Fig. 19.1.
Acute spongiotic dermatitis with spongiotic microvesicles.
•
In acute spongiotic dermatitis, the epidermis retains its normal “basket-weave” stratum corneum. The epidermis also has pale keratinocytes and spongiosis with or without spongiotic microvesicles
•
In the dermis, there is papillary dermal edema and a superficial perivascular inflammatory infiltrate that is predominantly lymphocytic but often has admixed eosinophils
Subacute spongiotic dermatitis (Fig. 19.2)
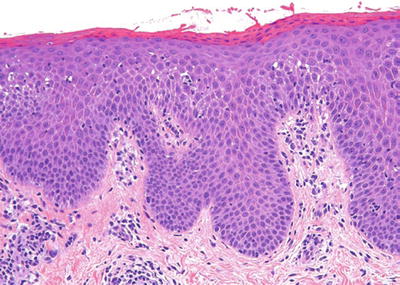
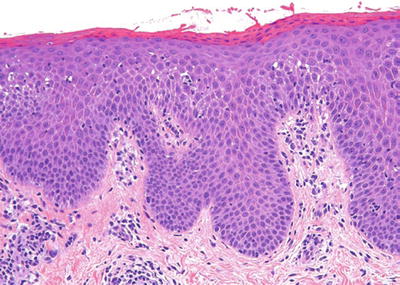
Fig. 19.2.
Subacute spongiotic dermatitis.
•
In subacute spongiotic dermatitis, the epidermis has parakeratosis, acanthosis, a diminished granular layer, and spongiosis
•
The findings in the dermis are similar to acute spongiotic dermatitis but usually with less edema
Chronic spongiotic dermatitis (Fig. 19.3)
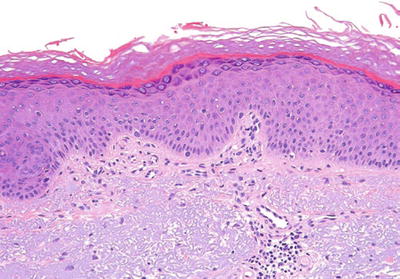
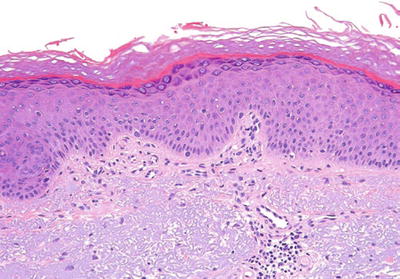
Fig. 19.3.
Chronic spongiotic dermatitis.
•
In chronic spongiotic dermatitis, the epidermis has acanthosis, hyperkeratosis, parakeratosis, an irregular granular layer, and only minimal to mild spongiosis
•
In the dermis, the papillary dermis may become fibrotic, and there is a variable perivascular inflammatory infiltrate
Eczematous Dermatitis
♦
Eczematous dermatitis is a clinical term that describes a papular to vesicular erythematous rash
♦
Distinct etiologies are not always apparent, but some have an identifiable cause (e.g., contact dermatitis)
♦
All have essentially indistinguishable histologic features and may have features of acute, subacute, or chronic spongiotic dermatitis
♦
Correlation with the clinical presentation is necessary
♦
The most common entities in the differential diagnosis of eczematous dermatitis are discussed below
Contact Dermatitis
Allergic Contact Dermatitis
Clinical
♦
Allergic contact dermatitis presents as pruritic erythematous papules and vesicles
♦
It is secondary to a type IV delayed hypersensitivity reaction
♦
Example: poison ivy
Microscopic
♦
The microscopic findings are those of typical spongiotic dermatitis
♦
Spongiotic microvesicles are a frequent finding, especially early in the course
♦
The presence of collections of Langerhans cells in the epidermis, also called Langerhans cell microabscesses, is suggestive of an allergic contact dermatitis
♦
In the dermis, there is a predominantly perivascular lymphocytic infiltrate with variable numbers of eosinophils
Irritant Contact Dermatitis
Clinical
♦
Irritant contact dermatitis presents as erythematous papules and vesicles
♦
It is secondary to a direct irritant effect of an offending agent
♦
Example: diaper rash
Microscopic
♦
There are subtle differences from allergic contact dermatitis
♦
There is ballooning degeneration of keratinocytes and focal necrotic keratinocytes
♦
In severe cases, there may be necrosis of the upper portion of the epidermis
♦
The inflammatory infiltrate is typically mild in nature
Atopic Dermatitis
Clinical
♦
Atopic dermatitis is characterized by a chronic, pruritic, relapsing papular dermatitis
♦
It is associated with history of asthma and allergic rhinitis (atopy)
♦
There is a predilection for flexural areas, especially in children
Microscopic
♦
Biopsies typically demonstrate subacute to chronic spongiotic dermatitis
Pompholyx (Dyshidrotic Eczema)
Clinical
♦
This is characterized by a symmetric vesicular eruption involving the hands and/or feet
Microscopic
♦
Biopsies typically demonstrate subacute to chronic spongiotic dermatitis
♦
Spongiotic microvesicles are common
♦
There may be features of either allergic contact or irritant contact dermatitis
Nummular Dermatitis (Nummular Eczema)
Clinical
♦
Nummular dermatitis presents as round to oval pruritic patches or plaques, usually involving the extremities
Microscopic
♦
Biopsies from early lesions show acute to subacute spongiotic dermatitis
♦
Biopsies from older lesions demonstrate chronic spongiotic dermatitis that may resemble psoriasis but with retention of granular layer, normal suprapapillary plate thickness, and hyperkeratosis (see Psoriasis below)
“Id” Reaction
Clinical
♦
This is an acute dermatitis that develops distal to a primary inflammatory focus
♦
The primary inflammatory lesion is frequently tinea pedis or impetiginized stasis dermatitis
Microscopic
♦
Biopsies demonstrate typical spongiotic dermatitis
Eczematous Drug Reaction
Clinical
♦
Approximately 5–10% of drug reactions may be eczematous in nature
Microscopic
♦
Biopsies from eczematous drug eruptions demonstrate spongiotic dermatitis
♦
Eosinophils may be more prominent in eczematous drug eruptions, but this is not specific
Vesicular Dermatophytosis
Clinical
♦
Vesicular dermatophytosis usually presents on the feet and resembles pompholyx (see above)
Microscopic
♦
The biopsy demonstrates spongiotic dermatitis and the presence of neutrophils in epidermis and/or stratum corneum
♦
In the dermis, eosinophils are usually conspicuous
♦
PAS or GMS stains highlight the fungal hyphae in the stratum corneum
Pityriasis Rosea
Clinical
♦
Pityriasis rosea usually presents in young adults as relatively asymptomatic patches and plaques
♦
It usually starts as a single round to oval salmon-colored herald patch that subsequently develops into a widespread, symmetric eruption on trunk that follows skin lines
Microscopic (Fig. 19.4)
♦
Microscopically it resembles subacute spongiotic dermatitis with discrete mounds of parakeratosis and rare scattered dyskeratotic keratinocytes
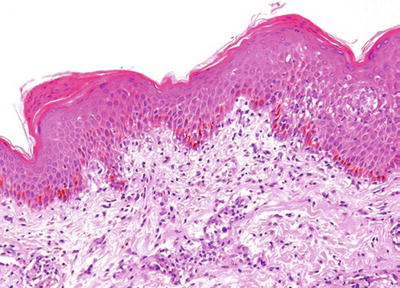
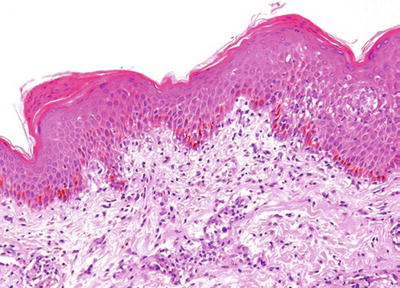
Fig. 19.4.
Pityriasis rosea.
♦
In the dermis, there is a mild to moderate mononuclear cell infiltrate often with some extravasation of erythrocytes in papillary dermis
Seborrheic Dermatitis
Clinical
♦
Seborrheic dermatitis affects the scalp (dandruff), ears, midface, and upper chest
♦
Lesions present as erythematous patches with greasy, yellow scale
♦
In AIDS patients and patients with neurologic disorders, it can be severe
Microscopic
♦
It is rarely biopsied, but biopsies usually show features of subacute or chronic spongiotic dermatitis
♦
A clue to the diagnosis is the presence of parakeratotic mounds, often with neutrophils, around follicular ostia
Stasis Dermatitis
Clinical
♦
Stasis dermatitis presents as an eczematous dermatitis of the lower extremities associated with underlying venous insufficiency
♦
The patient may also have associated venous stasis ulcers
Microscopic (Fig. 19.5)
♦
Biopsies demonstrate findings of subacute to chronic spongiotic dermatitis
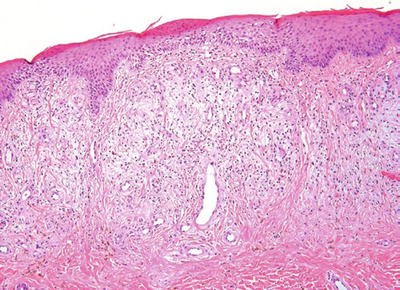
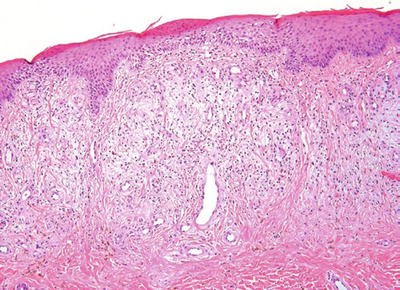
Fig. 19.5.
Stasis dermatitis.
♦
There is usually significant acanthosis of the epidermis
♦
The key histologic feature is the presence of lobular hyperplasia of superficial dermal blood vessels that is frequently accompanied by a mild perivascular lymphocytic infiltrate, extravasated erythrocytes, and siderophages
♦
Over time, the dermis becomes fibrotic
Psoriasiform Dermatitis
♦
Diseases associated with this pattern are characterized by epidermal acanthosis defined by elongation and widening of rete pegs
Psoriasis Vulgaris
Clinical
♦
Psoriasis vulgaris usually presents in second to third decades as erythematous plaques with silvery scale on extensor surfaces, scalp, gluteal cleft, and glans penis
♦
Nail findings including pitting and yellow discoloration are a frequent clinical finding
♦
Psoriatic arthritis is present in 1–5% of patients, generally in patients with severe cutaneous disease
Microscopic (Fig. 19.6)
♦
Psoriasis vulgaris is characterized by uniform acanthosis with elongated rete ridges and prominent parakeratosis
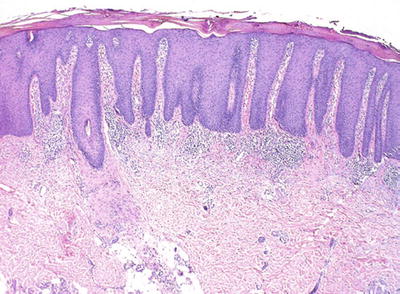
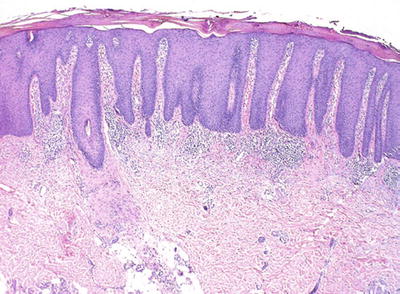
Fig. 19.6.
Psoriasis vulgaris.
♦
The granular layer is absent or diminished
♦
There are collections of neutrophils in stratum corneum (Munro microabscesses) and/or epidermis (pustules of Kogoj)
♦
Other findings include suprapapillary plate thinning and dilated, tortuous papillary dermal blood vessels
♦
Within the dermis, there is a superficial perivascular lymphocytic infiltrate that may contain neutrophils
♦
Eosinophils are not present in the dermal infiltrate of psoriasis, and their presence is against the diagnosis
Differential Diagnosis
♦
Includes nummular dermatitis, contact dermatitis, seborrheic dermatitis, and pityriasis rubra pilaris. In the first two considerations, the epidermis shows more irregular acanthosis and more spongiosis and often has eosinophils as part of the infiltrate. In seborrheic dermatitis, the clinical presentation differs and the parakeratosis with neutrophils is usually restricted to follicular ostia, but there are cases of so-called sebopsoriasis in which the clinical and histologic overlap precludes distinction. Pityriasis rubra pilaris may show a similar pattern of acanthosis but lacks neutrophils and has a granular layer
Psoriasis Variants
Drug-Induced Psoriasis
Clinical
♦
Patients treated with TNF-α inhibitors, especially in the setting of inflammatory bowel disease, can develop psoriasiform dermatitis
Microscopic
♦
Resembles psoriasis vulgaris, except eosinophils that are usually present
Pustular Psoriasis
Clinical
♦
Pustular psoriasis may be associated with pregnancy or discontinuation of systemic steroids in patients with known psoriasis
♦
The lesions are characterized by the acute onset of sterile pustules rather than large erythematous plaques
Microscopic (Fig. 19.7)
♦
Biopsy findings are characterized by large unilocular pustules in the stratum corneum/epidermis
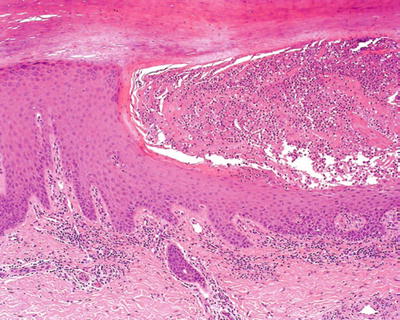
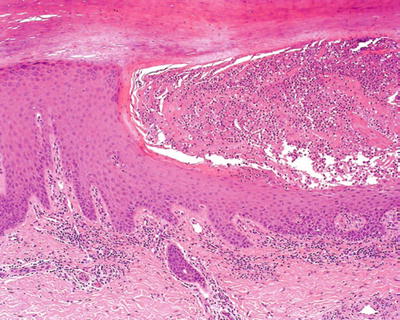
Fig. 19.7.
Pustular psoriasis.
♦
Because of the rapid nature of the onset, the epidermis has an intact or slightly diminished granular layer and has less prominent acanthosis
Differential Diagnosis
♦
Includes candidiasis, eczematous dermatitis with secondary impetiginization, and Reiter syndrome. In the first two considerations, there is more spongiosis and usually eosinophils. Reiter syndrome is histologically indistinguishable and needs to be differentiated on clinical grounds
Guttate Psoriasis
Clinical
♦
Guttate psoriasis is frequently associated with an antecedent streptococcal pharyngitis
♦
It is characterized by the rapid onset of widespread small scaly plaques
Microscopic (Fig. 19.8)
♦
Characterized by minimal acanthosis, a diminished granular layer, and focal mounds of parakeratosis with neutrophils
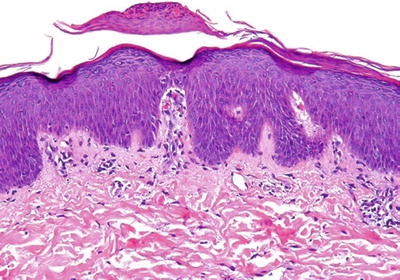
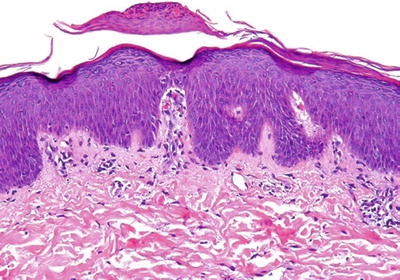
Fig. 19.8.
Guttate psoriasis.
Differential Diagnosis
♦
Includes pityriasis rosea and members of the eczematous dermatitis group of disorders. Pityriasis rosea lacks collections of neutrophils. Eczematous dermatitides have more spongiosis and frequently have some eosinophils as part of the inflammatory infiltrate
Pityriasis Rubra Pilaris
Clinical
♦
Pityriasis rubra pilaris is characterized by hyperkeratotic perifollicular papules with surrounding yellow-orange erythema, islands of uninvolved skin and palmar, and/or plantar keratoderma
Microscopic (Fig. 19.9)
♦
The quintessential features are diffuse hyperkeratosis alternating with parakeratosis both vertically and horizontally in a so-called checkerboard pattern
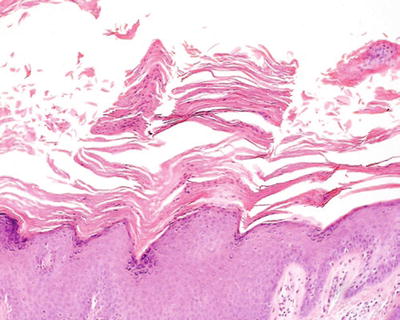
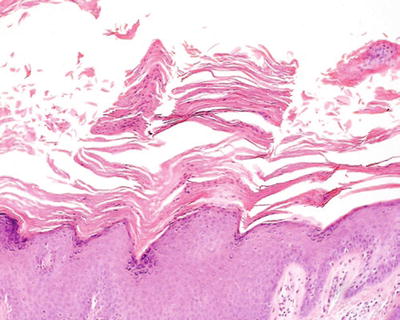
Fig. 19.9.
