(1)
Department of Pathology, Radboud University Nijmegen Medical Center, Nijmegen, The Netherlands
Keywords
JawSinonasal CavitiesOsteomaExostosisOsteomyelitis1.1 Introduction
The jaws and sinonasal walls may show reactive bony outgrowths that may cause functional problems. Moreover, inflammatory processes leading to bone loss may be of clinical significance. This Chapter discusses their specific histological features as well as differential diagnostic considerations that allow distinction from genuine neoplasms.
1.2 Exostosis
The jaws may show bony outgrowths at their surface. These exostoses, also called tori occur at the tooth-bearing part, the so-called alveolar process that houses the roots of the teeth in which case they mostly occur at the outer side that lies opposite to the mucosal surface of lip or cheek. Other involved sites are the lingual surface of the mandible or the midline of the palate (Fig. 1.1). Histologically, they are composed of dense lamellar bone that is continuous with the underlying cortical bone of the jaw (Fig. 1.2). However, they are rarely submitted for histological analysis as usually, they can be left untouched unless interfering with dental prosthetic treatment. So they are more important for the dentist than for the surgical pathologist. However, in case of jaw specimens only showing compact lamellar bone on histological examination, one should consider this diagnostic possibility but only in case of corresponding clinical information as there are no histological features that allow distinction between tori and normal compact lamellar bone from the peripheral jaw cortical layer.

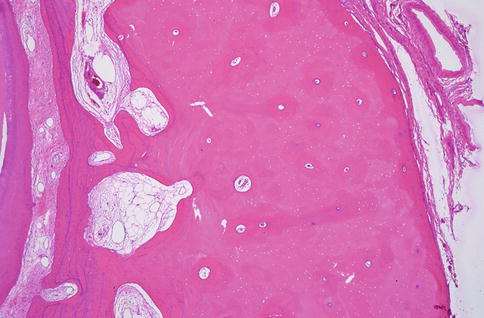

Fig. 1.1
Lingual view of mandible showing torus presenting itself as a bony thickening of the lingual alveolar plate
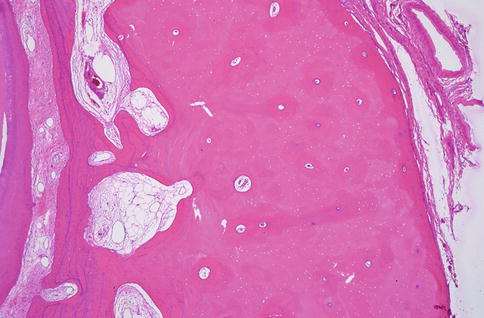
Fig. 1.2
Torus histologically showing thickening of alveolar socket composed of compact lamellar bone
1.3 Osteoma
Osteomas are outgrowths that mainly consist of compact lamellar bone. In the maxillofacial skeleton, they most commonly occur in the frontal and ethmoid sinus; less often, the maxillary antrum and the sphenoid sinus are involved [1]. They may also occur in the jaw bones either sporadic or as manifestation of Gardner’s syndrome [2].
Osteomas usually show a peripheral thick layer of compact lamellar bone that is covered by a thin rim of respiratory mucosa (Fig. 1.3). When moving away from the surface, this compact bone gradually transforms into coarse or slender bone trabeculae within a fatty or fibrous background that merge with the adjacent pre-existent cancellous bone. Sometimes, such a compact peripheral part is absent, the less dense trabecular component lying immediately underneath the covering respiratory mucosa (Fig. 1.4). Occasionally, also thin trabeculae of woven bone lined with prominent osteoblasts are present at the interface of the osteoma and the adjacent cancellous bone (Fig. 1.5).
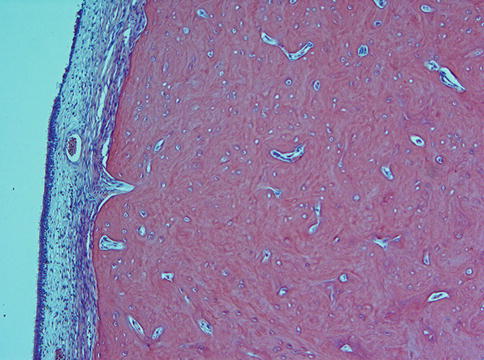
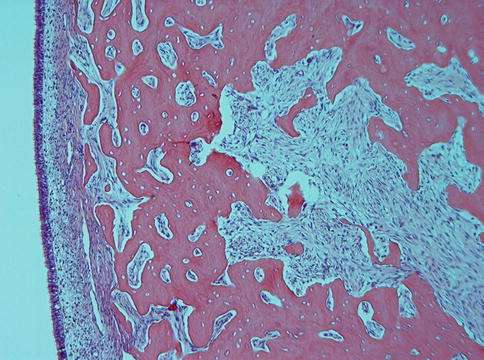
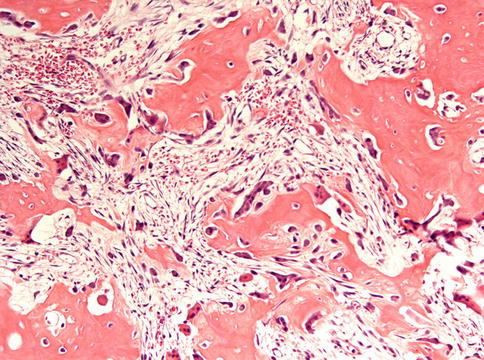
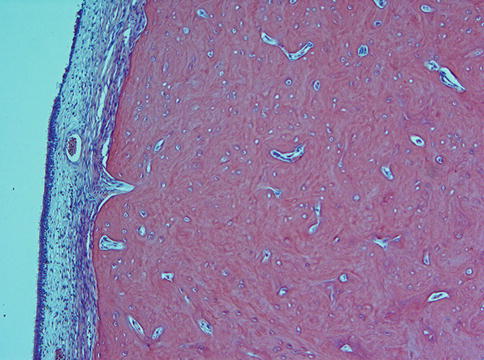
Fig. 1.3
Osteoma covered with thin layer of respiratory mucosa. Peripheral part is compact; central part more trabecular with loose fibrovascular stroma
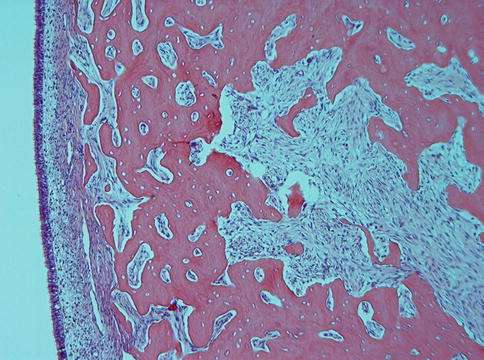
Fig. 1.4
Peripheral part of osteoma composed of slender trabeculae. In this case, the compact peripheral part as usually seen is lacking
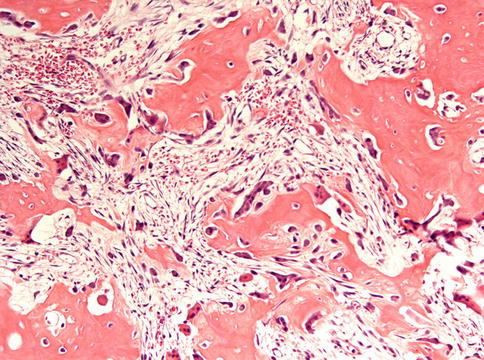
Fig. 1.5
Loose central part of osteoma mimicking osteoblastoma
If located within the jawbone, osteomas pose a differential diagnostic problem as they need to be distinguished from other bone containing lesions of the jaws, such as central ossifying fibroma, osseous dysplasia, osteoblastoma, cementoblastoma, and complex odontoma [3]. Most of these lesions however show a fibrocellular soft tissue component that is different from the fibrofatty soft tissue present in osteomas. Moreover, other hard tissue components than only lamellar bone are found in them. The only real problem may be encountered when dealing with central osteoma and localized chronic sclerosing osteomyelitis if they occur in the mandible as both lesions display a fibrotic marrow and mainly lamellar bone. In those cases, clinical data will be decisive, osteomas usually being an incidental finding on radiographs taken for some other reasons, e.g. during routine dental diagnostics and osteomyelitis causing clinical symptoms.
1.4 Osteomyelitis
Osteomyelitis is characterized by inflammation of the bone marrow accompanied with bone necrosis and sclerosis. The condition mainly involves the mandible, probably due to its compact nature in comparison with the more loosely textured maxilla. Although it may be seen at any age, children are rarely affected.
Osteomyelitis may occur through extension of infection of the dental pulp or as a complication after tooth extraction. After irradiation of the head and neck area as done for head and neck cancer, the subsequent decreased vascularisation of the jaw bone may cause increased vulnerability to infection. An inflammatory reaction in the poorly vascularised bone may develop; a condition known as osteoradionecrosis. Also, bisphosphonates, a class of drugs that prevent the loss of bone mass and therefore are used to treat osteoporosis and related disorders such as Paget’s disease, bone metastasis, multiple myeloma, and other conditions that feature bone fragility, have been associated with the development of necrosis and subsequent infection of the jaw bone [4].
Five different types of osteomyelitis can be discerned: acute suppurative osteomyelitis, chronic suppurative osteomyelitis, chronic focal sclerosing osteomyelitis, chronic diffuse sclerosing osteomyelitis, and proliferative periostitis. Radiographs show an ill-defined mixed radiodense and radiolucent lesion. In case of acute osteomyelitis, pain and fever occur and intraoral examination may reveal sinuses or dead bone sequestered through mucosal defects. In chronic osteomyelitis, slight discomfort may be the sole symptom.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


