Notes—Cholecystectomy
Santiago Horgan
Garth R. Jacobsen
Anatomy
This chapter will assume that the surgeon undertaking an endoscopically assisted cholecystectomy has a mastery over biliary anatomy. This is an essential prerequisite, as visualization of the critical structures in a natural orifice translumenal endoscopic surgery (NOTES) cholecystectomy may be from different angles, with lighting conditions that are different than those obtained during a standard rigid scope cholecystectomy. Visualization during a NOTES cholecystectomy is most often achieved through a flexible endoscope. Current flexible endoscopic platforms (i.e., endoscopes) do not automatically correct for horizon and mirror imaging of the target structures. Despite the above limitations, a clear critical view must always be obtained. Some of the differences in visualization with both a laparoscope and an endoscope can be seen in Figure 1. While correction of horizon in a transvaginal cholecystectomy with a standard endoscope is a relatively simple task, this is not the case with a transgastric cholecystectomy. By necessity the scope must be retroflexed, which introduces additional complexity and mental strain in correcting for horizon and mirror imaging. Practice in both inanimate and animate models as well as in routine endoscopic procedures is essential in gaining real-time proficiency in image correction and correct interpretation of the anatomy.
Transgastric cholecystectomy provides for two unique anatomical challenges to the NOTES surgeon when compared with a standard open or laparoscopic cholecystectomy, the first of which is choosing a gastric access site. Surgeons undertaking a transgastric natural orifice procedure are presumably familiar with basic endoscopic techniques such as percutaneous endoscopic gastrostomy tube placement. When choosing a gastric access site one must be able to locate the anterior gastric wall. This is done most readily by utilizing techniques of transillumination and palpation. Current limitations of endoscopic instrumentation have prohibited routine application of pure NOTES (i.e., not hybrid) cholecystectomy. The vast majority of natural orifice cases performed within the United States and internationally to date have been of a hybrid technique, defined as utilizing one or more transabdominal ports. This allows for visualization of the gastrotomy site not only from the intralumenal endoscopic view, but also from within the abdominal cavity with a standard laparoscope. The practicing NOTES surgeon should not disregard the tremendous value of having a standard laparoscopic view and utilize this to their advantage.
The ideal gastric access site is on the anterior wall of the stomach in a position that allows for as in-line as possible passage of the gastroscope or operating platform from the esophagogastric junction to be lower third of the stomach in a prepyloric position (Fig. 2). In addition, care must be taken to avoid the gastroepiploic vessels. Consideration of this anatomical access site will make subsequent retroflexion and manipulation of the operative platform or endoscope easier. In addition in-line access will augment the surgeon’s ability to close the gastric defect with currently available endoscopic suturing techniques. This will eliminate the need to severely flex the scope or suturing device, which in turn limits the fidelity of all currently available instrumentation.
A second critical anatomic consideration during transgastric cholecystectomy is that of esophageal diameter. A review of the gastrointestinal literature as well as experience within our own lab have demonstrated the maximal diameter of a specimen that may be safely extracted from the esophagus to be approximately 2 to 3 cm. Preoperative ultrasonography can easily demonstrate stones that may be larger than this size limitation. It can be extremely difficult, if not impossible, to crush, or pulverize large stones prior to extraction. In this situation a transgastric approach may not be ideal, and could at worst result in esophageal perforation during extraction. In addition, a densely packed gallbladder full of small stones may easily surpass this size limitation and care must be taken when extracting gallbladders of this nature. If the gallbladder is packed with smaller stones, it can be opened and the small stones either left to pass enterally or extracted within a specimen bag. The tightest points during a transgastric extraction are at the level of the gastric wall, the lower esophageal sphincter, and the cervical esophagus.
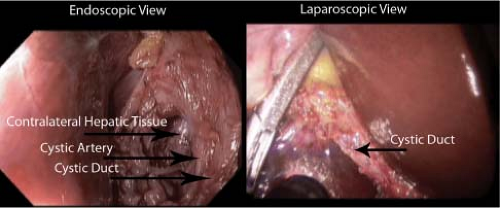 Fig. 1. Real-time synchronous images from an endoscope on the left and a laparoscope on the right. Notice the gastroscope on the bottom left hand side of the laparoscopic view. |
While gastric anatomy may be familiar to today’s general, biliary, and gastrointestinal surgeon, female pelvic anatomy may not. Safe routine access to the peritoneal cavity via transvaginal route has been practiced by gynecologists for decades. However, to obtain safe access one must be familiar with the female pelvic anatomy. The vaginal wall itself is composed of several layers consisting of an inner squamous epithelium followed by submucosa and smooth muscle. The first critical consideration that must be made is for the blood supply of the uterus and vagina. The blood supply of the vagina comes in laterally and is composed of branches from the internal iliac artery, more specifically the uterine artery, the vaginal artery, and the internal pudendal artery. Likewise, venous drainage occurs laterally via vaginal and internal pudendal veins. The somatic innervation of the vagina consists of branches from the pudendal nerve originating from sacral segments 2 to 4. There is almost no innervation to the upper two-thirds of the vagina or the posterior vaginal fornix.
Safe access is always performed through the midline posterior to the cervix transversing the posterior vaginal fornix (Fig. 3). The posterior vaginal fornix is anatomically located posterior to the cervix, and can be
readily localized by speculum examination. As with transgastric access, there have been clinical reports of blind access to the peritoneal cavity without the use of a transabdominal trocar. However, given the relative proximity of the pelvic vasculature as well as rectum and other viscera, the authors believe that blind access through this space represents a potential hazard.
readily localized by speculum examination. As with transgastric access, there have been clinical reports of blind access to the peritoneal cavity without the use of a transabdominal trocar. However, given the relative proximity of the pelvic vasculature as well as rectum and other viscera, the authors believe that blind access through this space represents a potential hazard.
Further anatomic consideration must be made for the normal anatomic depth and position of the uterus. While standing the normal uterus flexes anteriorly to a position that is approximately 90 degrees in relation to the vagina. This is not the case when in the supine position. In order to safely visualize access through the posterior vaginal fornix it is often necessary to use a uterine retractor to flex the uterus anteriorly. Commercially available uterine retractors must be sized appropriately. Most specifically, the depth of the retractor must be set. This can be done with gentle probing of the uterus through the cervical os with a uterine sound to gauge depth. However, when doing so one must be familiar with the normal anatomic depth. The normal anatomical depth is between 4 and 6 cm from the internal cervical os to the back of the uterine vault. Careful consideration of the above anatomy, and proper selection of an access site, whether transvaginal or transgastric, will aid in safe access to the peritoneal cavity.
The clinical presentation of a patient who is a candidate for a NOTES cholecystectomy is currently elementally different than that of a standard cholecystectomy patient. The introduction of natural orifice techniques has been careful and stepwise. Surgeons, for the most part, have been extremely cautious in the application of these techniques, at least within the United States. While the modern-day laparoscopic surgeon is comfortable approaching most gallbladder disease with at least an attempted laparoscopic approach, the natural orifice surgeon is more cautious. A concerted effort has been made in order to not repeat the injuries introduced with the rapid introduction of laparoscopic cholecystectomy. All natural orifice cases done within the United States to date have been done under tightly controlled situations and strict review by institutional review boards. The initial cases were undertaken in patients with symptomatic cholelithiasis. However, as the experience has progressed chronic cholecystitis has been addressed, as has acute cholecystitis. Given today’s technological limitations, natural orifice approaches, especially transgastric, should be limited to highly selected patients. The surgeon endeavoring to approach the gallbladder through these alternate access routes should begin their experience with routine symptomatic cholelithiasis cases.
 Fig. 2. Gastric entry using balloon dilation technique. On the left is seen the laparoscopic view during a hybrid cholecystectomy and on the right is the concomitant endoscopic view. |
Given the inherent difficulty of operating through an endoscopic platform, such as decreased ability to triangulate, and struggling to actively correct an image that is linked to one or more instruments, a thorough investigation of the gallbladder should be had prior to operative intervention. This consists, at minimum, of an abdominal ultrasound. If one is considering a transvaginal approach, a pelvic ultrasound may be useful to delineate uterine anatomy and identification of anomalies such as a severely retroverted uterus or large uterine fibroids. Particular care must be taken in the evaluation of patients who have had chronic pelvic pain |or an extremely retroverted uterus. In the case of the severely retroverted uterus, retraction of the organ in order to gain access to the posterior vaginal fornix may be difficult or impossible. Likewise, patients who have severe endometriosis may have pelvic adhesions that could make pelvic access impossible. With regard to transgastric cholecystectomy, prior gastric intervention, such as bariatric procedures, and/or gastric resections have not been undertaken for good reason. Alterations in gastric anatomy and blood supply may make access to the peritoneal cavity difficult and closure unreliable.
As mentioned above, there is an anatomic limitation as to the size of which specimens can be extracted through the transgastric route, particularly relating to the compliance of the gastric wall as well as the esophageal diameter. Stones larger than 2 to 3 cm may require enlarging of the gastrotomy site, which may result in a difficult and unreliable closure. Additionally, it is not possible to pass a stone
or a gallbladder full of stones that is larger than 2 to 3 cm through the gastroesophageal junction or cervical esophagus without risk of traumatic laceration or disruption.
or a gallbladder full of stones that is larger than 2 to 3 cm through the gastroesophageal junction or cervical esophagus without risk of traumatic laceration or disruption.
Certainly the treatment of biliary disease in relation to natural orifice surgery follows all current standards in place for the techniques of open or laparoscopic cholecystectomy. Currently the transvaginal access route is the most widely applied. This derives from the fact that the complexity and necessity for advanced platforms is much less. The vaginal access route offers direct access to the right upper quadrant with both flexible and rigid instrumentation. Many of these instruments are modifications of standard laparoscopic instrumentation, and are familiar to the surgeon. The closure of the vaginotomy is a simple task and can be done under direct visualization with standard open instrumentation and absorbable suture. Transgastric access involves a 60- to 90-degree retroflexion of either a dual-channel endoscope or an operative platform. This introduces additional difficulty with visualization, and, unless a hybrid technique is employed, absolutely limits the ability to use standard rigid instrumentation. The Natural Orifice Surgery Consortium for Assessment and Research (NOSCAR®) maintains a voluntary database housing clinical data on natural orifice surgery outcomes. A recent query of this database yielded 166 total cases of transvaginal cholecystectomy. However, a review of the current literature, as well as unpublished reports from national meetings, brings the total number of cases to well over 300. The estimated number of transgastric cases is dramatically lower, and is estimated to be less than 100.
Current indications for transgastric or transvaginal cholecystectomy are evolving. In the hands of a skilled surgical team, routine transvaginal cholecystectomy for biliary colic can be performed with operative times that are approaching those of their more conventional counterparts. Transgastric cholecystectomy, as mentioned above, is more difficult and should be considered highly investigational and subject to intense scrutiny by the surgeon’s own institution as well as surgical societies. The current indications for this procedure have much less to do with the disease process than to do with the experience of the surgical team, as well as that team’s access to advanced endoscopic technologies. We are not at a point that widespread application of either the transvaginal or transgastric route can be routinely recommended to the practicing general surgeon. However, as data regarding safety and efficacy accumulate, the indications will most certainly broaden.
Preoperative planning is essential in all natural orifice cases. Much that we take for granted today was painstakingly developed and refined by the pioneers of laparoscopic surgery. Technology is advancing at a rapid pace, and new instrumentation is available with each passing month. Certainly the patient’s disease state plays a role, and considerations such as the size of the gallbladder stones and information as to the level of inflammation are important. In addition, knowledge of prior gastric and vaginal intervention must be gained, and a thorough medical surgical history taken. As the operative date draws near, most of the planning revolves around the utilization and availability of endoscopic and laparoscopic instrumentation to accomplish the surgical task. We believe that a set team that is well versed and practiced in both inanimate and animate models to be essential for surgical success. Preoperative planning starts in the lab. Once sound execution of natural orifice access techniques and familiarity with instrumentation has been firmly established, the team can begin the transition to the clinical arena. The first step in accomplishing this is to set up a natural orifice operating suite.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



