Normal Anatomy and Histology
Paul W. Biddinger
Descriptions of the thyroid and related diseases date back to antiquity. The thyroid was identified by European anatomists during the Renaissance including Vesalius who described the glandulas ad laryngis radicem adnatas in book six of his famous work De Humani Corporis Fabrica of 1543. Thomas Wharton is generally credited for first using the term thyroid gland in his 1656 treatise Adenographia. His use of this name seems to be because of the gland’s proximity to the thyroid cartilage. The term thyroid has been applied to the major cartilage of the larynx dating back at least to the time of Galen. Thyroid derives from the Greek words thyreos, meaning shield, and eidos, meaning shape, form, or likeness. The thyreos is a narrow, oblong military shield, and its name derives from thyra, the Greek word for door. The thyroid cartilage indeed has a shield-like appearance.
Wharton considered the thyroid to be a pair of glands and described them as resembling an oblong fig or pear. He thought their principal function was uptake of superfluous fluids of the recurrent nerve. Other putative functions included warming the adjacent cartilages, lubricating the larynx, and contributing to the roundness and beautification of the neck.1 Considerable advances in our understanding of the thyroid gland have occurred since the 17th century.
MACROANATOMY
Basic Anatomy
The thyroid gland is located in the lower anterior region of the neck at the level of C5-C7 vertebrae. It is a bilobed organ joined by an isthmus and encased in a thin fibrous capsule. The right and left lobes have a somewhat conical shape with convex anterior and lateral surfaces. The lobes tend to be about 4 to 5 cm in length, 2 to 3 cm in greatest transverse dimension, and 1.5 to 2 cm in greatest anterior-posterior dimension. The isthmus is about 1 cm in greatest transverse and vertical dimensions. The location of the isthmus is variable, but it usually joins the two lateral lobes at the level of the second and third tracheal rings.
Approximately half of all thyroid glands exhibit a pyramidal lobe, with most studies reporting an incidence in the 30% to 75% range (Fig. 1.1).2 Some of the variation in incidence may relate to the variable size and prominence of the lobe, and hence threshold of recognition. The pyramidal lobe represents the remnant of the inferior portion of the thyroglossal duct. The lobe extends superiorly from the isthmus and may be attached to the hyoid bone by fibrous tissue. Pyramidal lobes are more frequently attached to the left side of the isthmus and in some cases attached to the left lobe itself.2
The tubercle of Zuckerkandl is a focal enlargement along the lateral border of the lateral lobes that is commonly observed during thyroid surgery.3 It ranges from a slight thickening to a 1 cm or larger nodular structure. It can be found on either side or bilaterally. It has utility as a surgical landmark because the recurrent laryngeal nerve usually courses medially, sometimes in a cleft between the tubercle and the main substance of the lateral lobe. In addition, the superior parathyroid gland is commonly found just cephalad to the tubercle.
Normal Weight
Studies examining the weight of normal thyroid glands, either by direct measurement or by extrapolation from volume measurement, have yielded variable means and ranges, particularly the latter.4,5,6,7,8 Distillation of these findings yields an average weight of about 18 g for adult men and 15 g for adult women. The reported distributions of thyroid weights tend to show a positive skew, with a broader range of weights above the mean than below. Most of the reported weights of normal adults lie within a range from 8 to 30 g. Glands with weights in excess of 50 g have also been reported, but these outliers raise questions regarding their normal status. The glands of adult women tend to be smaller than that of adult men, but the differences are modest and the ranges mostly overlap. Some studies have shown a positive correlation between thyroid weight and body weight, body mass index, or age.4,5,6,7,8,9 Body weight or body mass index tends to show stronger correlation than age, but overall these correlations are weak. Thyroid weight tends to show a progressive increase in childhood and adolescence, stability in early to midadulthood, and gradual decline in older age.7,8 An increase in thyroid size has been reported in pregnant women.10,11 However, most cases of enlargement may reflect iodine deficiency as opposed to an invariable physiologic response to pregnancy.
Anatomic Relationships
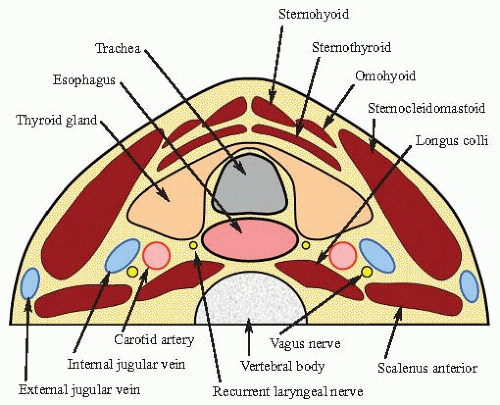
The medial surfaces of the lobes abut the thyroid cartilage of the larynx and superior aspect of the trachea. The apices of the lobes are located near the oblique line of the thyroid cartilage and the bases at the level of the fourth, fifth, or sixth tracheal ring. The superomedial aspects of the lateral lobes are adjacent to the inferior pharyngeal constrictors and posterior portions of the cricothyroid muscles. The common carotid artery, internal jugular vein, and vagus nerve, encased within the carotid sheath, course along the posterolateral aspects of the lateral lobes (Fig. 1.2). The recurrent laryngeal nerves are located in the tracheoesophageal grooves in proximity to the posteromedial aspects of the lateral lobes. The superior branch of the external laryngeal nerve usually courses to the cricothyroid muscle immediately posterior to the superior poles of the lateral lobes.
The thyroid gland is encased by the pretracheal fascia, anchoring the gland to the trachea and correlating with the movement of the gland during swallowing. The sternothyroid muscle is located immediately anterior to the thyroid, spanning from the oblique line of the thyroid cartilage to the manubrium of the sternum. Muscles anterior to the sternothyroid are the sternohyoid, superior belly of the omohyoid, and the anterior border of the sternocleidomastoid. The thyrohyoid muscle is essentially a superior extension of the sternothyroid, extending from the oblique line of the thyroid cartilage to the hyoid bone.
Vascular Supply
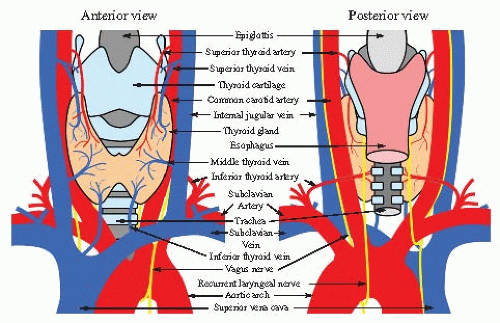
The blood supply to the thyroid is through the right and left superior thyroid arteries and the right and left inferior thyroid arteries (Fig. 1.3). The superior thyroid arteries derive from the external carotid arteries, and the inferior thyroid arteries derive from the subclavian arteries through the thyrocervical trunks. An inconstant artery, the thyroidea ima, occasionally arises from the brachiocephalic trunk, aortic arch, or left common carotid and ascends along the anterior midline of the trachea to reach the thyroid in the region of the isthmus. Venous drainage is through a plexus that leads to the superior, middle, and inferior thyroid veins. The superior and middle veins drain into the internal jugular veins, and the inferior veins join the brachiocephalic veins. A dense capillary plexus encompassing the follicles lies between the arterial and venous vessels.
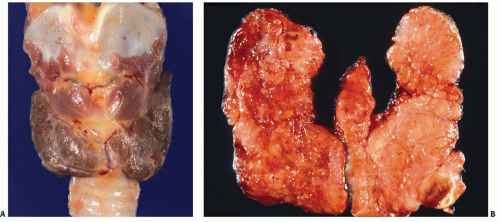 FIGURE 1.1. Gross photographs of thyroid glands. A: Bilobed thyroid and its relationship to the thyroid cartilage. B: Thyroid with prominent pyramidal lobe. |
Lymphatic Drainage
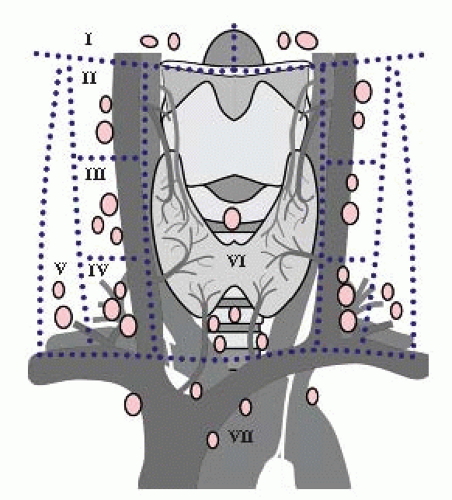
The lymphatic drainage flows from vessels in the perifollicular connective tissue to a subcapsular network. Lymphatic vessels leave the gland in proximity to veins and extend to several regional lymph nodes (Fig. 1.4). The most proximate nodes are located in the anterior, or central, compartment of the neck and collectively compose the level VI nodes. These include those immediately adjacent to the thyroid gland (perithyroidal or pericapsular nodes), prelaryngeal, pretracheal, and paratracheal lymph nodes. A midline prelaryngeal node found anterior to the cricothyroid membrane and superior to the isthmus is known alternatively as the Delphian node. Lymphatic drainage involves other regional lymph nodes including the internal jugular (particularly levels III and IV), superior mediastinal, supraclavicular, spinal accessory, retropharyngeal, and, to a limited extent, the submandibular and submental (level I) lymph nodes.
Innervation
The thyroid is innervated by nerves originating from the superior and middle sympathetic cervical ganglia. These nerves release noradrenaline from interfollicular adrenergic nerve terminals.12 Cholinergic nerve fibers also have been demonstrated in the thyroid, suggesting a role of the parasympathetic nervous system in the regulation of thyroid function.13
MICROANATOMY
The Follicle
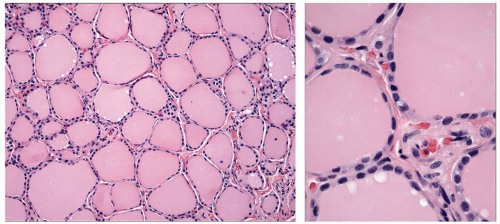
The follicle is the distinctive basic unit of the thyroid gland (Fig. 1.5). It is a spherical structure that usually has a polyhedral appearance because of the abutment of adjacent follicles. Each follicle is lined by a single layer of follicular cells with apices in contact with a central extracellular collection of colloid. The bases of the follicular cells lie along a thin fibrovascular stroma rich in a capillary network that encompasses the follicle. Normal thyroid glands usually contain between 500,000 and 1.5 million follicles.7 The size of most normal follicles lies in the range of 50 to 500 µm with an average size of about 200 µm. Thyroid lobules are formed by groups of 20 to 40 follicles. The lobules are invested by a thin layer of fibrous connective tissue, and each is supplied by small arterial branch. The fibrous tissue dividing the lobules is eventually contiguous with the capsule of the gland.
