24 Neurosurgery
Surgical anatomy and physiology
Blood supply
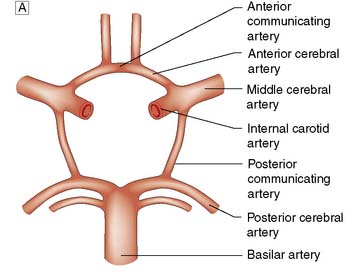
The brain requires a large blood flow (800 ml/min, 16% of cardiac output) to satisfy its oxygen and glucose requirements. The cortex receives about 50 ml/100 g/min, and white matter about 20 ml/100 g/min. Cerebral blood flow (CBF) is largely pressure-autoregulated (i.e. for mean arterial pressures between 60–140 mmHg, CBF remains constant), but is directly related to PaCO2. Other compounds, such as nitric oxide and endothelin, also regulate local CBF. The anterior and posterior circulations of the brain communicate with each other and across the midline through the circle of Willis (Fig. 24.1). In some circumstances, occlusion of a major artery can be compensated for by collateral flow.
Intracranial pressure
The brain is enclosed within a rigid bony container. Intracranial pressure (ICP) therefore depends on the relative volumes of intracranial blood, CSF and brain parenchyma. ICP also fluctuates in response to changes in intrathoracic pressure (e.g. increased by coughing, defaecation) and cardiac pulsation. These transient increases do no harm. In a normal supine adult, ICP is the same as the CSF pressure obtained at lumbar puncture (5–15 cm H2O, 4–10 mmHg). In patients with intracranial mass lesions (tumour, haemorrhage), oedema or CSF obstruction, the extra volume is at first compensated for by a reduction in cerebral blood volume and CSF volume. However, a critical point is soon reached where no further compensation is possible, and any additional volume insult will lead to exponential rises in ICP (Fig. 24.2).
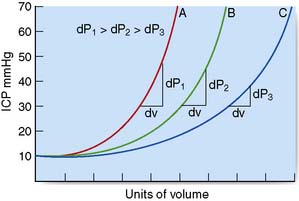
Fig. 24.2 Diagrammatic representation of the effects of a mass lesion on intracranial pressure (ICP).
Generalized or localized increases in ICP may lead to marked displacement of intracranial structures (brain herniation syndromes) and can compromise brain perfusion. The cerebral perfusion pressure (CPP) equals mean arterial pressure (MAP) less the ICP (CPP = MAP – ICP). Progressive rises in ICP lead to increases in MAP and reflex bradycardia. However, if there is a severe and sustained elevation of ICP, autoregulation will be ineffective and cerebral perfusion may be focally or generally compromised, leading to cerebral ischaemia and infarction. A CPP of > 60 mmHg is generally required to sustain adequate cerebral perfusion. Although children and young adults can tolerate lower levels, the consequences of a profound, prolonged lowering of CPP are often devastating (e.g. following severe head injury with raised ICP, or after cardiac arrest). The rate of increase in the volume of intracranial mass is crucial to the shape of the ICP pressure–volume curve (Fig. 24.2). With more chronic, slow-growing lesions such as brain tumours, abscesses or congenital abnormalities, extraordinary degrees of compensation can occur. In some situations, even massive lesions can lead to minimal symptoms and signs, despite brain herniation.
Brain herniation syndromes
Subfalcine (cingulate gyral) herniation
With a parasagittal mass, the ipsilateral cingulate gyrus may herniate beneath the free edge of the falx (Fig. 24.3A). The anterior cerebral artery may be compressed sufficiently to cause medial hemispheric infarction, but otherwise there are no obvious clinical signs except deteriorating conscious level.
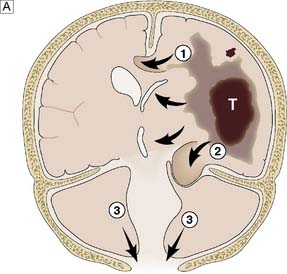
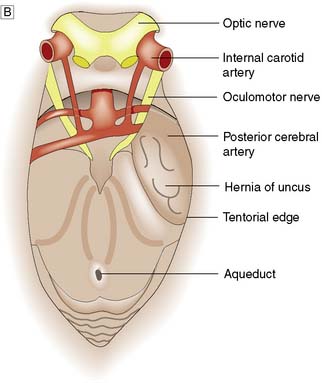
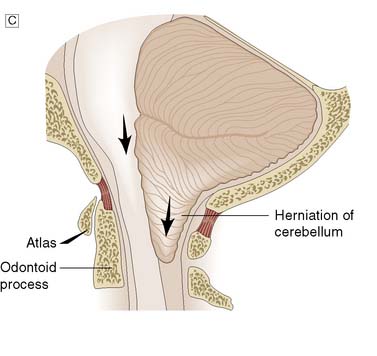
Fig. 24.3 Herniation syndromes.
A Coronal diagram of the dynamics of an intracranial mass lesion. Tumour (T) causes mass effect that compresses the midline and the ventricles (unnumbered arrows), provoking subfalcine or cingulated herniation (arrow 1), and transtentorial herniation (arrow 2). If the mass effect is uncontrolled, tonsillar herniation may also occur (arrows 3). B Transtentorial herniation in the axial plane (plane of dotted line in Fig. 24.3A). C Foraminal herniation.
Transtentorial (uncal) herniation
With large ipsilateral brain lesions, the medial part of the temporal lobe is pushed down through the tentorial notch to become wedged between the tentorial edge and the midbrain (Fig. 24.3B). The opposite cerebral peduncle is pushed against the sharp tentorial edge, and the midbrain and uncus become wedged at the tentorium. The aqueduct is compressed, obstructing CSF flow, and venous obstruction leads to midbrain haemorrhage. The clinical features of an uncal herniation, most often due to a traumatic intracranial haematoma, are:
• The Glasgow Coma Score (GCS) falls (Table 24.1)
• The motor component of the GCS becomes asymmetrical
• The ipsilateral pupil dilates and becomes non-reactive to light
• The respiratory rate falls and the patient become apnoeic.
| Eyes open | 4 |
| 3 | |
| 2 | |
| 1 | |
| Best motor response To verbal command | |
| 6 | |
| To painful stimulus | |
| 5 | |
| 4 | |
| 3 | |
| 2 | |
| 1 | |
| Best verbal response | |
| 5 | |
| 4 | |
| 3 | |
| 2 | |
| 1 | |
| Total number of points (minimum 3, maximum 15) | |
Foraminal (tonsillar) herniation
With mass lesions of the posterior cranial fossa, the cerebellar tonsils and medulla are displaced downwards through the foramen magnum (Fig. 24.3A and C). Cerebellar impaction leads to medullary compression. Following traumatic or spontaneous haematomas, this can lead to a dramatic decrease in the GCS, acute hypertension, bilateral extensor responses and bilateral fixed dilated pupils, followed by sudden respiratory arrest. A similar syndrome may occur following the removal of CSF at lumbar puncture in patients with raised ICP due to a posterior fossa tumour, and is also known as ‘coning’. There is a rapid deterioration in conscious level, with decerebration. Lumbar puncture must not be performed in patients suspected of having raised ICP due to a mass lesion.
Summary Box 24.1 Intracranial pressure
• The rigid bony framework enclosing the central nervous system means that any increase in mass content increases intracranial pressure (ICP)
• Acute increases in ICP lower perfusion pressure and, if unrelieved, lead progressively to decreased Coma Score, herniation syndromes, bradycardia, hypertension, respiratory abnormalities (e.g. apnoea), vasoparalysis and death
• The principal symptoms of chronic raised ICP are headache, vomiting and visual disturbance (blurring of vision). Papilloedema may be apparent
• If ICP is due to a unilateral mass lesion, intracranial structures may be displaced. There are three major forms of herniation: subfalcine, transtentorial and foraminal.
Investigations
Plain X-ray
Summary Box 24.2 Vascular disorders and the central nervous system
• Symptoms due to occlusive vascular disease most often originate from blockage of extracranial vessels by atherosclerosis. Intracranial occlusion can be thrombotic or embolic
• Transient ischaemic attacks are associated with a high risk of major stroke within 5 years unless treatment is instituted (e.g. by carotid endarterectomy or aspirin therapy)
• Intracranial haemorrhage may be extradural, subdural, subarachnoid or intracerebral. Extradural and subdural haemorrhage are usually the result of trauma; subarachnoid bleeding is due to rupture of an aneurysm in around 70% of cases; and intracerebral bleeding is frequently associated with hypertension and amyloid angiopathy
• Patients with subarachnoid haemorrhage from an aneurysm should be considered for either clipping or coiling of the aneurysm to avoid recurrent bleeding.
vascular markings. Calcification of the pineal gland or choroid plexus may allow displacement to be detected, and abnormal calcification can develop in certain cysts and tumours. This investigation has, however, largely been superseded by computed tomography and magnetic resonance imaging.
Cerebrovascular disease
Stroke is a common major clinical disorder in clinical neuroscience practice. Occlusive disease often affects the extracranial vessels and is a common cause of stroke and transient ischaemic attack, usually managed by vascular surgeons (Ch. 25). Most forms of embolic and ischaemic stroke are dealt with by medical neurologists, whereas many large primary intracerebral haemorrhages and, more importantly, subarachnoid haemorrhage (SAH) are dealt with by the neurosurgeon. Brain tissue metabolism is vitally dependent on a consistent delivery of oxygen and glucose substrates for energy. If there is cessation of substrate delivery, the brain tissue will either die (if CBF is below a threshold of 12–15 ml/ 100 g/min) or stop functioning (if CBF is between 15 and 25 ml/100 g/min). These ischaemic thresholds are very important in terms of the extent of stroke (i.e. the amount of tissue that will die) and the penumbra (i.e. tissue that is damaged but still able to recover from these acute events). Urgent thrombolysis in ischaemic stroke is possible if the patient reaches hospital within 4 hours of onset of symptoms and can improve prognosis. Decompressive craniectomy can also save life in selected cases if raised intracranial pressure due to ischaemic brain swelling is a problem.
Subarachnoid haemorrhage
Grading of SAH depends on the coma score of the patient at time of presentation. The most widely used system, and also the easiest to use, is the World Federation of Neurosurgical Societies’ (WFNS) grading, which goes from grade 1 to grade 5 (Table 24.2). When the SAH has produced a syndrome of grade 2–5, it is quite apparent that some neurological catastrophe has occurred. However, when the syndrome is of a grade 1 haemorrhage, differential diagnosis is quite extensive and not infrequently the primary event is overlooked. SAH can mimic atypical migraines, thunderclap headache, coital cephalgia, pituitary apoplexy and meningitic-like syndromes. Sudden death is not uncommon when an aneurysm ruptures into the brain substance rather than the subarachnoid space. The focal signs depend upon the vessel affected. When symptoms and signs are mild, the differential diagnosis is quite extensive and diagnosis depends on having a high index of suspicion.
Table 24.2 World Federation of Neurosurgical Societies (WFNS) grading system for subarachnoid haemorrhage
| WFNS grade | Glasgow Coma Score | Focal neurological deficits |
|---|---|---|
| 1 | 15 | No |
| 2 | 13–14 | No |
| 3 | 13–14 | Yes |
| 4 | 9–12 | – |
| 5 | 3–8 | – |
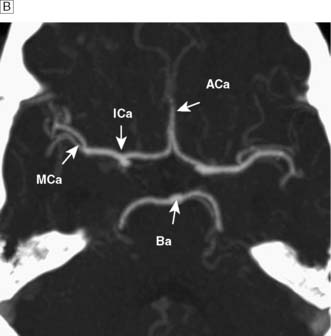
Investigations
The standard investigation is CT, which characteristically shows blood in the CSF basal cisterns in the acute phase (Fig. 24.4). As CSF blood is broken down, the CT detection rate falls after the first 72 hours. If the diagnosis is in doubt, then a lumbar puncture should be performed, but only in patients whose clinical condition is good and in whom CT has excluded an intracranial mass lesion or midline shift. If this is performed early, the CSF will be uniformly blood-stained; later it will contain haem pigments that will be apparent on naked-eye inspection (xanthochromia) or can be detected by spectrophotometry.
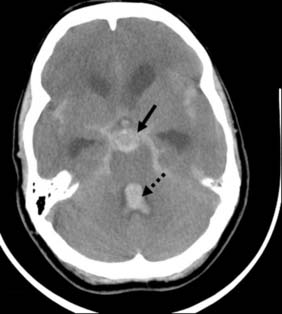
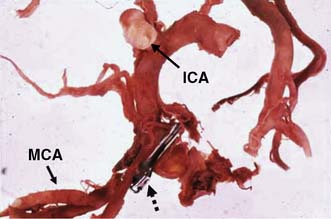
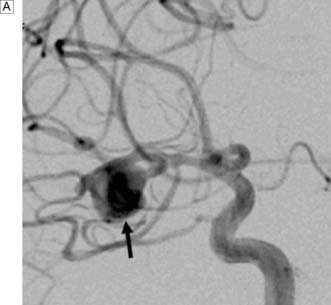
Next, a search must be made for the site of the bleeding. About 80% of aneurysms involve the anterior circulation. Conventionally, carotid or vertebral angiography has been performed (Fig. 24.5). However, CT and MR angiography are equally good at revealing aneurysms greater than 5 mm, and are non-invasive and so associated with less morbidity. As the consequences of missing a diagnosis of SAH are serious, there is a tendency to perform angiography in patients in whom the diagnosis is equivocal. For that reason, a source of bleeding will be identified in only 70% of angiograms. This is usually an aneurysm, less commonly an AVM or a cavernoma. In 30% of cases, no source is found. In the majority, this is a ‘true’ negative, and many of these patients will have a condition called perimesencephalic SAH, which is of unknown aetiology.
Management of aneurysmal SAH
The medical management of SAH includes intravenous fluids; the calcium antagonist, nimodipine (EBM 24.1); analgesia; and antiemetics. Patients in coma will usually be intubated and managed in a neurointensive care unit. Having initially been quite well, many patients begin to exhibit signs of focal or global cerebral ischaemia 4–10 days following an SAH. This has been attributed primarily to vasospasm and can be ameliorated by the prophylactic use of nimodipine; however, clinical deterioration may occur due to hydrocephalus, seizures, metabolic abnormalities and systemic infections.
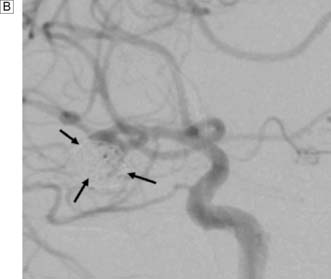
Rebleeding is a major cause of morbidity and mortality following aneurysm rupture. Until recently, standard management was occlusion of the aneurysm from the cerebral circulation by surgically clipping its neck (Fig. 24.6 and EBM 24.2). However, it is now possible to place detachable coils within the aneurysm via a catheter passed from the femoral artery into the cerebral circulation (Fig. 24.7). The coils unwind in the aneurysm and induce thrombosis. Coiling is a much less invasive procedure than open surgery and a recent prospective randomized controlled trial showed that, when an aneurysm can be treated by surgery or coiling, the latter is safer (EBM 24.3). Previously, only a proportion of aneurysms were suitable for coiling. However, improvements in coil, stent and basket technology mean most aneurysms can now be coiled.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree