Figure 22-1 United States Department of Agriculture MyPlate. (From http://www.choosemyplate.gov [last accessed 1/5/15])
Calculating Energy Requirements
- Total energy expenditure = basal metabolic rate (BMR) + the energy expenditure of activity + the thermic effect of food.
- The thermic effect of food is a small percentage of total energy expenditure and is largely ignored when energy requirements are estimated.
- Harris-Benedict equations estimate BMR on the basis of gender, height, age, and weight:
- Male: BMR (kcal) = 66.5 + (13.8 × weight in kg) + (5 × height in cm) – (6.8 × age in years).
- Female: BMR (kcal) = 655 + (9.6 × weight in kg) + (1.9 × height in cm) – (4.7 × age in years).
- Male: BMR (kcal) = 66.5 + (13.8 × weight in kg) + (5 × height in cm) – (6.8 × age in years).
- Energy needs are then calculated by multiplying BMR by an activity factor between 0.8 and 1.8 that adjusts for the stress of various medical conditions and for the level of activity.
- Table 22-1 can be used for an easy reference to determine energy requirements.
TABLE 22-1 Energy Requirements Based on BMI
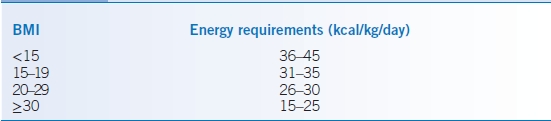
BMI, body mass index.
Macronutrients
Protein
- Components of protein include essential and nonessential amino acids. Essential amino acids are histidine, isoleucine, leucine, lysine, methionine/cystine, phenylalanine/tyrosine, threonine, tryptophan, and valine.
- Types of protein:
- Complete proteins contain all essential amino acids and are derived from animal sources and select plant sources such as soy, quinoa, spirulina, buckwheat, hemp seed, and amaranth.
- Incomplete proteins do not contain all essential amino acids.
- Complete proteins contain all essential amino acids and are derived from animal sources and select plant sources such as soy, quinoa, spirulina, buckwheat, hemp seed, and amaranth.
- Sources of protein include meat, dairy products other than cream and butter, and plant products such as grains, legumes, and vegetables.
- Plant proteins can be ingested in combination so that their amino acid patterns become complementary. Vegans can meet requirements when grains, legumes, and leafy greens are combined.
- The RDA for protein intake in young healthy adults of both sexes is 0.8 g/kg body weight/day. The average American’s daily protein intake far exceeds the RDA.
- Protein requirements increase during growth, pregnancy, lactation, and rehabilitation.
Carbohydrates
- Carbohydrates are composed of saccharide units.
- Types of carbohydrates:
- Complex carbohydrates: polysaccharides, starch, which is digestible, and fiber, which is indigestible.
- Sugars: monosaccharides (glucose, fructose), disaccharides (sucrose, lactose, maltose), or oligosaccharides; sucrose and lactose are the primary dietary sugars.
- Complex carbohydrates: polysaccharides, starch, which is digestible, and fiber, which is indigestible.
- Carbohydrates typically comprise 45% to 65% total daily calories.
- Fiber:
- Fiber is found in all plant sources (whole grains, legumes, and prunes are very good sources) and is commercially available in sources such as psyllium (e.g., Metamucil) and methylcellulose (e.g., Citrucel).
- Fiber intake for males is 30 to 38 g/day and for females is 21 to 29 g/day.
- Most Americans do not consume the recommended amount of fiber and may benefit from supplementation.
- Soluble fiber is soluble in water and fermentable by intestinal bacteria. Pectin, gum, mucilages, and some hemicelluloses are considered soluble fibers. Benefits of soluble fiber include the following:
- Delayed gastric emptying, slowed intestinal transit, and decreased glucose absorption with benefits in obese patients
- Improvement in glycemic control in diabetic patients
- A decrease in luminal wall tension (pain and cramps) and diarrhea in irritable bowel syndrome
- Binding of fatty acids, cholesterol, and bile acids leading to lower serum lipid levels and atherosclerosis prevention
- Delayed gastric emptying, slowed intestinal transit, and decreased glucose absorption with benefits in obese patients
- Insoluble fiber is insoluble in water and not fermented by intestinal bacteria. Cellulose, lignin, and some hemicelluloses are considered insoluble fibers. Sources of insoluble fiber include certain plant sources (whole grains, flax seed, and certain vegetables such as celery, potato skin, and green beans). Benefits of insoluble fiber include the following:
- Increased intestinal transit and increased fecal bulk, resulting in a laxative effect
- May reduce the rates of diverticulosis and colonic neoplasms
- Increased intestinal transit and increased fecal bulk, resulting in a laxative effect
- Fiber is found in all plant sources (whole grains, legumes, and prunes are very good sources) and is commercially available in sources such as psyllium (e.g., Metamucil) and methylcellulose (e.g., Citrucel).
Fat
- Components of fat include glycerol backbone with three fatty acid chains. Fats are categorized by the following:
- Fatty acid chain length: short-chain, medium-chain, and long-chain fatty acids.
- Degree of hydrogen saturation of the fatty acid chains: polyunsaturated (multiple unsaturated sites), monounsaturated (a single unsaturated site), and saturated (completely saturated).
- Ability of the body to synthesize the fat: essential or nonessential. Essential fatty acids are omega-3 α-linolenic acid and omega-6 linolenic acid. All other fatty acids are nonessential.
- Fatty acid chain length: short-chain, medium-chain, and long-chain fatty acids.
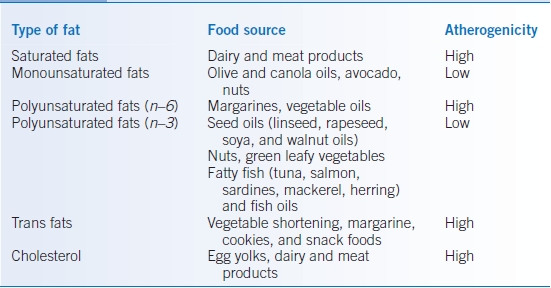
- Increasing saturation is associated with increasing risk of coronary artery disease. Unsaturated fatty acids may be hydrogenated to form trans fats.
- Polyunsaturated fats are divided into n–6 and n–3 fatty acids according to their molecular structure. A high ratio of n–6 fatty acid to n–3 fatty acid intake may be atherogenic.
- Fat should comprise no more than 35% of total daily calories, and saturated fat should comprise no more than 7% of total daily calories.
- Trans fats are made by hydrogenating vegetable oils, which solidifies the oils and increases the shelf life and flavor of the foods that contain them. They contribute to increased blood low-density lipoprotein (LDL) cholesterol, decreased blood high-density lipoprotein (HDL) cholesterol, and coronary artery disease. Trans fat should comprise no more than 1% of total daily calories.
- Monounsaturated fats (when substituted for saturated fat) have beneficial effects on the cholesterol profile decreasing LDL and triglyceride levels while increasing HDL.
Cholesterol
- Dietary fats and cholesterol are packaged into lipoproteins for delivery to the tissues.
- The classification of lipoproteins can be found in Chapter 11.
- LDL, very–low-density lipoprotein (VLDL), intermediate-density lipoprotein (IDL), and chylomicrons carry cholesterol to the tissues with LDL carrying 70% of serum cholesterol.
- HDL returns cholesterol from the tissues to the liver and carries 20% to 30% of serum cholesterol. HDL levels are inversely correlated with the risk of heart disease.
- Reduced saturated fat, trans fat, and cholesterol intake; weight loss; and dietary adjuncts such as soluble fiber, plant sterols and stanols, and soy protein may decrease LDL cholesterol levels.
- Aerobic exercise, weight loss through decreasing caloric intake, smoking cessation, omega-3 fatty acid intake, increased soluble fiber intake, and drinking one to two servings of alcohol daily have been associated with increased HDL levels.3
- Cholesterol intake should be <300 mg/day (Table 22-2).
TABLE 22-2 Dietary Sources of Fats
Alcohol
- Alcohol is structurally similar to carbohydrates.
- Each gram of ethanol yields 7 kcal and can be a significant source of empty calories.
- The alcohol contents in one 1.5-oz shot of hard liquor, one 12-oz beer, and one 5-oz glass of wine are roughly equivalent. One serving of an alcoholic beverage provides 14 to 20 g ethanol (100 to 140 calories) plus additional calories found in additives such as cream, sodas, or fruit juices.
- Ethanol is known to increase HDL in serum; thus, moderate ethanol use may convey a cardioprotective effect.
- Alcohol interferes with thiamine absorption and formation of its active metabolite.
Macronutrient Substitutes
- Artificial sweeteners and sugar substitutes provide sweetness with a reduction in calories. Five artificial sweeteners have been approved by the U.S. Food and Drug Administration (FDA): saccharin, aspartame, acesulfame, sucralose, and neotame (Table 22-3).
- The fat replacement olestra is a mixture of hexa-, hepta-, and octaesters of sucrose with long-chain fatty acids.
- Olestra imparts taste indistinguishable from fat yet is too large to be absorbed.
- It is currently found primarily in snack foods such as chips.
- Side effects include cramping, flatulence, and diarrhea from fat malabsorption. Poor absorption of fat-soluble vitamins may occur because they are excreted with olestra.
- Olestra imparts taste indistinguishable from fat yet is too large to be absorbed.
TABLE 22-3 Current Artificial Sweeteners
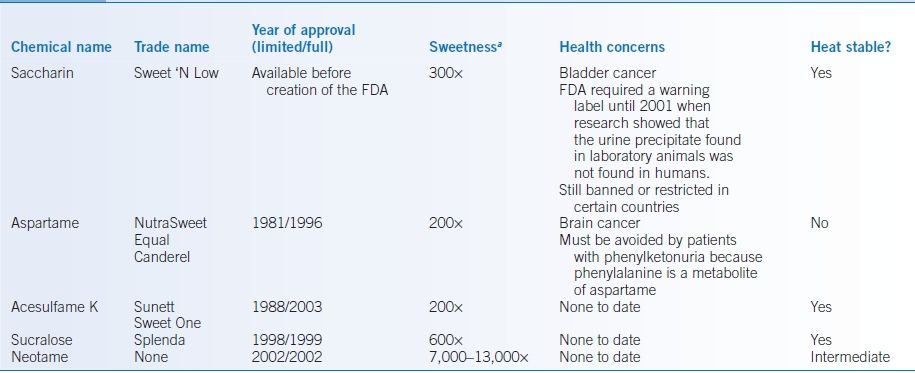
aAs compared to sucrose.FDA, Food and Drug Administration.
Micronutrients
- Vitamins are essential organic compounds that are required to maintain growth, metabolism, and overall health. Vitamins are either fat soluble (vitamins A, D, E, and K) or water soluble (all other vitamins) (Table 22-4).
- Dietary minerals are inorganic compounds that do not supply energy (Table 22-5). They are important in regulating metabolism, tissue catabolism, and anabolism, including
- Cellular regulation and fluid balance
- Coenzymes and cofactors
- Bone and tooth formation
- Cellular regulation and fluid balance
TABLE 22-4 Water- and Fat-Soluble Vitamins
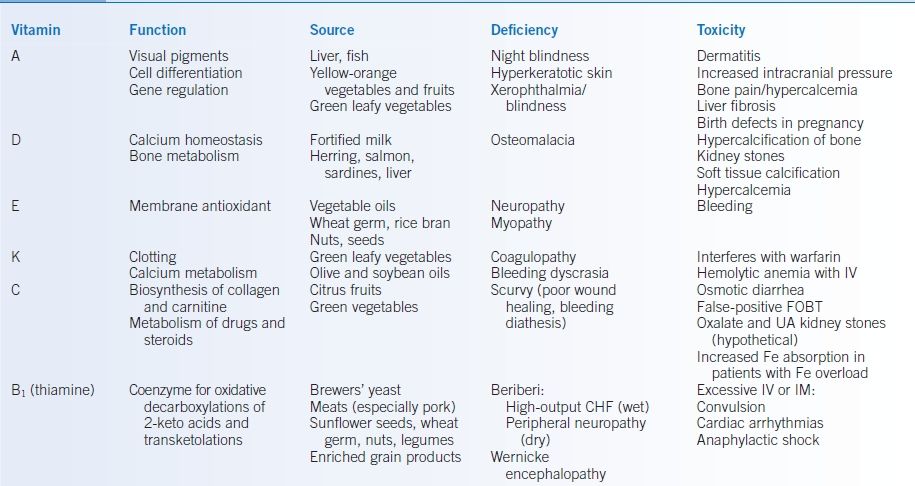
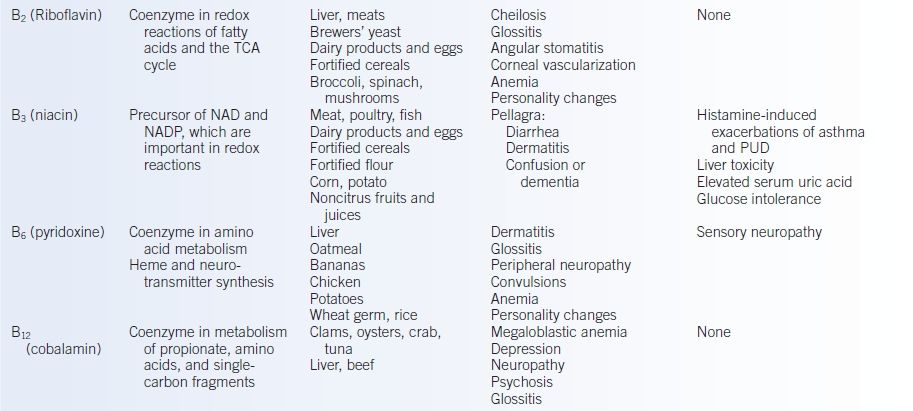
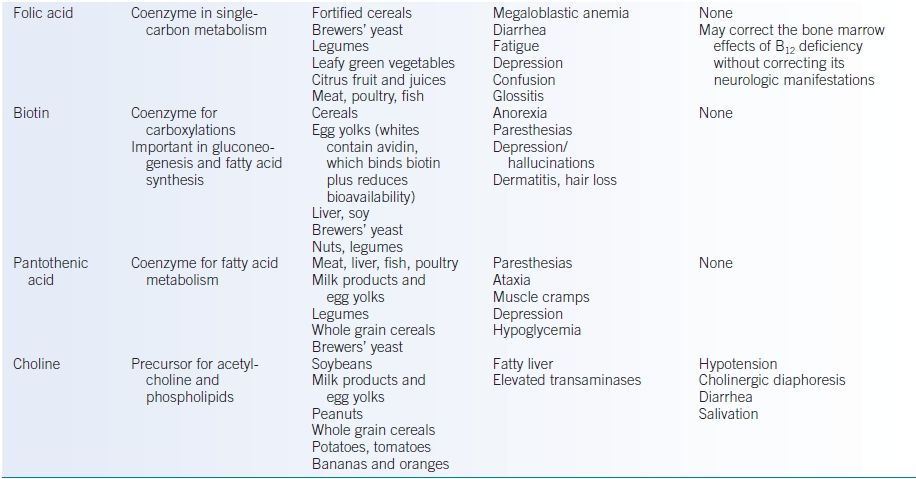
CHF, congestive heart failure; FOBT, fecal occult blood testing; NAD, nicotinamide adenine dinucleotide; NADP, nicotinamide adenine dinucleotide phosphate; PUD, peptic ulcer disease; TCA, tricarboxylic acid; UA, uric acid.
TABLE 22-5 Minerals
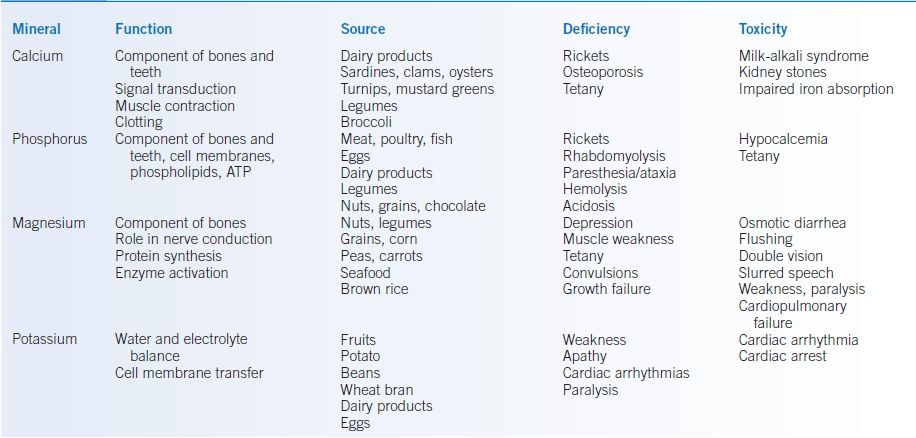

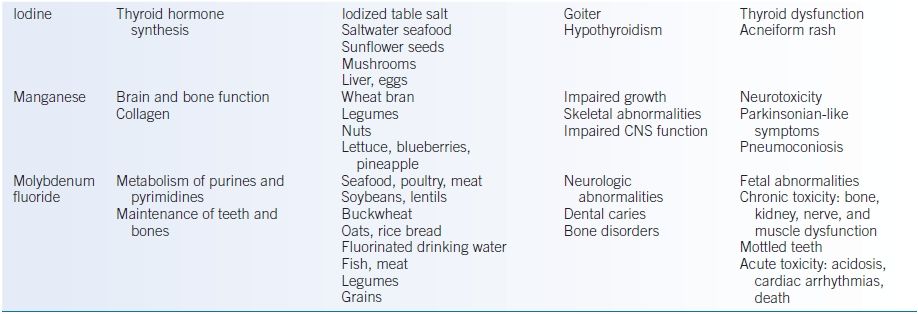
ATP, adenosine triphosphate; CNS, central nervous system; GI, gastrointestinal.
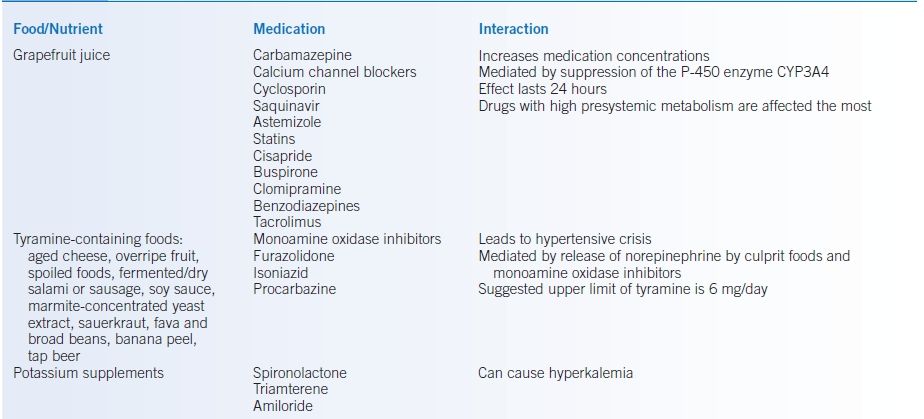
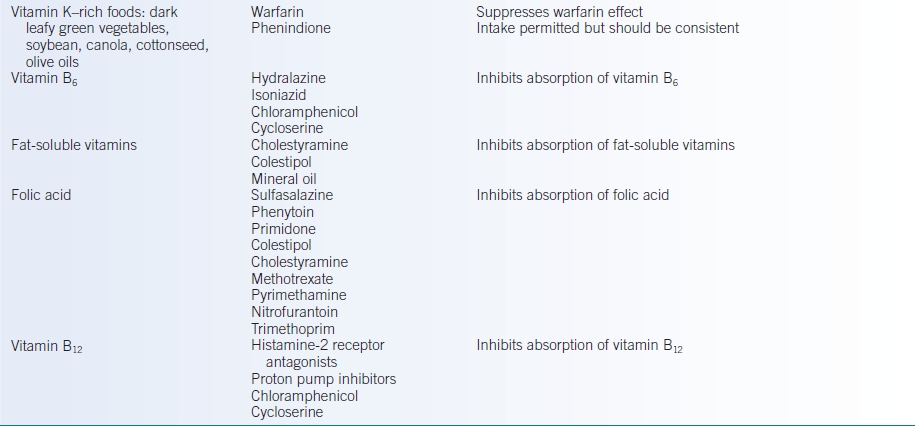
DRUG-NUTRIENT INTERACTIONS
- Food can enhance or impede medication effects.
- Medication can influence food and nutrient intake, absorption, metabolism, and excretion.
- It is beyond the scope of this chapter to list all possible interactions; however, some common interactions may be found in Table 22-6.
TABLE 22-6 Important Food/Nutrient and Medication Interactions
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