Colloid
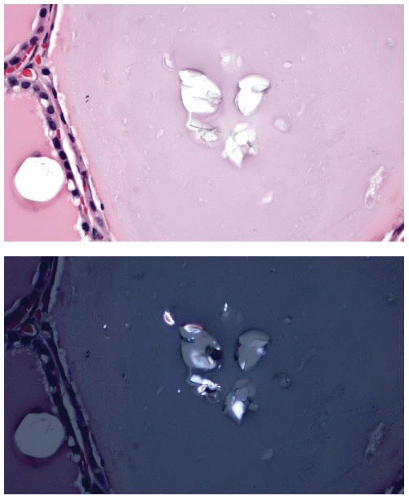
The colloid within the central follicular space contains thyroglobulin, an iodinated glycoprotein that is the precursor of triiodothyronine (T3) and thyroxine (T4). Colloid has an amorphous eosinophilic appearance and is highlighted by periodic acid-Schiff and thyroglobulin stains. The intensity of staining with hematoxylin and eosin can vary. The colloid in follicles with low activity usually shows more intense eosinophilia compared with the colloid in follicles with a high level of hormone synthesis and release. Colloid in these latter follicles may also show scalloping or small vacuoles at the interface with follicular cells, a sign of endocytotic resorption. Larger, round to oval clear spaces are common within colloid, and some of these spaces may contain calcium oxalate crystals. Colloid generally has a homogeneous appearance. However, it can contain particulate-like clumps of material that are more intensely eosinophilic or slightly basophilic (Fig. 1.6). This histologic finding seems more common in active follicles, but it is unclear whether this is a manifestation of increased synthetic activity or a nonspecific artifact.14
Crystals
The presence of calcium oxalate crystals within colloid is a common finding.15,16 Crystals appear as small clear refractile foci and are birefringent when viewed with polarizing filters (Fig. 1.7). These crystals begin to appear during childhood and adolescence and become more prevalent as adults age. Calcium oxalate crystals have potential utility in distinguishing thyroid from parathyroid tissue.17
Follicular Cells
Follicular cells have eosinophilic cytoplasm and round to slightly oval nuclei. The nuclei are located basally and have finely granular chromatin and inconspicuous nucleoli. Follicular cells vary in size and shape from low cuboidal to columnar, and this correlates with their level of thyroid hormone synthesis (Fig. 1.8). Cells with a low synthetic level have a low cuboidal appearance, and relatively abundant colloid occupies the lumen. This appearance of
follicles is sometimes designated the resting state. In contrast, follicular cells stimulated to produce more thyroid hormone exhibit columnar morphology. Histologic sections of normal adult thyroid glands usually show follicular cells with cuboidal to low cuboidal features.
follicles is sometimes designated the resting state. In contrast, follicular cells stimulated to produce more thyroid hormone exhibit columnar morphology. Histologic sections of normal adult thyroid glands usually show follicular cells with cuboidal to low cuboidal features.
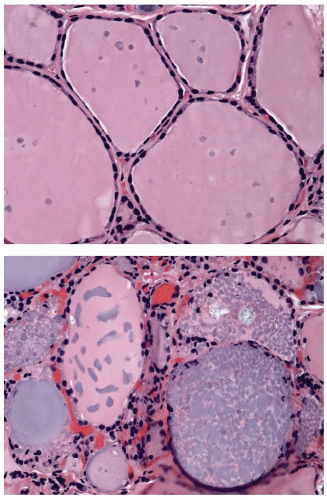 FIGURE 1.6. Photomicrographs showing particulate material within colloid. The top image shows a relatively subtle accumulation, whereas the bottom image is an extreme example of the phenomenon. |
Ultrastructure
Ultrastructural examination of follicular cells reveals junctional complexes of desmosomes and terminal bars linking cells along their lateral borders near the apices. The bases of the cells abut a basal lamina that separates them from the interstitial stroma and fenestrated capillary network (Fig. 1.9). The nuclei are basally located. Granular endoplasmic reticulum and mitochondria are readily identifiable components of the cytoplasm. The supranuclear region contains a Golgi complex that increases in prominence with increased activity. The apical region contains Golgi-derived dense secretory vacuoles, which transport glycoproteins to the plasmalemma for exocytosis into the follicular lumen. Lysosomes are prominent cytoplasmic components. This includes both primary and secondary lysosomes. The latter, also known as phagolysosomes, represents the fusion of primary lysosomes with colloid taken into the cytoplasm by endocytosis. Numerous apical microvilli are present, and their length increases when hormonal synthesis is stimulated.
Immunohistochemistry
Follicular cells exhibit cytoplasmic positivity in sections immunohistochemically stained for thyroglobulin and low molecular weight cytokeratins (Fig. 1.10).18,19,20,21 Coexpression of vimentin has also been noted.18,19,20 Normal follicular cells express transcription factors including thyroid transcription factor-1 (TTF1), TTF2, and paired box gene 8 (PAX8).22,23 Thyroid stimulating hormone (TSH) receptor and thyroid peroxidase (TPO) can also be demonstrated immunohistochemically in normal follicular cells.22,24,25 Growth factors and their receptors are also expressed, including epidermal growth factor (EGF), transforming growth factor (TGF(α)), and epidermal growth factor receptor (EGFR) (Table 1.1).26,27
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree