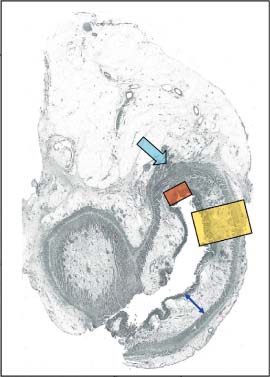
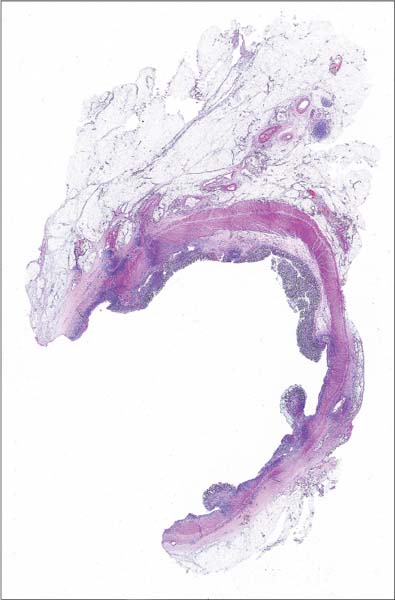
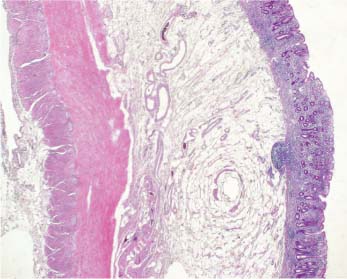
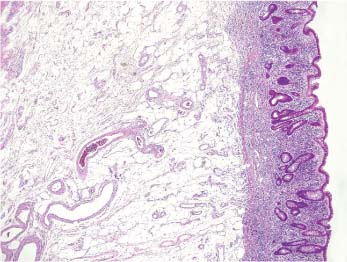
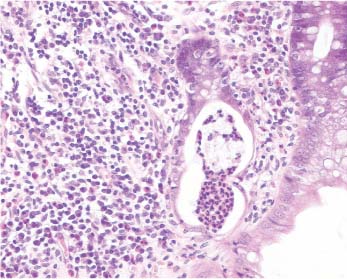
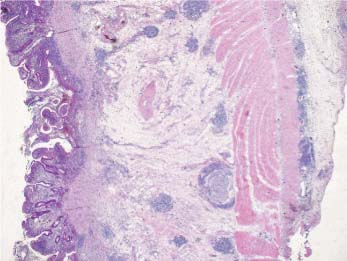
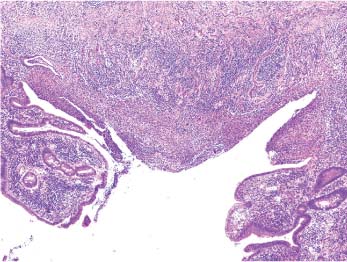
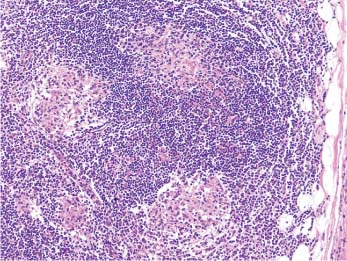
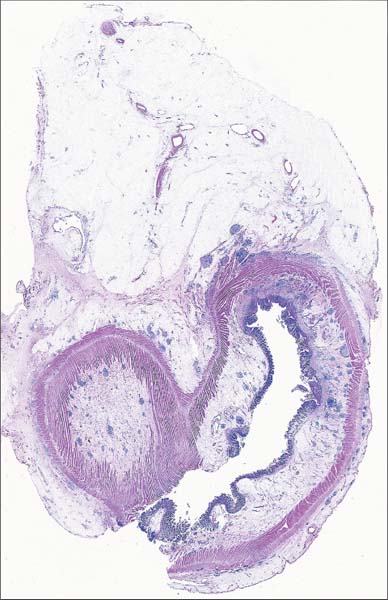
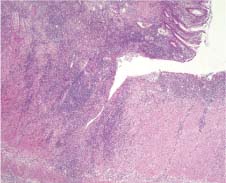
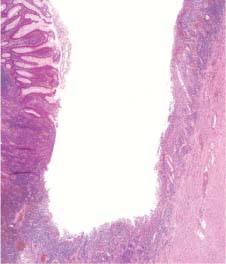
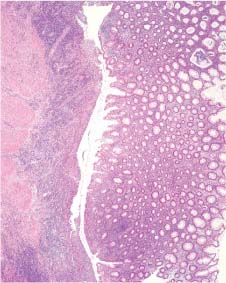
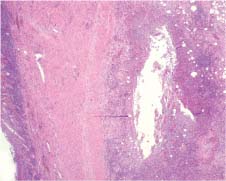
5 Non-neoplastic Lesions Patient data: 66-year-old man with a 15-year history of ulcerative colitis, currently non-responding to therapy. Surgical treatment: Colectomy, after long-term medication for the disease. Specimen: 120-cm-long large intestine together with a 4-cm part of the terminal ileum. Ulcerations in the distal part of the specimen. No polyps or tumors. Histopathologic diagnosis: Active ulcerative colitis. No dysplasia. No malignancy. Follow-up: 16 months, no signs of recurrence of the disease. The large section in Figure 5.1 demonstrates the typical morphological appearance of ulcerative colitis. The main pathological changes in this disease are restricted to the mucosa. The submucosa shows only signs of edema; larger numbers of inflammatory cells are not seen. The lamina muscularis propria is intact. In the schematic image (Fig. 5.1d), the mucosa is indicated with a red arrowhead, the submucosa with a yellow one and the lamina muscularis propria with a green one. Figure 5.1a represents a low-power magnification of the bowel wall, including all the indicated layers, in the area of the yellow rectangle in the schematic image. The magnified detail in Figure 5.1b demonstrates the edematous submucosa, which is free of inflammatory cells. The distortion of the crypts is also well seen. Figure 5.1c is a detail from the mucosa, illustrating intensive active inflammation with a collection of granulocytes in the lumen of a distorted gland (so-called cryptal abscess). Several lymph nodes are also present in the specimen (marked with the green arrows in the schematic image, Fig. 5.1d). Fig. 5.1a Fig. 5.1b Fig. 5.1c Fig. 5.1 Large-section histology image of ulcerative colitis. Fig. 5.1d Schematic guide to the morphologic details in the large section in Fig. 5.1. Patient data: 53-year-old man with a long history of Crohn’s disease, presenting with abdominal pain. Previously operated on for intestinal obstruction caused by Crohn’s disease. Surgical treatment: Ileocecal resection. Specimen: 15-cm-long segment of the large intestine together with an 8-cm part of the terminal ileum and 4-cm appendix. The walls of the terminal ileum and proximal part of the cecum were thickened, the lumen narrowed, and the mucosa partly ulcerated. Histopathologic diagnosis: Crohn’s disease of the terminal ileum and cecum. No signs of malignancy. Follow-up: 1 month, no signs of disease