Patient Story
A 2-week-old infant is brought to the office for her first well-baby check. The parents noticed a rash on the face. You diagnose the white spots on the bridge of the nose as milia and neonatal acne on the cheeks. The parents are happy to hear that the neonatal acne and milia will go away without treatment (Figures 108-1 and 108-2).
Introduction
- Rashes are common in newborns. Physicians will be consulted frequently as they are a common parental concern. Almost all newborn rashes are benign; however, a few are associated with more serious conditions. A newborn’s skin shows a variety of changes during the first 2 months of life and most are self-limited. Physicians must be prepared to identify common rashes and advise parents.1
- Milia are inclusion cysts that appear as tiny white papules in the skin (Figure 108-1) or on the roof of the mouth.
- Neonatal acne is an acneiform eruption appearing as small red papules or whiteheads with surrounding erythema on the skin of newborns (Figure 108-2).
- A mongolian spot is a hereditary, congenital macule of bluish-black or bluish-gray pigment usually in the sacral area, back, and buttocks of infants (Figures 108-3 and 108-4).
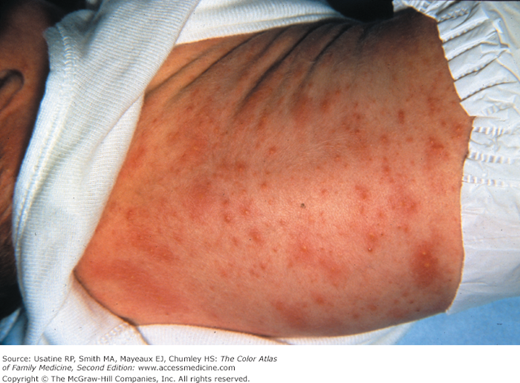
- Erythema toxicum neonatorum (ETN) is a benign, self-limited skin eruption appearing as small yellow-white papules or vesicles with surrounding skin erythema (Figures 108-5 and 108-6).
Synonyms
Epidemiology
- Approximately 40% of newborn infants in the United States develop milia.2 This condition is mainly associated with newborns carried to full term or near term.
- Neonatal acne occurs in up to 20% of the newborns. It typically consists of close comedones of the forehead, nose, and cheeks, although other locations are possible. It is most frequent in boys in the first week of life.3
- The prevalence of mongolian spots varies among different ethnic groups. They have been reported in approximately 96% of black infants, 90% of Native American infants, 81% to 90% of Asian infants, 46% to 70% of Hispanic infants, and 1% to 10% of white infants.2,4,5
- ETN occurs in 30% to 70% of full-term infants and in 5% of premature infants. The incidence rises with increasing gestational age and birth weight.6,7
Etiology and Pathophysiology
- Milia are inclusion cysts that contain trapped keratinized stratum corneum surrounded by a dense lymphocytic infiltrate. Milia are caused by retention of keratin within the dermis. They may rarely be associated with other abnormalities in syndromes such as epidermolysis bullosa and the orofacial digital syndrome (type 1).2,8
- Maternal androgenic hormones that stimulate sebaceous glands likely cause neonatal acne.9
- Hyperactivity of sebaceous glands, stimulated by neonatal androgens, has been implicated as the underlying pathogenic mechanism.
- Histologic examination shows hyperplastic sebaceous glands with keratin-plugged orifices.
- Hyperactivity of sebaceous glands, stimulated by neonatal androgens, has been implicated as the underlying pathogenic mechanism.
- The mongolian spot is a hereditary, congenital, developmental condition exclusively involving the skin. It results from entrapment of melanocytes in the dermis during their migration from the neural crest into the epidermis.
- Mongolian spots are associated with cleft lip, spinal meningeal tumor, melanoma, and phakomatosis pigmentovascularis types 2 and 5.2,10
- A few cases of extensive mongolian spots have been reported with inborn errors of metabolism, the most common being Hurler syndrome, followed by gangliosidosis type 1, Niemann-Pick disease, Hunter syndrome, and mannosidosis. In such cases, they are likely to persist rather than resolve.2,4
- Mongolian spots are associated with cleft lip, spinal meningeal tumor, melanoma, and phakomatosis pigmentovascularis types 2 and 5.2,10
- The etiology of ETN is not known. ETN is thought to be an immune system reaction; the condition is associated with increased levels of immunologic and inflammatory mediators (e.g., interleukins 1 and 8, eotaxin).11

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree