Chapter 4 Nutrition
I. Key Dietary Terminology
A. Overview
1. The dietary reference intake (DRI) is a set of several reference values, including the recommended dietary allowance related to adequate intakes and upper levels of intakes.
2. The recommended dietary allowance (RDA) refers to intakes needed for optimal health; it is not a minimum daily requirement.
3. Daily energy expenditure depends most importantly on the basal metabolic rate (BMR) and on postprandial thermogenesis and the degree of physical activity.
4. The respiratory exchange rate (RER), also called the respiratory quotient, is the rate of oxygen consumption for different carbon sources.
5. The body mass index (BMI) is used to determine obesity, defined as a BMI greater than 30 (normal, 20 to 25).
B. DRI
C. RDA
1. RDA represents an optimal dietary intake of nutrients that under ordinary conditions can maintain a healthy general population.
D. Basal metabolic rate (BMR)
1. BMR accounts for about 60% of daily energy expenditure and refers to the energy consumption of an individual at rest.
3. Physical activity is variable and is expressed as an activity factor, which when multiplied by the BMR equals the daily energy expenditure.
E. Respiratory exchange rate (RER)
1. The respiratory exchange rate (RER), also called the respiratory quotient, is the rate of oxygen consumption for different carbon sources.
F. BMI
4. Sample calculations using two patients, A and B:
a. Patient A consumes 3600 kcal/day consisting of 168 g of fat, 108 g of protein, and 414 g of carbohydrates. Calculate the percentage of each of the nutrients. Is the patient gaining, maintaining, or losing weight?
b. Patient B consumes 2000 kcal/day consisting of 67 g of fat, 60 g of protein, and 290 g of carbohydrates. Calculate the percentage of each of the nutrients. Is the patient gaining, maintaining, or losing weight?
II. Dietary Fuels
A. Overview
1. Dietary carbohydrates with α-1,4 glycosidic linkages are digested to monosaccharides and transported directly to the liver through the hepatic portal vein.
2. Dietary carbohydrates with β-1,4 glycosidic linkages are not digested but serve other functions in the gut such as reducing cholesterol absorption and softening the stool.
3. Triacylglycerols are the major dietary lipids, although phospholipids and cholesterol are also consumed in the diet.
4. Long-chain triacylglycerols and cholesterol are packaged in chylomicrons and bypass the liver by transport through the lymphatics to the subclavian vein.
5. Dietary proteins are digested to free amino acids for the synthesis of proteins and to supply carbon skeletons for the synthesis of glucose for energy.
B. Dietary carbohydrates (see Chapter 1)
2. α-Amylase, which is found in saliva in the mouth and in pancreatic secretions in the small intestine, cleaves the α-1,4 linkages in starch, producing smaller molecules (e.g., oligosaccharides and disaccharides).
3. Intestinal brush border enzymes (e.g., lactase, sucrase, maltase) hydrolyze dietary disaccharides into the monosaccharides glucose, galactose, and fructose, which are reabsorbed into the portal circulation by carrier proteins in intestinal epithelial cells (see Chapter 3).
4. Insoluble and soluble dietary fiber has β-1,4 glycosidic linkages which cannot be hydrolyzed by amylase and supply no energy, but they serve several important functions in the body.
a. Fiber increases intestinal motility, which results in less contact of bowel mucosa with potential carcinogens (e.g., lithocholic acid).
c. Fiber softens the stool, which alleviates constipation and reduces the incidence of diverticulosis of the sigmoid colon.
d. Fiber reduces absorption of cholesterol (decreasing blood cholesterol), fat-soluble vitamins, and some minerals (e.g., zinc).
e. Soluble fiber (e.g., oat bran, psyllium seeds) has a greater cholesterol-lowering effect than insoluble fiber (e.g., wheat bran).
C. Dietary lipids
1. Long-chain free fatty acids from triacylglycerols provide the major source of energy to cells, with the exception of RBCs and the brain.
