf life such as vitamin K, but others such as riboflavin, vitamin B12, and vitamin C experience considerable loss. (3)
3. Soy formulas also provide 20 kcal/ounce and are available in the same forms as milk based formulas. Because it is low in soy formulas, carnitine that plays a role in lipid metabolism is added. (3)
4. Heating formula in the bottle in a microwave oven is not recommended because this process can cause mouth burns. The formula heats unevenly, causing the outside of the bottle to feel cool even though the contents are very hot.
5. As the infant grows, the recommended number of feedings and volume change.
Table 2.6 Suggested Number and Volume of Bottle Feedings for a Normal Infant
Kelts: Manual of Pediatric Nutrition (p. 38) by DG Kelts and EG Jones. Little, Brown, and Company, 1994. Used with permission.
| Age | Number of Feedings | Volume in ml |
| Birth–1 week | 6–10 | 30–90 |
| 1 week–1 month | 7–8 | 60–120 |
| 1 month–3 months | 5–7 | 120–180 |
| 3 months–6 months | 4–5 | 180–210 |
| 6 months–9 months | 3–4 | 210–240 |
| 10 months–12 months | 3 | 210–240 |
*Note: 120 ml = 4 fluid ounces.
Supplements for All Infants
Some supplements are suggested for both breastfed and formula fed infants.
Table 2.7 Suggested Vitamin and Mineral Supplementation for Full-Term Infants (0–12 Months)
Modified from King and Samour, Handbook of Pediatric Nutrition, 3rd Edition, Jones and Bartlett Publishers, 2005, p. 91, Table 2.
| Supplement | Infants fed Human Milk | Infants Fed Commercial Formula |
| Vitamin K | A single dose is given at birth. Intestinal flora of breastfed infants produces less vitamin K so additional doses may be needed. | A single dose is given at birth. |
| Vitamin D | The content of Vitamin D is low in human milk; 200 IU/day is recommended when there is minimal exposure to sunlight. | Iron-fortified formulas are supplemented with Vitamin D. |
| Iron | The content of iron in human milk may not meet the child’s need after 6 months of age. An iron supplement is recommended by most authorities. | Iron-fortified formula is an excellent source. |
| Fluoride | 0.25 mg/day after 6 months if local water supply has <0.3 parts per million fluoride. | 0.25 mg/day after 6 months if local water supply has <0.3 parts per million fluoride or ready-to-use formula is used. |
All Infants
1. Feed infants when they give hunger cues rather than on a specific schedule. These cues include rooting, mouth opening, lip licking, placing hands to mouth, and motor activity.
2. Introduce solid foods when infants are developmentally ready using a spoon. This is usually between 4 and 6 months of age or when birth weight has doubled. Signs of developmental readiness include moving food from the front to the back of the mouth and swallowing it, sitting alone or with minimal support, reaching to grasp the spoon, and turning the head away to refuse food.
After Age 4 to 6 Months
1. Breast milk or iron-fortified formula is recommended for infants to age 1 year. Cow’s milk in any form (whole, reduced-fat [2%], low-fat [1%], or fat-free [skim]) and goat’s milk should not be given to infants during their first 12 months.
2. Developmental skills such as raising the head and swallowing are usually not present in the infant for solid foods until 4 to 6 months of age.
3. A commercially prepared, single-grain infant cereal (usually rice) fortified with iron should be the first solid food introduced. The order of introduction of other solid foods is not important.
4. Introduce no more than one single-ingredient food at a time. Offer new foods at weekly intervals to identify food intolerances. The new food can be offered several days in a row.
5. Begin teaching infants to drink from a cup at about 6 months.
6. Small, frequent feedings are preferable for infants. Let infants decide when they have had enough. “Full” cues include refusing to open mouth, turning head away, and spitting food out.
7. When infant foods are prepared at home, no salt or sugar should be added. Start with fresh or frozen foods as much as possible. Fruits canned in fruit juice and vegetables canned without salt can be used. The sugar and salt contents of many canned fruits and vegetables make them unsuitable for infants.
8. In the last several months of their first year, infants can progress from smooth foods to foods with more texture. Provide mashed foods first, followed by “chunky” foods. Offer cut-up soft table foods after infants have mastered eating chunky textures.
9. After the age of 12 months, foods should be the primary source of nourishment, even if a child continues to be breast- or bottle-fed.
10. By age 12 months, children make the transition from demand feeding to the family schedule of meals and snacks. By this time weaning from the bottle often occurs automatically as children become interested in eating table foods. Nursing from bottle or breast, if continued, should be in place of a scheduled snack and no longer given on demand.
11. To protect children’s teeth, frequent nursing from breast or bottle should not be permitted, and bottles should not be allowed in bed. (8)