recurrence. Although somewhat tangentially sectioned, the large histologic section in Figure 5.2 reliably demonstrates the hallmark of Crohn’s disease: transmural inflammation leading to thickening of the intestinal wall. Figure 5.2a represents a low-power magnification of the area corresponding to the yellow rectangle in the schematic image (Fig. 5.2d) and illustrates the presence of inflammatory changes in all layers of the intestinal wall. Deep mucosal ulcerations are seen as well as the lymphoid follicles in the submucosa and subserosa. The submucosa is edematous, thickened (as indicated with the blue double-arrow in the schematic image) and contains inflammatory cells. A deep ulceration with incipient fissure formation is demonstrated in Figure 5.2b (corresponding to the area of the red rectangle in Fig. 5.2d). Comparison with the previous large-section image (Case 5.1) clearly shows the differences between ulcerative colitis and Crohn’s disease. As a hallmark of Crohn’s disease, epithelioid granulomas were found in the intestinal wall and in the lymph nodes. A lymph node containing granulomas (indicated with the blue arrow in the schematic image) is microscopically magnified in Figure 5.2c. Fig. 5.2a Fig. 5.2b Fig. 5.2c Fig. 5.2d Schematic guide to the details in the large section in Fig. 5.2. Fig. 5.2 Large-section histology image of Crohn’s disease. Patient data: 46-year-old woman presenting with abdominal pain. Radiologic examination revealed stenosis of the terminal ileum. Surgical treatment: Ileocecal resection, no preoperative treatment. Specimen: 10-cm-long segment of the large intestine together with an 18-cm part of the terminal ileum, with a thickened wall, pseudopolyps, and ulcerations on the mucosal surface. Histopathologic diagnosis: Crohn’s disease in the terminal ileum. Follow-up: 8 months, no signs of disease recurrence. This large histologic section in Figure 5.3 demonstrates another case of Crohn’s disease. Pseudopolyps, wide ulcerations, transmural inflammation, and a pericolic abscess are seen. The pseudopolyps are indicated with yellow arrows in the schematic image (Fig. 5.3e). The blue rectangle in the schematic image indicates a fissure, magnified microscopically in Figure 5.3a. Figure 5.3b illustrates a deep ulceration and part of a pseudopolyp (corresponding to the red-colored area in Fig. 5.3e). An undermining ulceration is present in the blue-colored area in the schematic image and is histologically magnified in Figure 5.3c. The pericolic abscess marked with a yellow rectangle in Figure 5.3s is seen magnified in Figure 5.3d. Compared to the previous case (Case 5.2), the present image illustrates a more advanced stage of Crohn’s disease. Fig. 5.3a Fig. 5.3b Fig. 5.3c Fig. 5.3d
Case 5.1 Ulcerative Colitis
Practical points

Case 5.2 Crohn’s Disease
Practical points
Case 5.3 Crohn’s Disease
Practical points
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree