Table 31-1. Selected Examples of Nonprescription Cough Products
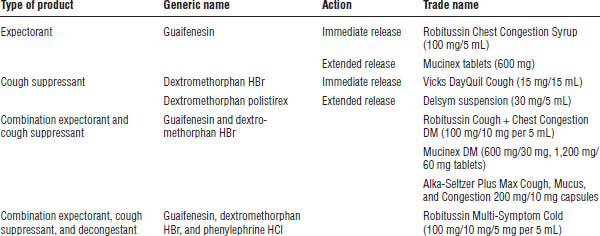
■ Product availability: Lozenge, ointment, steam inhalation
■ Patient education: Ointment and solution are toxic if ingested.
Sore throat remedies
Sore throat remedies include the following:
■ Saline gargle
■ Sprays and lozenges:
• Benzocaine: Chloraseptic and Cepacol lozenges
• Dyclonine: Sucrets Maximum Strength lozenges
• Phenol: Chloraseptic spray
• Menthol: Vicks VapoDrops
Special populations
Pregnancy
■ Dextromethorphan is viewed as probably safe.
Lactation
■ Dextromethorphan, guaifenesin, and topical anesthetics are all low risk.
■ Patients may want to avoid diphenhydramine because it is excreted into breast milk and may also decrease milk production.
Common Cold
Clinical presentation
■ Sore throat, nasal symptoms, watery eyes, sneezing, cough, malaise, and low-grade fever occur.
■ There is a gradual onset with slow progression.
■ Duration is 1–2 weeks.
Prevention
■ Frequent hand cleansing
■ Sanitizers
Treatment
Nonpharmacologic therapy
■ Humidifiers
■ Increased fluid intake
■ Rest
■ Propping head upright
■ Rubber bulb nasal syringe for children < 4 years of age
■ Irrigation of nose with saline drops or mist
Nonprescription medication treatment (symptomatic)
■ Decongestants for nasal congestion
■ Antihistamines used in combination with a decongestant for excess nasal discharge (not effective as monotherapy for treatment of colds)
■ Analgesics for related pain or headaches
■ Local anesthetic lozenges or sprays for sore throat (pharyngitis)
Allergic Rhinitis
Clinical presentation
■ Nasal: Congestion, rhinorrhea, nasal pruritus, sneezing, postnasal drip
■ Ocular: Itching, lacrimation, redness, irritation
■ General: Headache, malaise, mood swings, irritability
Treatment
Nonpharmacologic therapy
Patients should avoid the offending allergens:
■ Limit outside exposure during periods of high pollen.
■ Avoid indoor and outdoor mold.
■ Avoid dust, especially in the bedroom.
■ Avoid pet dander, especially from cats.
Nonprescription Therapy for Treatment of the Common Cold and Allergies
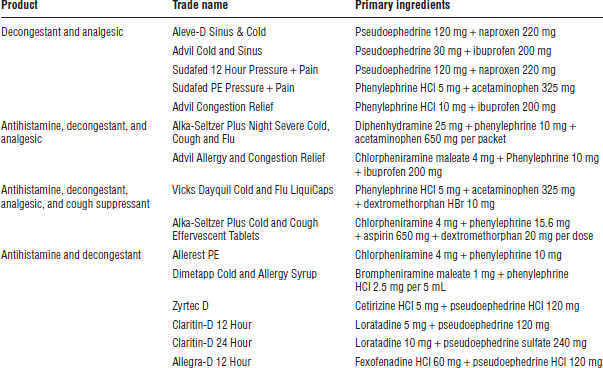
Selected products for treating the common cold and allergies are shown in Tables 31-2, 31-3, and 31-4.
Antihistamines
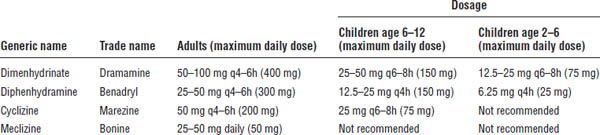
Selected antihistamines are described in Table 31-2.
Table 31-2. Selected Nonprescription Antihistamine Products
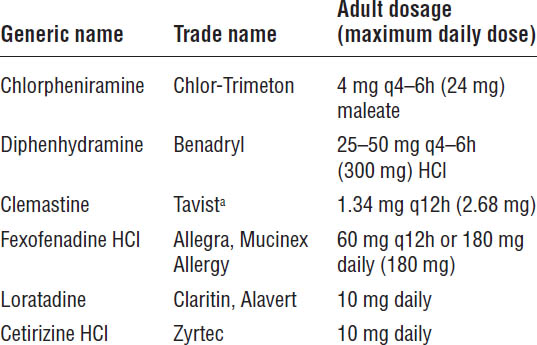
a. Brand name is no longer manufactured in the United States.
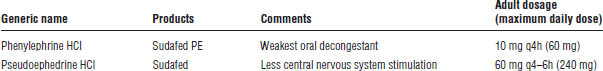
Table 31-3. Selected Nonprescription Oral Decongestant Products
Pharmacology
■ Antihistamines are H1-receptor antagonists.
■ First-generation antihistamines are nonselective and sedating.
■ Second-generation antihistamines are peripherally selective and have a low incidence of sedation.
Side effects
■ Sedation (primarily with first-generation antihistamines)
■ Anticholinergic effects
• Dry mouth
• Dry eyes
• Urinary retention
• Constipation
• Paradoxical stimulation in some children and elderly patients
Precautions and contraindications
■ Do not drive or operate heavy machinery.
■ Avoid use with alcohol.
■ Prostatic hyperplasia can occur.
■ Narrow-angle glaucoma is possible.
Intranasal corticosteroid
Triamcinolone acetonide (Nasacort Allergy 24HR) pharmacology
■ Decreases the influx of inflammatory cells and inhibits the release of cytokines, thereby reducing inflammation of the nasal mucosa
Table 31-4. Selected Nonprescription Cold, Allergy, and Sinus Combination Products
■ Considered first-line therapy for moderate to severe allergic rhinitis
■ More effective than antihistamines, especially for treatment of late allergic rhinitis symptoms such as nasal congestion
Dosing
■ Age 2–12 years: Initiate at 1 spray in each nostril daily (110 mcg/day).
• If symptoms are not relieved:
▪ Age 2–5: Refer to primary care provider (PCP).
▪ Age 6–12: Increase dose to 2 sprays in each nostril daily.
■ Age ≥ 12 years: Initiate at 2 sprays in each nostril daily (220 mcg/day).
• Once symptoms are controlled, patient may be able to titrate down to 1 spray in each nostril daily.
Side effects
■ Nasal discomfort
■ Nasal irritation, dryness, or both
■ Epistaxis
■ Stinging, burning, or both
■ Sneezing
■ Headache
■ Bitter taste
■ Rhinitis medicamentosa
Precautions and contraindications
■ If patient plans on using triamcinolone acetonide longer than 2 months per year, encourage patient to see PCP.
■ Concerns regarding the more serious side effects:
• Changes in vision, cataracts
• Increased risk of infection in adults
• Growth inhibition in children
Oral decongestants
Selected oral decongestant products are described in Table 31-3.
Pharmacology
■ α-adrenergic agonists and vasoconstrictors
■ Constriction of blood vessels to decrease blood supply to nasal mucosa and decrease mucosal edema
■ No effect on histamine or allergy-mediated reaction
Regulation
The 2005 Combat Methamphetamine Epidemic Act has the following requirements:
■ Pseudoephedrine must be kept either behind the counter or in a locked cabinet.
■ Quantity is limited to 3.6 g/day and 9 g/month per patient.
Side effects
These products are relatively safe with no dependence. They can be used long term, with the most common side effects as follows:
■ Nervousness
■ Irritability
■ Restlessness
■ Insomnia
Precautions and contraindications
■ Hypertension: These agents are generally accepted with mild or well-controlled hypertension; they should not be used with uncontrolled hypertension.