2. Dietary fats also contain essential fatty acids and are required for the absorption of fat-soluble vitamins.
3. The composition of dietary triacylglycerols varies in plants and animals.
a. Plants primarily contain unsaturated and saturated fats.
b. Animals also contain unsaturated and saturated fats.
4. Essential fatty acids are required in the diet and include the polyunsaturated fatty acids linoleic (n-6) and linolenic (n-3) acids.
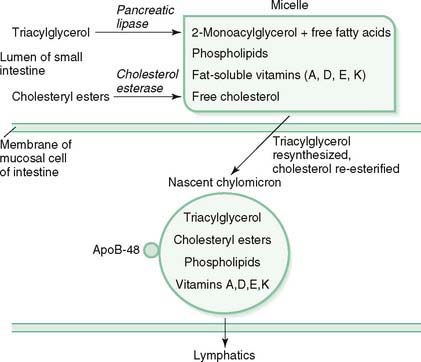
5. Dietary triacylglycerols are digested primarily in the small intestine (Fig. 4-1).
a. Pancreatic lipase (aided by colipase) degrades triacylglycerol into 2-monoacylglycerol and free fatty acids.
c. 2-Monoacylglycerol, free fatty acids, and cholesterol, along with fat-soluble vitamins and phospholipids, are emulsified by bile salts to form micelles that are absorbed into intestinal mucosal cells by passive diffusion.
d. Nascent chylomicrons are assembled in mucosal cells and contain triacylglycerols (≈85%), cholesteryl esters (≈3%), phospholipids, the fat-soluble vitamins (i.e., A, D, E, and K), and apolipoprotein B-48, which is necessary for secretion of chylomicrons into the lymphatics.
e. When discharged into the lymphatic vessels, lipoproteins rich in triacylglycerols ultimately enter the bloodstream and circulate to deliver fatty acids to tissues (see Chapter 7).
D. Dietary proteins
1. The biologic value of a dietary protein is determined by its content of essential amino acids (see Chapter 1).
a. Plant proteins (e.g., rice, wheat, corn, beans) are of low biologic value unless they are combined to provide all of the essential amino acids.
b. Animal proteins (e.g., eggs, meat, poultry, fish, and dairy products) are of high biologic value because they contain all of the essential amino acids.
2. Digestion of dietary proteins begins in the stomach, where the low pH denatures proteins, making them more susceptible to enzymatic hydrolysis.
b. Pancreatic proteases (e.g., trypsin) and peptidases secreted by intestinal epithelial cells digest the polypeptides from the stomach to free amino acids.
c. Uptake of amino acids from the intestinal lumen and their release into the portal circulation by carrier proteins in the intestinal epithelial cells are driven by the hydrolysis of ATP.
3. Proteins are in a constant state of degradation and resynthesis.
a. When amino acids are oxidized, their nitrogen atoms are fed into the urea cycle in the liver and excreted as urea in the urine (primary route), feces, and sweat (see Chapter 8).
b. Nitrogen balance is the difference in the amount of nitrogen (protein) consumed and the amount of nitrogen excreted in the urine, sweat, and feces.
(1) Healthy adults are normally in zero nitrogen balance (i.e., nitrogen intake equals nitrogen loss).
(2) A positive nitrogen balance (i.e., nitrogen intake is greater than nitrogen loss) indicates active synthesis of new protein. Examples include pregnancy and lactation, growth in children, and recovery from surgery, trauma, or extreme starvation.
5. Protein-energy malnutrition results from inadequate intake of protein or calories.
a. Marasmus is caused by a diet deficient in protein and calories (e.g., total calorie deprivation).
b. Kwashiorkor is caused by a diet inadequate in protein in the presence of an adequate carbohydrate intake.
III. Water-Soluble Vitamins

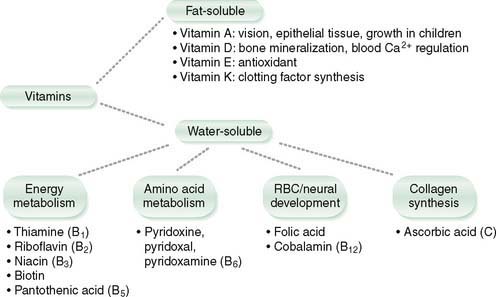
A. Overview (Fig. 4-2 and Table 4-1)
1. Thiamine functions in oxidative decarboxylation and pentose phosphate pathway; deficiency produces beriberi.
3. Niacin functions in NAD+ and NADP+ as cofactors for redox reactions; deficiency produces pellagra.
4. Pantothenic acid functions in fat and carbohydrate metabolism as a component of acetyl CoA and fatty acid synthase; deficiency symptoms are unknown.
5. Pyridoxine functions in transamination reactions, heme synthesis, glycogenolysis, and various other amino acid conversions; deficiency produces sideroblastic anemia and peripheral neuropathy.
6. Cobalamin functions in single carbon metabolism; deficiency produces macrocytic anemia and pernicious anemia.
9. Ascorbic acid (vitamin C) functions in hydroxylation reactions; deficiency produces scurvy.
TABLE 4-1 Water-Soluble Vitamins: Signs and Symptoms of Deficiency
| Vitamin | Signs and Symptoms of Deficiency |
|---|---|
| Thiamine (vitamin B1) | Wernicke-Korsakoff syndrome (confusion, ataxia, nystagmus, ophthalmoplegia, antegrade and retrograde amnesia, precipitated by giving thiamine with glucose in intravenous solution); peripheral neuropathy (dry beriberi); dilated cardiomyopathy (wet beriberi) |
| Riboflavin (vitamin B2) | Corneal neovascularization; glossitis; cheilosis; angular stomatitis |
| Niacin (vitamin B3) | Pellagra, with diarrhea, dermatitis, dementia |
| Pantothenic acid (vitamin B5) | None identified |
| Pyridoxine (vitamin B6) | Sideroblastic anemia; peripheral neuropathy; convulsions |
| Cobalamin (vitamin B12) | Macrocytic (megaloblastic) anemia; neutropenia and thrombocytopenia; hypersegmented neutrophils; glossitis; subacute combined degeneration (posterior column and lateral corticospinal tract demyelination); dementia; achlorhydria, atrophic gastritis body and fundus, increased serum gastrin (only in pernicious anemia); increased plasma homocysteine; increased urine methylmalonic acid |
| Folic acid | Same as vitamin B12 deficiency with the following exceptions: no neurologic dysfunction and normal urine methylmalonic acid level |
| Biotin | Dermatitis, alopecia, glossitis, lactic acidosis |
| Ascorbic acid (vitamin C) | Bleeding diathesis (ecchymoses, hemarthroses, bleeding gums, perifollicular hemorrhages, corkscrew hairs); loosened teeth; poor wound healing; glossitis |
B. Thiamine (vitamin B1)
1. Sources of thiamine include enriched and whole-grain cereals, brewer’s yeast, meats, legumes, and nuts.
2. Thiamine pyrophosphate is the active form of the vitamin.
3. Thiamine deficiency most commonly occurs in alcoholics or malnourished individuals.
a. Most clinical findings in thiamine deficiency reflect the loss of ATP from dysfunction of the pyruvate and α-ketoglutarate dehydrogenase reactions, which normally gain 2 NADH (6 ATP).
b. Intravenous infusion of a glucose-containing fluid may precipitate acute thiamine deficiency in alcoholics (depleted by the pyruvate dehydrogenase reaction); deficiency is manifested by Wernicke-Korsakoff syndrome (WKS).
c. WKS includes confusion, ataxia, nystagmus, eye muscle weakness, and retrograde and antegrade memory deficits.
C. Riboflavin (vitamin B2)
Get Clinical Tree app for offline access
2. Flavin adenine dinucleotide (FAD) and flavin mononucleotide (FMN) are the active forms of riboflavin.