Pityriasis rubra pilaris demonstrating the checkerboard pattern of parakeratosis.
♦
The epidermis also has acanthosis very similar to psoriasis vulgaris
♦
The granular layer is intact
♦
There is no suprapapillary thinning or collections of neutrophils in the epidermis
♦
In the dermis, there is a mild lymphohistiocytic, superficial perivascular infiltrate
Differential Diagnosis
♦
Psoriasis: Psoriasis has neutrophils in the stratum corneum and a diminished granular layer
♦
Chronic spongiotic dermatitis: Chronic spongiotic dermatitis has less uniform acanthosis and lacks the checkerboard pattern of alternating parakeratosis and hyperkeratosis
♦
Subacute and chronic eczematous dermatitis:
Acanthosis is often a prominent feature in later-stage lesions of spongiotic dermatitis. Therefore, it could be considered to also overlap with the psoriasiform dermatitis pattern (see Spongiotic Dermatitis above)
Lichen Simplex Chronicus/Prurigo Nodularis
Clinical
♦
These two entities are considered a spectrum of the same disease with different clinical presentations
♦
Lichen simplex chronicus presents as pruritic, lichenified, indurated plaques
♦
Prurigo nodularis presents as pruritic nodules
♦
The lesions are related to repetitive rubbing/scratching
♦
Lesions occur only in areas that can be reached and scratched such as the posterior scalp, extremities, and genitalia
♦
Features of lichen simplex chronicus may be seen as a secondary superimposed process on a preexisting dermatitis such as an eczematous dermatitis
Microscopic (Fig. 19.10)
♦
There is prominent compact hyperkeratosis and a thickened granular layer that resembles acral skin


Fig. 19.10.
Prurigo nodule.
♦
The epidermal acanthosis may have a pseudoepitheliomatous pattern, the latter feature being more common in prurigo nodularis
♦
Vertical fibrosis of papillary dermis is a characteristic feature
♦
A mild superficial perivascular lymphocytic infiltrate is present
Differential Diagnosis
♦
Psoriasis: Psoriasis lacks a thickened granular layer and contains neutrophils in the stratum corneum/epidermis
♦
Lichen planus: Lichen planus has hyperkeratosis and a thickened granular layer but has a prominent lichenoid inflammatory infiltrate with interface change
♦
Verruca vulgaris: Verruca vulgaris has papillomatosis, koilocytic cells and dilated blood vessels in the dermis without vertical fibrosis of the papillary dermis
♦
Chronic spongiotic dermatitis: Late-stage chronic spongiotic dermatitis may show similar epidermal features of hyperkeratosis, a thickened granular layer, and acanthosis but usually has a more prominent inflammatory infiltrate and does not have vertical fibrosis of the papillary dermis. Chronic spongiotic dermatitis, however, can have superimposed features of lichen simplex chronicus in long-standing lesions
♦
Squamous cell carcinoma: The pseudoepitheliomatous hyperplasia seen in some cases of prurigo nodularis can be mistaken for a well-differentiated squamous cell carcinoma. The presence of nuclear atypia, atypical mitotic figures, adjacent actinic keratosis/squamous cell carcinoma in situ and true desmoplasia allows differentiation
Secondary Syphilis
Clinical
♦
Lesions of secondary syphilis usually present as nonpruritic macules or papules involving trunk, extremities, palms, and soles
Microscopic
♦
The epidermis shows parakeratosis and psoriasiform hyperplasia
♦
Within the dermis, there is a lichenoid or superficial and deep perivascular lymphocytic infiltrate that usually contains plasma cells
♦
Organisms can be visualized with a Warthin-Starry stain or immunohistochemical stains (the latter is superior)
Differential Diagnosis
♦
Psoriasis: Cutaneous lesions of secondary syphilis lack neutrophils and have significant numbers of plasma cells
♦
Lichen planus: Secondary syphilis can rarely present as a lichenoid variant. Lichen planus typically does not contain plasma cells and has wedge-shaped hypergranulosis and interface change
♦
Chronic spongiotic dermatitis: There can be significant overlap. A deep perivascular component and plasma cells help distinguish secondary syphilis
♦
Pityriasis rosea: Secondary syphilis does not typically have the discrete parakeratotic mounds and has a denser infiltrate with plasma cells
♦
Mycosis fungoides: Mycosis fungoides has collections of atypical cerebriform lymphocytes in the epidermis and haloed lymphocytes. Plasma cells are not typically present in mycosis fungoides
Dermatophytosis
Clinical
♦
Dermatophyte infections classically present as annular scaly plaques with central clearing, usually on the trunk
♦
On the feet, there may be confluent erythema with scale in a moccasin distribution, interdigital maceration, and nail alterations
♦
Lesions that are biopsied frequently do not have classic clinical presentations because they have been altered by topical therapy. The possibility of dermatophyte infection should always be considered in any “rash” that is not responsive to topical corticosteroids
Microscopic (Fig. 19.11)
♦
Neutrophils in stratum corneum
♦
Parakeratosis
♦
Acanthosis
♦
+/− spongiosis
♦
Hyphae in stratum corneum (often only visualized with PAS or GMS stains)
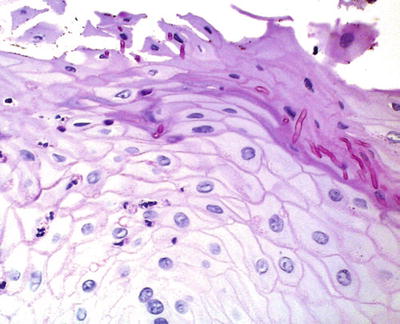
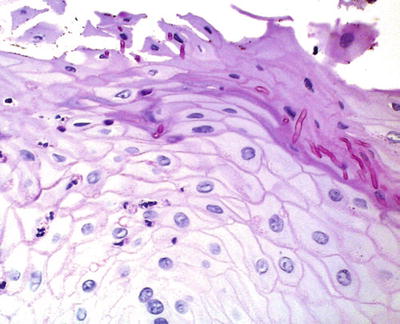
Fig. 19.11.
PAS stain demonstrating fungal hyphae in stratum corneum.
Differential Diagnosis
♦
Psoriasis, spongiotic dermatitis
Interface Dermatitis
♦
Diseases associated with this pattern are characterized by inflammation that is either perivascular or band-like in distribution with epidermal basal vacuolization and dyskeratotic cells
Interface Dermatitis with Associated Perivascular Infiltrate
Erythema Multiforme
Clinical
♦
Erythema multiforme is a self-limiting episodic eruption characterized by erythematous macules, papules, and targetoid lesions
♦
It usually presents on extensor surfaces, palms, soles, and oral mucosa
♦
It can be clinically divided into minor (erythema multiforme) and major (Stevens-Johnson syndrome) forms based on extent of mucosal involvement
♦
It may be associated with HSV and mycoplasma infection and drugs (esp. sulfonamides)
Microscopic (Fig. 19.12)
♦
The epidermis has a normal basket-weave stratum corneum with variable spongiosis
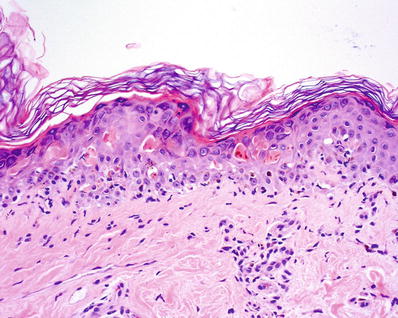
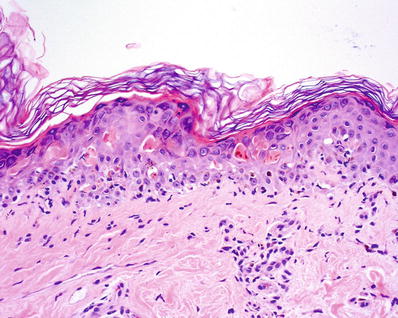
Fig. 19.12.
Erythema multiforme.
♦
Within the epidermis, there are scattered to confluent dyskeratotic cells at all levels of the epidermis
♦
There is interface change characterized by basal vacuolization
♦
Within the dermis, there is a mild superficial perivascular lymphohistiocytic infiltrate with exocytosis of lymphocytes into epidermis. Eosinophils can sometimes be present
♦
In older and severe lesions, epidermal necrosis can be seen
Differential Diagnosis
♦
Morbilliform drug eruption: There is significant histologic overlap, but the degree of epidermal damage is more pronounced in erythema multiforme
♦
Viral exanthem: Similar to drug eruptions, the degree of epidermal damage is more pronounced in erythema multiforme
♦
Dermatomyositis and lupus erythematosus: In these chronic diseases, there is often hyperkeratosis, parakeratosis, and basement membrane thickening, unlike in erythema multiforme. Usually there are more dyskeratotic cells in erythema multiforme. Increased dermal mucin, a feature of both dermatomyositis and lupus erythematosus, is not seen in erythema multiforme
♦
Toxic epidermal necrolysis: The distinction of toxic epidermal necrolysis from erythema multiforme is primarily based on clinical findings, though there is often more prominent epidermal damage, with full thickness necrosis, in toxic epidermal necrolysis
Toxic Epidermal Necrolysis
Clinical
♦
Toxic epidermal necrolysis presents as a widespread tender macular erythematous eruption with vesicles and bullae
♦
The lesions exhibit Nikolsky sign (epithelial detachment with mild pressure)
♦
It is often associated with medications
♦
It has a mortality of 25–50%
Microscopic (Fig. 19.13)
♦
The histologic features are similar to erythema multiforme (see above). Often the degree of epidermal damage is more pronounced than in erythema multiforme
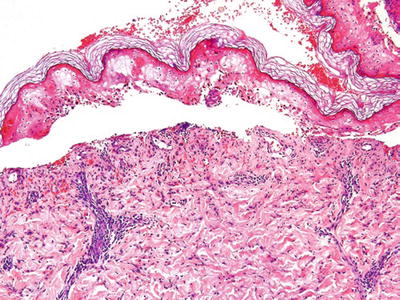
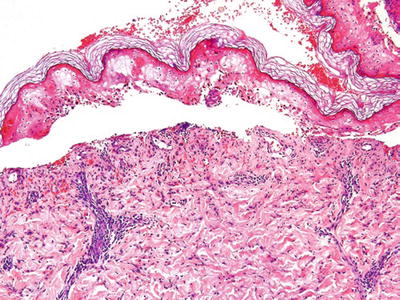
Fig. 19.13.
Toxic epidermal necrolysis.
Differential Diagnosis
♦
Erythema multiforme: As mentioned above, the distinction is primarily clinical
♦
Fixed drug eruption: There is less epidermal damage, a denser inflammatory infiltrate with more eosinophils, and frequently melanophages The clinical presentation as a solitary lesion or limited to a single geographic area is different
♦
Morbilliform drug eruption: There is less epidermal damage and clinically the disorders look different
Lupus Erythematosus
Clinical
♦
Cutaneous lupus erythematosus presents in three different forms:
Chronic (discoid): Well-demarcated scaly plaques, erythematous to hyperpigmented, usually on the head; most patients have disease limited to the skin
Subacute: Scaly erythematous, often annular plaques on upper trunk and extensor surfaces of arms; positive ANA 75% (cytoplasmic Ro and La)
Acute: Associated with systemic lupus erythematosus; erythematous lesions, malar rash; positive ANA and anti-DNA antibodies
♦
There is significant histologic overlap between the different subtypes of lupus erythematosus:
Common features include basal vacuolization, a perivascular and variable periadnexal mononuclear cell infiltrate, and increased dermal mucin
Epidermal changes can also include hyperkeratosis, parakeratosis, atrophy, follicular plugging, basement membrane thickening, and focal dyskeratotic keratinocytes
Differentiating histologic subtypes is often dependent on the clinical presentation (see above), though the discoid subtype is more histologically distinct with a denser and deeper infiltrate and more prominent epidermal changes
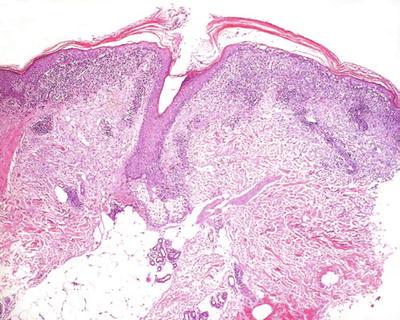
Fig. 19.14.
Lupus erythematosus.
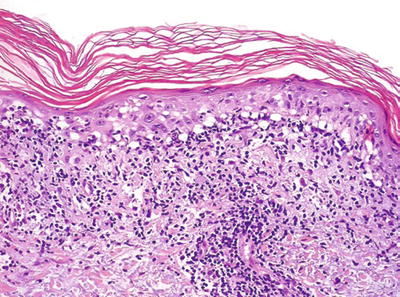
Fig. 19.15.
Prominent interface change in lupus erythematosus.
Differential Diagnosis
♦
Dermatomyositis: Dermatomyositis tends to have a milder infiltrate but otherwise closely resembles lupus erythematosus. Distinction requires clinical information
♦
Erythema multiforme: Erythema multiforme lacks many of the epidermal changes seen in lupus erythematosus (e.g., hyperkeratosis, basement membrane thickening), lacks dermal mucin, and usually has more dyskeratotic keratinocytes
♦
Lichen planus: Lichen planus has characteristic thickening of the granular layer and a dense band-like infiltrate along the dermal-epidermal junction It lacks dermal mucin and a deeper inflammatory component
Dermatomyositis
Clinical
♦
This is classically a systemic disease with muscle weakness, heliotrope periorbital discoloration, violaceous rash on the face and neck, periungual erythema, and Gottron papules on the hands. Not infrequently patients may have cutaneous findings without reported muscle weakness
Microscopic (Fig. 19.16)
♦
There is interface change characterized by basal vacuolization
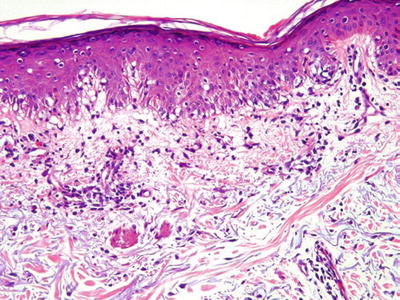
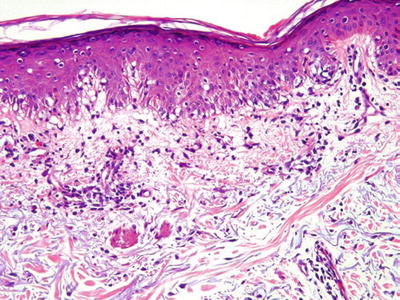
Fig. 19.16.
Dermatomyositis.
♦
There may be hyperkeratosis and/or parakeratosis and focal dyskeratotic keratinocytes
♦
Within the dermis, there is a mild, superficial perivascular mononuclear cell infiltrate and increased dermal mucin
Differential Diagnosis
♦
Lupus erythematosus: In dermatomyositis the infiltrate is milder than in most cases of lupus erythematosus, but knowledge of the clinical presentation is required to confidently distinguish dermatomyositis from lupus erythematosus
♦
Graft versus host disease: The clinical setting is distinctly different. Graft versus host disease lacks dermal mucin
Graft Versus Host Disease
Clinical
♦
Acute: The acute form usually presents 2–4 weeks after bone marrow transplant. Late-onset acute graft versus host disease can occur with donor lymphocyte reinfusion
♦
It presents as macular erythema on the trunk, neck, hands, and feet. Occasionally there may be blisters
♦
Chronic: This form usually presents months to years after bone marrow transplant. There are two forms: lichenoid and sclerodermoid
Lichenoid chronic graft versus host disease: This form presents as violaceous papules and plaques on extremities, palms, and soles; mucosal involvement is frequent
Sclerodermoid chronic graft versus host disease: This form presents as widespread dermal sclerosis
Microscopic
♦
Acute (Fig. 19.17)
Acute graft versus host disease is graded according to the following criteria:
Grade 1: Basal vacuolization, mild superficial perivascular lymphocytic infiltrate
Grade 2: Basal vacuolization with dyskeratotic keratinocytes, exocytosis of lymphocytes, and mild superficial perivascular lymphocytic infiltrate
Grade 3: Same as grade 2 but with cleft formation between dermis and epidermis
Grade 4: Same as grade 3 but with complete separation of epidermis and dermis
♦
Chronic
Lichenoid: The epidermis is hyperkeratotic with a thickened granular layer. There is interface change with basal vacuolization and dyskeratotic keratinocytes. The dermal infiltrate is usually mild with a superficial perivascular to lichenoid pattern
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