■ Heart disease (arrhythmias and ischemic heart disease): They increase the heart rate.
■ Diabetes: They have a minimal effect on blood sugar level.
■ Hyperthyroidism: This condition is more sensitive to sympathomimetics.
■ Enlarged prostrate: Benign prostatic hyperplasia (BPH) is exacerbated by constricting smooth muscle of the bladder neck.
■ Narrow-angle glaucoma: Dilation increases intraocular pressure.
■ Blood pressure: MAO inhibitors interact with decongestants to increase blood pressure.
Topical decongestants
Pharmacology
■ α-adrenergic agonists act locally as vasoconstrictors.
■ These agents constrict blood vessels, decrease blood supply to the nose, and decrease mucosal edema.
■ They have no effect on histamine or allergy-mediated reaction.
Side effects
Minimal systemic absorption results in few side effects. Local effects may include burning, nasal irritation, and sneezing.
Precautions and contraindications
Rhinitis medicamentosa (rebound congestion) may occur if duration of use is > 3–5 days. The FDA recommends using these products no more than 3 days in duration.
Dosage forms of topical decongestants
Sprays
Sprays are the simplest dosage delivery. A large surface area is covered. Imprecise dosing and contamination of the bottle are possible. Products include the following:
■ Short-acting: Phenylephrine HCl (Neo-Synephrine)
■ Longest-acting: Oxymetazoline HCl (Afrin, Vicks Sinex)
Drops
Drops are preferred for use in small children. They cover a small surface area. They pass to the larynx, where they may be swallowed and result in systemic effects.
Nasal inhaler
A nasal inhaler requires an unobstructed airway to deliver drug to the nasal mucosa. Nasal inhalers contain sympathomimetic amines, as well as camphor and menthol. Medications lose efficacy after 2–3 months. Products include the following:
■ Propylhexedrine (Benzedrex inhaler)
Nasal saline solution
This solution is very safe and is good for use in infants and children to remove dried, encrusted, or thick mucus from the nose while also moisturizing and soothing nasal passages. It can be used with oral decongestants. Products include the following:
■ Saline drops (Ayr)
■ Saline sprays (Ayr, Ocean Nasal Spray)
■ Neti pot
Mast cell stabilizer
Cromolyn (Nasalcrom)
■ Pharmacology: Prevention of the release of inflammatory mediators from mast cells
■ Dosage: One spray per nostril q4–6h
■ Onset of action: Approximately 1 week; 2–4 weeks for maximal effect
■ Efficacy: Not efficacious if taken prn; must be taken on a scheduled basis and is more effective if started at least 1 week prior to symptom onset
■ Side effects: Nasal irritation, nasal burning, stinging, sneezing, cough, unpleasant taste
Analgesics
Analgesics treat the pain, fever, and headaches associated with cold, flu, or allergies. Medications include the following:
■ Aspirin (mostly replaced now by acetaminophen and nonsteroidal anti-inflammatory drugs [NSAIDs])
■ Acetaminophen (N-acetyl-para-aminophenol, or APAP)
■ NSAIDs
• Ibuprofen (OTC not approved for children < 6 months of age)
• Naproxen (OTC not approved for children < 12 years of age)
Special populations
Children
■ Do not use cough and cold products in children < 4 years of age.
■ All children < 12 years of age are excluded from self-care of allergy unless they have been diagnosed by a health care provider and are approved for nonprescription therapy.
■ Second-generation antihistamines and intranasal corticosteroids can be used for self-care in children < 6 years of age (provided they have been diagnosed by a health care provider and approved for nonprescription therapy).
Pregnancy
■ Avoid products containing pseudoephedrine in the first trimester.
■ Oxymetazoline is the preferred topical decongestant.
■ For allergy, cromolyn is considered first-line therapy, followed by the second-generation antihistamines: loratadine and cetirizine. Chlorpheniramine can also be used.
Lactation
■ Avoid using the following topical decongestants: xylometazoline and naphazoline.
■ All antihistamines can decrease milk production.
■ For allergy, cromolyn is considered first-line therapy, followed by loratadine and chlorpheniramine.
31-4. Constipation
Clinical Presentation
■ Patient has difficult or infrequent passage of stools.
■ Patient may complain of abdominal or rectal fullness.
Etiology
Table 31-5 shows the common causes of constipation.
Treatment
Nonpharmacologic therapy
■ Increase fluid intake.
■ Increase dietary fiber.
■ Exercise.
■ Establish good bowel habits.
Table 31-5. Common Causes of Constipation
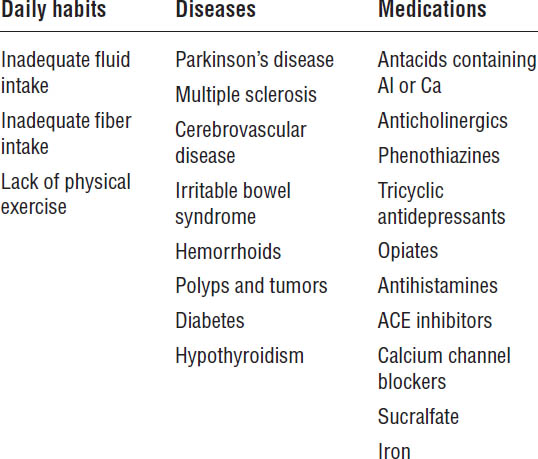
ACE, angiotensin-converting enzyme.
Nonprescription medication therapy
Bulk-forming laxatives
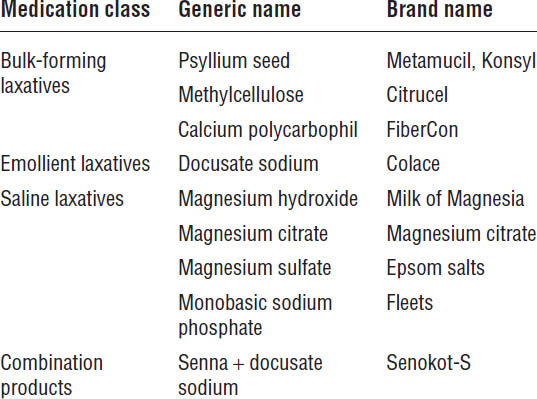
Selected bulk-forming laxative products are described in Table 31-6.
Mechanism of action
Natural or semisynthetic hydrophilic polysaccharide derivatives are present in bulk-forming laxatives. They absorb water to soften stool, increase bulk, and facilitate peristalsis and elimination. Onset of effect may not be seen for 2–3 days.
Role in therapy
Bulk-forming laxatives are the safest, most natural therapy for normal transit constipation. They are the most often recommended medication for chronic use. Use caution in patients with fluid restriction (i.e., renal dysfunction, heart failure), narcotic-associated dysmotility, and fecal impaction.
Drug interactions
■ These laxatives may bind with digoxin, warfarin, and other drugs.
■ Calcium complexes may bind with tetracycline, inhibiting its absorption.
■ Recommend separating doses from other medications by 1–2 hours.
Side effects
■ Dose should be increased gradually over several weeks to avoid bloating, flatulence, and abdominal pain.
Table 31-6. Additional Nonprescription Treatments of Constipation Not Listed in Text
■ These laxatives can cause bowel obstruction if not taken with sufficient amounts of water.
■ Caution diabetics about sugar content of some products.
Emollient laxatives (stool softeners)
Emollient laxatives act as surfactants, absorbing water into the stool. Onset of effect may take 2–3 days. Emollient laxatives may cause systemic absorption of mineral oil; therefore, concurrent use is contraindicated.
Emollient laxatives are often used in combination products. They are useful in situations when straining should be avoided, such as following rectal surgery, during the postpartum time period, and following a recent myocardial infarction.
Selected emollient laxative products are described in Table 31-6.
Stimulant laxatives
Stimulant laxatives stimulate bowel motility through localized mucosal irritation. They increase secretion of fluids into the bowel. Impaired colon function occurs with chronic use.
Dangers of chronic stimulant laxative use include the following:
■ Laxative habit
■ Cathartic colon
■ Melanosis coli
■ Loss of fluids and electrolytes
■ Cramping pains
Anthraquinones
Senna (Senokot and Ex-Lax) is an anthraquinone:
■ Pharmacology: Anthraquinones are absorbed into the bloodstream with action on the large intestines. Onset of effects is 6–12 hours. This medication should be taken at bedtime.
■ Side effects: Such effects include discoloration of urine, stimulant habituation, and melanosis coli (i.e., dark pigmentation of colonic mucosa).
Diphenylmethanes
Bisacodyl (Dulcolax tablets or suppositories) is a diphenylmethane. Minimal systemic absorption occurs with this drug. This medication is enteric coated; do not crush or take with antacids. The onset of effects varies with route of administration:
■ Oral: 6–8 hours
■ Rectal: 15–60 minutes
Stimulant oils
Castor oil acts on the small intestine. It is a strong cathartic and may induce fluid or electrolyte disturbances. Onset is rapid: 2–6 hours.
Hyperosmotic laxatives
Glycerin
Glycerin has an osmotic effect and is a local irritant that stimulates bowel movement. Onset of effect is usually within 30 minutes.
Products include Fleet Pedia-Lax Liquid Glycerin Suppository and Fleet Glycerin Suppository.
Polyethylene glycol 3350 (MiraLAX)
Polyethylene glycol (PEG) 3350 has a mechanism of action similar to that of glycerin. This agent is meant for short-term therapy for constipation. Onset of action is usually within 1–3 days. The adult dosage is 17 g of powder in 4–8 oz of water. Side effects are as follows:
■ Bloating
■ Abdominal discomfort
■ Cramping
■ Flatulence
Saline laxatives
With saline laxatives, nonabsorbable cations create osmotic gradient to pull water into the intestine. Onset varies depending on the route of administration:
■ Rectal: 5–30 minutes
■ Oral: 30 minutes to 4 hours
Twenty percent of magnesium may be absorbed systemically. Saline laxatives are contraindicated in patients with impaired renal function (magnesium-or phosphate-containing), congestive heart failure, or hypertension (sodium-containing). Selected saline laxative products are described in Table 31-6.
Enemas
Enemas include Fleet Enema (monobasic and dibasic sodium phosphates). They are typically used for acute treatment (fecal impaction), not for long-term management of constipation.
Lubricant laxatives
Selected lubricant laxative products are as follows:
■ Mineral oil: Liquid petrolatum
■ Olive oil: “Sweet oil”
Lubricant laxatives soften the feces by emulsifying the contents of the intestinal tract. Onset of action is 6–8 hours. Use in self-care is strongly discouraged because of high risk of adverse events in children and the elderly. Do not administer with stool softeners.
Special patient populations
Children
■ Mild constipation can be treated with increases in fluids and/or fruit juices containing sorbitol, such as apple, pear, prune, apricot, nectarine, or peach juice.
■ Increase dietary fiber intake.
■ For children 2–6 years of age, the following products are approved for use:
• Rectal: Glycerin suppositories
• Oral: Docusate sodium or magnesium hydroxide
■ For children 6–12 years of age, the following products are approved for use:
• Rectal: Glycerin or bisacodyl suppositories
• Oral: Bulk-forming laxatives, docusate, and magnesium hydroxide are preferred; oral stimulants (senna, bisacodyl) should be reserved for when preferred treatments fail.
■ For patients 6–17 years of age, one could apply off-label use of PEG 3350 at doses of 1 g/kg daily (not to exceed 17 grams daily), but a health care provider must be involved with the care of this patient.
■ For patients > 17 years of age, PEG 3350 is FDA approved for use.
Pregnancy
■ Attempt dietary changes first by incorporating more fiber via prunes or prune juice.
■ If dietary changes do not work, use bulk-forming laxatives with sufficient amounts of water.
■ For complaints of primarily dry, hard stools, use docusate.
■ Senna or bisacodyl can be used safely short term and have more data supporting their use than does PEG 3350, but some experts use PEG 3350 as first-line treatment.
■ Avoid castor oil (causes uterine contractions) and mineral oil (impairs maternal fat-soluble vitamin absorption).
Lactation
■ Senna, bisacodyl, PEG 3350, and docusate are all compatible with breast-feeding.
■ Avoid castor oil and mineral oil.
31-5. Diarrhea
Clinical Presentation
Diarrhea is the abnormal increase in frequency of stools and stool looseness. It may be acute (< 14 days) or chronic (> 4 weeks).
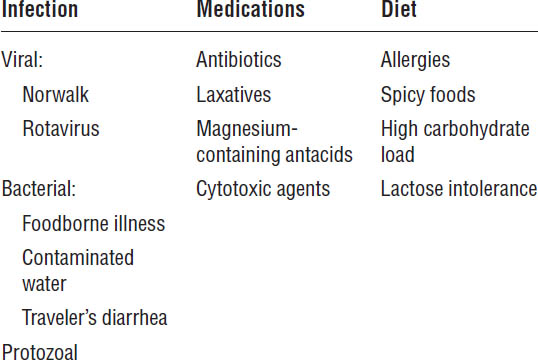
Etiology
Common causes of diarrhea are shown in Table 31-7.
Complications
■ Dehydration (especially in infants and elderly patients)
■ Electrolyte abnormalities
Nonpharmacologic Treatment
■ Administer oral rehydration therapy, such as Pedialyte.
■ Avoid fatty and spicy foods and foods with high sugar content.
Nonprescription Medication Therapy
Loperamide HCl (Imodium AD)
Loperamide is a synthetic opioid agonist that slows GI motility. The dosage is 4 mg initially and then 2 mg after each loose stool. For OTC use, maximum dose is 8 mg/day. The pharmacist may encounter cancer patients for whom the oncologist has recommended loperamide 2 mg po q2h with a maximum dose of 16 mg/day for chemotherapy-induced diarrhea not caused by irinotecan and 24 mg/day for chemotherapy-induced diarrhea caused by irinotecan, though both of these maximum doses are intended for no more than 24 hours.
Table 31-7. Common Causes of Diarrhea
The medication is well tolerated, but typical side effects are as follows:
■ Constipation
■ Dizziness
■ Dry mouth
Precautions and contraindications are as follows:
■ Loperamide is not recommended for children < 6 years of age without medical supervision.
■ It should not be used if the patient has bloody or black stool; consult a health care provider before use if the patient has a fever, mucus in stool, or a history of liver disease.
■ Antiperistaltic action could worsen effects of invasive or inflammatory bacterial infection.
Bismuth subsalicylate (Pepto-Bismol)
Bismuth subsalicylate reacts with stomach acid to form salicylic acid and bismuth oxychloride. It reduces frequency of diarrhea and improves stool consistency. It has a direct antimicrobial effect; therefore, it is effective in traveler’s diarrhea.
Side effects include the following:
■ Salicylate toxicity (tinnitus)
■ Bismuth toxicity (neurotoxicity)
■ Gray-black discoloration of tongue or stool
The medication is contraindicated in the following:
■ Aspirin allergy
■ Children and teens with viral illness (Reye’s syndrome)
■ Patients having a history of GI bleeding or using warfarin
31-6. Nausea and Vomiting
Physiology
Vomiting is coordinated by the vomiting center in the medulla. Stimuli from the peripheral nervous system and within the central nervous system (CNS) act on the vomiting center. Responding to these impulses, the vomiting center stimulates the abdominal muscles, stomach, and esophagus to induce vomiting.
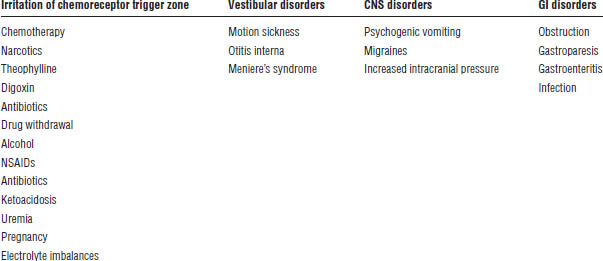
Etiology
Common causes of nausea and vomiting are shown in Table 31-8.
Complications
■ Dehydration
■ Electrolyte imbalance
■ Aspiration
Table 31-8. Common Causes of Nausea and Vomiting
■ Acid–base disturbances
Nonprescription Medication Therapy
In addition to the medications described in this section, Table 31-9 describes nonprescription drugs of choice for the nausea or vomiting associated with motion sickness.
Antihistamines
Antihistamines cross the blood-brain barrier to depress vestibular excitability.
Phosphorated carbohydrate solution (Emetrol)
This agent is a hyperosmolar solution of levulose (fructose), dextrose (glucose), and phosphoric acid. It is buffered to a pH of 1.5. It reduces gastric muscle contraction through an unknown direct effect. It must not be diluted (which raises the pH).
Bismuth subsalicylate (Pepto-Bismol)
Bismuth subsalicylate is available as nonprescription suspension, caplet, and chewable tablet. See Section 31-5 for additional information.
Histamine 2–receptor antagonists
Histamine 2–receptor antagonists (H2RAs) may provide symptomatic relief by inhibiting gastric acid secretion. Potential drug interactions occur with cimetidine.
Side effects are as follows:
■ Headache
■ Constipation
■ Diarrhea
See Section 25-4 on peptic ulcer disease in Chapter 25 for additional information on H2RAs.
Antacids
Antacids may treat nausea, dyspepsia, and stomach upset associated with excessive intake of food or drink. They are combinations of magnesium hydroxide, sodium salts, aluminum hydroxide, calcium carbonate, and magnesium carbonate. The usual adult dosage is 15 mL 30 minutes after meals and at bedtime.
Side effects include the following:
■ Constipation
■ Diarrhea
■ Sodium overload
Antacids may decrease absorption of some medications. Therefore, administer other medications 1–2 hours before or after antacids.
Special patient populations
Pregnancy
Especially during the first trimester, nonpharmacologic therapy is recommended:
■ Ensure there is fresh air in the rooms where you sleep, prepare food, and eat.
■ Eat small, frequent meals.
■ Avoid rich, fatty foods.
■ Before getting out of bed in the morning, eat several dry crackers and relax for 10–15 minutes.
Refer the patient to the health care provider if pharmacologic therapy is being considered. Once the health care provider is involved in care, the following medications are preferred for use in pregnancy:
■ Antihistamines (meclizine, cyclizine, dimenhydrinate, diphenhydramine): All have a low risk of teratogenicity but should be reserved for those with severe symptoms unresponsive to nonpharmacologic measures.
Table 31-9. Nonprescription Drugs of Choice for Prevention of Motion Sickness
■ Pyridoxine (vitamin B6): 10–25 mg tid–qid
■ Doxylamine succinate: 12.5 mg tid–qid
■ Calcium-containing antacids
■ Ginger: There is evidence supporting its use in pregnancy (see Section 31-14 for herbal products).
31-7. Pain and Fever
Pathophysiology of Pain
Nociceptors are peripheral pain receptors. They send pain stimuli to the spinal cord through afferent, nociceptive nerves. Impulses then pass to the brain through dorsal root ganglia.
Pathophysiology of Fever
The core temperature is the temperature of the blood surrounding the hypothalamus. The thermoregulatory center in the anterior hypothalamus controls body temperature through physiologic and behavioral mechanisms. Pyrogens—fever-producing substances—increase the thermoregulatory set point, raising the body temperature.
Nonprescription Medication Therapy
Selected analgesic and antipyretic products are shown in Table 31-10.
Acetaminophen
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


