Nodular Fasciitis
Elizabeth A. Montgomery, MD
Key Facts
Clinical Issues
Age: 3rd-4th decades
Gender: M = F
Most lesions are benign and do not recur, even if incompletely excised
Simple excision is treatment
Microscopic Pathology
Loose storiform, “feathery” pattern with tissue culture appearance, variable myxoid stroma, cystic spaces, strands of keloid-like collagen
Mitoses present but no atypical forms
Osteoclast-like giant cells found in most lesions if sought
Scattered lymphocytes but essentially no plasma cells
Extravasated erythrocytes unassociated with hemosiderin
3 forms reported: Myxoid, cellular, and fibrous
Loose correlation with duration of lesions; myxoid lesion often resected within 10 days after coming to clinical attention; cellular and fibrous forms resected after longer intervals (patterns variable)
Myofibroblastic differentiation results in expression of some smooth muscle immunohistochemical markers
Lesions can be mistaken for leiomyosarcomas when mitotically active
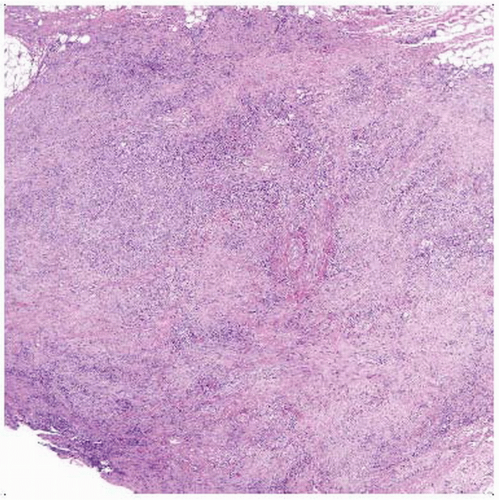 Hematoxylin & eosin shows low magnification of nodular fasciitis. The lesion is nodular and reminiscent of granulation tissue. Note the moderate circumscription. |
TERMINOLOGY
Abbreviations
Nodular fasciitis (NF)
Synonyms
Pseudosarcomatous fasciitis
Subcutaneous pseudosarcomatous fibromatosis
Definitions
Rapidly growing myofibroblastic mass-forming proliferation that is often cellular and mitotically active but behaves in benign fashion
Typically displays loose storiform pattern, cystic spaces, and strands of keloid-like collagen
Intravascular fasciitis is rare variant of nodular fasciitis arising from small or medium-sized vessels
Presents as soft tissue mass with focal intravascular extension or multinodular predominantly intravascular mass
Despite intravascular location, lesion behaves in benign fashion with no tendency to recur or metastasize
Cranial fasciitis involves soft tissues of scalp and underlying skull of infants
Usually erodes bone but may penetrate through bone to involve meninges
Fragments of bone may be seen at periphery of lesion
Birth trauma presumed inciting stimulus
ETIOLOGY/PATHOGENESIS
Unknown
History of local trauma in subset
CLINICAL ISSUES
Epidemiology
Incidence
Uncommon but comparatively common among soft tissue lesions
Age
3rd-4th decades
Gender
M = F
Presentation
Subcutaneous mass
Treatment
Simple excision usually curative
Prognosis
Excellent prognosis
Seldom recurs, even if incompletely excised
MACROSCOPIC FEATURES
General Features
Well-marginated but unencapsulated
Variable mucoid appearance
Sections to Be Submitted
Usually entire lesion is submitted
Size
2-3 cm mass
MICROSCOPIC PATHOLOGY
Histologic Features
Loose storiform, “feathery” pattern with tissue culture appearance, variable myxoid stroma, cystic spaces, strands of keloid-like collagen
Mitoses present but no atypical forms
Osteoclast-like giant cells found in most lesions if sought
Can be highlighted by CD68
Scattered lymphocytes but essentially no plasma cells
Extravasated erythrocytes
No associated hemosiderin
3 forms reported: Myxoid, cellular, and fibrous
Loose correlation with duration of lesions
Myxoid lesion often resected within 10 days after coming to clinical attention
Cellular and fibrous forms resected after longer intervals
Some lesions show several patterns
Myofibroblastic differentiation results in expression of some smooth muscle immunohistochemical markers
Lesions can be mistaken for leiomyosarcomas when mitotically active
Predominant Pattern/Injury Type
Localized
Predominant Cell/Compartment Type
Mesenchymal, spindle
Variant Forms
Nodular myositis
Same as nodular fasciitis but intramuscular
Debate as to whether such cases are instead early myositis ossificans
Intravascular fasciitis
Typically affects head and neck and distal extremities
More solid than classic form
Typically displays abundant osteoclast-like giant cells
Easily mistaken for leiomyosarcoma based on mitoses
Cranial fasciitis
Lesion of infants sometimes attributed to birth trauma
Similar morphology to that of nodular fasciitis but more myxoid background
Some reported examples may be fibromatoses
Can involve skull itself
Subsets occur in specific locations
Spermatic cord (proliferative funiculitis)
Within nerves
ANCILLARY TESTS
Cytology
Shows myofibroblastic cells
Lesions are cellular, which can lead to erroneous impression of sarcoma on aspiration cytology
Frozen Sections





