Neuropathology
EMBRYOLOGY
What structures or cells related to the nervous system are derived from neuroectoderm?
The pineal gland, neurons of the central nervous system, oligodendrocytes, and astrocytes
What structures or cells related to the nervous system are derived from neural crest?
Schwann cells, dorsal root ganglia, autonomic ganglia, and pia mater
From which embryologic tissue type is dura mater derived?
Mesoderm
What structure induces ectoderm to form neuroectoderm?
Notochord
ANATOMY
What are the anatomic components of the central nervous system (CNS)?
The brain and the spinal cord
What are the anatomic components of the peripheral nervous system (PNS)?
Peripheral nerves and nerve roots—divided into sensory and motor divisions. The PNS is composed the somatic and autonomic nervous system; the autonomic nervous system is then further divided into the sympathetic, parasympathetic, and enteric nervous systems.
Name the three layers of meninges:
- Dura mater
- Arachnoid mater
- Pia mater
Together, the arachnoid and pia mater are referred to as leptomeninges.
Between the dura mater and arachnoid mater
Where is the subarachnoid space?
Between the arachnoid mater and pia mater
Where is the choroid plexus?
It is located in all parts of the ventricular system excluding the occipital and frontal horns of the lateral ventricles and cerebral aqueduct.
What is the function of the choroid plexus?
To produce cerebrospinal fluid (CSF) which acts as a mechanical buffer and immunologic barrier for the nervous system
Where is cerebrospinal fluid (CSF) located?
CSF fills spaces in the nervous system including the ventricles, sulci, cisterns, and the central canal of the spinal cord. CSF is then reabsorbed through the arachnoid granulations into the venous system.
Describe the arterial blood supply to the brain:
The internal carotid arteries give rise to the anterior and middle cerebral arteries which form an anastomosis (the Circle of Willis) with the posterior cerebral arteries arising from the vertebral arteries.
Describe the venous drainage of the brain:
Cerebral veins (eg, great cerebral vein, superior ophthalmic vein) drain into venous sinuses (eg, superior sagittal sinus, transverse sinus) located between the meningeal and periosteal layers of the dura mater which drain into the internal jugular veins.
Name two locations in the nervous system which lack a blood-brain barrier:
- Area postrema
- Posterior pituitary
How many spinal nerves do humans have?
31—8 cervical spinal nerves, 12 thoracic spinal nerves, 5 lumbar spinal nerves, 5 sacral spinal nerves, and 1 coccygeal spinal nerve
Name the three major spinal tracts and describe the type of transmitted information:
- Lateral corticospinal tract—voluntary movement (motor) of contralateral limb
- Dorsal column-medial lemniscal pathway—pressure, vibration, light touch sensation, and proprioception
- Spinothalamic tract—pain and temperature sensation
What is the function of the basal ganglia?
Coordination of voluntary movements and posture
Which are the nuclei composing the basal ganglia?
Caudate, putamen, subthalamic, globus pallidus, and substantia nigra
What are the functions of the thalamus?
To relay afferent (ascending) sensory, special sensory, and motor information to the cerebral cortex and to regulate degree of consciousness
What are the functions of the hypothalamus?
Regulation of body temperature, hunger, sexual urges and emotions, circadian rhythms, thirst and water balance, and the autonomic nervous system
Where is the visual cortex?
Occipital lobe
What is the function of the vestibular apparatus?
Spatial orientation
What is the function of the cochlea?
Hearing—the base of the cochlea detects high-frequency sounds while the apex detects low-frequency sounds
HISTOLOGY
What are the major supporting cells of the brain?
Astrocytes
What cells form myelin sheets around axons in the brain?
Oligodendrocytes
What is the predominate cell type found in white matter?
Oligodendrocytes
What cells form myelin sheets around axons in the peripheral nervous system?
Schwann cells
What cells in the brain become phagocytic in response to tissue damage?
Microglia
What are ependymal cells?
Low cuboidal epithelial cells composing the choroid plexus; they may be ciliated which facilitates movement of cerebrospinal fluid.
Which three structures constitute the blood-brain barrier?
- Capillary endothelial cells and tight junctions between the cells
- Basement membrane
- Astrocyte processes
Describe the layers of a peripheral nerve:
The epineurium surrounds an entire nerve. Each fascicle of nerve fibers within a single nerve is surrounded by perineurium. Endoneurium surrounds each single nerve fiber within a fascicle.
What is the function of Meissner corpuscles?
Sensation of light discriminatory touch in skin of palms, soles, and digits
What is the function of Pacinian corpuscles?
Sensation of pressure, coarse touch, vibration, and tension in deep skin, joint capsules, serous membranes, and mesenteries
NEUROPATHOLOGY
General Principles
What is the range of normal values for intracranial pressure (ICP)?
0 to 15 mm Hg
Is the normal range of ICP low or high relative to mean arterial pressure (MAP)?
Low. Increases in ICP (eg, by mass lesions, increased amount of CSF, or bleeding) can quickly cause neurologic compromise.
What are the potential causes of elevated intracranial pressure?
Because the skull is a defined physical space, anything causing increased volume in the confined space will increase pressure, including mass lesions (eg, tumors, blood, abscesses), increased CSF (eg, due to obstructed flow or decreased absorption), or cerebral edema.
What are the main types of cerebral edema?
Vasogenic, cytotoxic, osmotic, and interstitial
Which type of cerebral edema stems from disruption of the blood-brain barrier?
Vasogenic edema—disruption of the blood-brain barrier can result from physical effects of processes such as hypertension or trauma on endothelial cell tight junctions or from release of vasoactive and inflammatory substances by certain tumors.
Where in the brain is vasogenic edema mostly seen?
White matter
What type of edema results from the influx of sodium and water in the neural cells?
Cytotoxic edema—which is due to inadequate function of the sodium-potassium pump in glial cells. The blood-brain barrier remains intact.
Where in the brain is cytotoxic edema most likely to be found?
Gray matter
What is the most common cause of cytotoxic edema?
Hypoxia/ischemia
What is a potential life-threatening complication of increased intracranial pressure?
Increased ICP may result in brain herniation compromising blood flow and/or brain activity, leading to death.
Which cerebral artery can be compressed in a cingulate herniation?
Anterior cerebral artery
What cranial nerve can be compressed in an uncal herniation?
Cranial nerve III
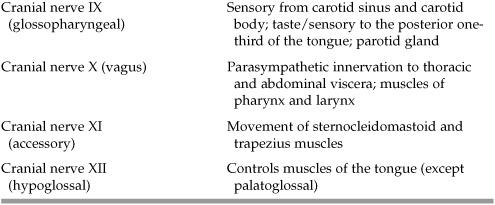
Table 12.1 Types of Herniation
What is tearing of the penetrating vessels of the midbrain and pons called in a tonsillar herniation?
Duret hemorrhages
What surgical intervention can be used to relieve increased intracranial pressure?
Resection or evacuation of a space-occupying lesion or craniotomy to allow the brain additional room to expand
What is hydrocephalus?
A condition in which there is increased fluid within the skull
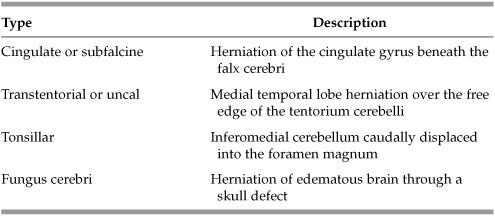
Table 12.2 Types of Hydrocephalus
Congenital
What condition in a newborn is caused by failure of the vertebral arches to close and clinically may present with a tuft of hair at the lower lumber region?
Spina bifida occulta
What is the condition called if in addition to failed closure of the vertebral arches, the meninges are herniated through the defect in the spine?
Meningocele
What is the condition called if in addition to failed closure of the vertebral arches, the spinal cord and meninges are herniated through the defect in the spine?
Meningomyelocele
What clinical findings in a newborn might make a physician suspicious of a congenital viral infection?
Microcephaly, focal cerebral calcification, and an infant whose weight is small for gestational age
What are the common pathogens involved in congenital infections?
Toxoplasma; Other—human immunodeficiency virus (HIV), Varicella, Listeria; Rubella; Cytomegalovirus; Herpes; e; Syphilis (Treponema pallidum)
*TORCHeS
What common manifestations do the TORCHeS infections share?
With any of these infections, patients may present with microcephaly, chorioretinitis, and focal cerebral calcifications.
What is a common household reservoir for toxoplasmosis?
Cat feces
What congenital syndrome is associated with the development of early Alzheimer disease?
Down syndrome
What is microcephaly?
Head circumference smaller than two standard deviations below the mean for age and sex; there are numerous etiologies for microcephaly including infectious and genetic causes and maternal alcohol use.
What is macrocephaly?
Head circumference larger than two standard deviations above the mean for age and sex; there are numerous etiologies for macrocephaly including hydrocephalus and genetic, infectious, and environmental causes.
What is anencephaly?
Absence of a large part of the brain and skull; results when the cephalic end of the neural tube fails to close (around day 23-26 of gestation)
What are the typical clinical findings of Klüver-Bucy syndrome?
Hypersexuality, uninhibited behavior, visual agnosia, and hyperorality
What part of the brain is affected in Klüver-Bucy syndrome?
Bilateral amygdalae
Anatomic
What visual field defect will a patient experience if a lesion involving the right optic nerve is present?
Right anopia (blindness of the right temporal and right nasal visual fields)
What visual field defect will a patient experience if a lesion involving the optic chiasm is present?
Bitemporal hemianopia (blindness of the left temporal and right temporal visual fields)
What visual field defect will a patient experience if a lesion involving the right optic tract is present?
Left homonymous hemianopsia (blindness of the left temporal and right nasal visual fields)
What visual field defect will a patient experience if a lesion involving Meyer loop is present?
Left upper quadrantanopsia
What visual field defect will a patient experience if a lesion involving the dorsal optic radiation is present?
Left lower quadrantanopsia
What are the signs of a complete cranial nerve III lesion?
No pupillary light reflex; dilation of pupil; no accommodation of lens; ptosis of upper eyelid; inability to gaze downward and outward
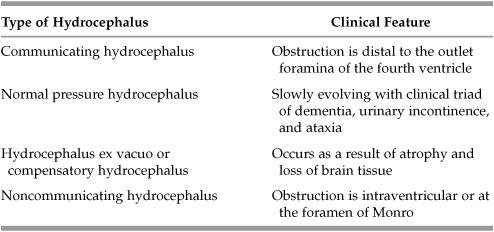
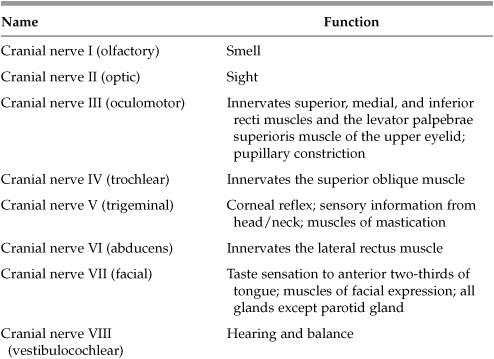
Table 12.3 Cranial Nerves
What other functions does cranial nerve VII have?
Taste to the anterior two-thirds of tongue; sensory to the external ear and muscles of facial expression; parasympathetic to submandibular, sublingual, and lacrimal glands
What nerve is entrapped in carpal tunnel syndrome?
Median nerve
Tingling along the median nerve distribution reproduced by tapping on the palmaris longus tendon at the wrist is known as what sign?
Tinel sign
Tingling along the median nerve distribution reproduced by opposing the dorsal aspects of the hands is known as what sign?
Phalen sign
What is the treatment of carpal tunnel syndrome?
NSAIDs, wrist splints, ergonomics, and carpal tunnel release surgery
Injury to which upper extremity nerve will result in “wrist drop”?
Radial nerve
What clinical findings are associated with Arnold-Chiari malformation?
Due to downward displacement of the cerebellar vermis and medulla, patients may develop headaches which worsen with Valsalva maneuver, syringomyelia, facial pain, muscle weakness, and hearing problems.
What is the diagnostic test of choice to evaluate for possible Arnold-Chiari malformation?
MRI
What is the treatment?
Surgery for symptomatic patients (usually a suboccipital craniectomy)
What is a seizure?
A transient condition of excessive or synchronous neuronal activity in the brain
What is epilepsy?
A disorder in which a patient experiences recurrent seizures (does not include febrile seizures)
What is the difference between a partial and a generalized seizure?
Partial seizures affect only one, localized part of the brain, therefore the clinical symptoms will be specific to the area of affected brain. Generalized seizures affect the brain diffusely, therefore the clinical symptoms will be generalized and nonlocalizing.
What is the difference between a simple and a complex seizure?
Simple and complex seizures are subtypes of partial seizures. A complex partial seizure is one that starts localized (as a simple partial seizure) but then secondarily generalizes thereby impairing consciousness. There is no alteration of consciousness in a simple seizure.
What is status epilepticus?
A condition in which the brain is in a state of persistent seizure
What is the first-line drug therapy for patients in status epilepticus?
Benzodiazepines (diazepam or lorazepam)
Which medication is first-line prophylaxis for status epilepticus?
Phenytoin
For which type of seizure is ethosuximide the recommended first-line drug therapy?
Absence seizures
Which medications may be used as first-line therapy in patients with generalized tonic-clonic seizures?
Phenytoin, carbamazepine, or valproic acid
Which medication may be used in pregnant women and children who have seizures?
Phenobarbital, however, if a pregnant woman has eclampsia, magnesium sulfate is the first-line therapy.
Neoplastic
What are the common presenting features of patients with brain tumors?
Patients may present with a variety of symptoms including nausea, headache, seizures, focal findings (eg, compression of a single cranial nerve), and/or altered mental status/confusion.
What is the most common adult brain tumor?
Metastases (eg, lung, breast, melanoma)
Within the skull, where are adult brain tumors most often located?
Superior to the tentorium—“supratentorial”
Within the skull, where are pediatric brain tumors most often located?
Inferior to the tentorium—”infratentorial”
What is the most common primary brain tumor in adults?
Glioblastoma multiforme (GBM)
What is a “glioma”?
A glioma is a relatively nonspecific term applied to any brain tumor derived from glial cells which include astrocytes, oligodendrocytes, and microglia.
From what cell type does glioblastoma multiforme (GBM) arise?
Astrocytes—GBM is a term applied to a grade IV astrocytoma
How would a GBM appear microscopically?
Tumor cells in GBM are often described as “pseudopalisading” and forming a border around central areas of hemorrhage and necrosis.
What is the classic radiological finding for GBM?
Ring-enhancing lesion with surrounding edema
Why might a GBM be referred to as “butterfly glioma”?
When detected, GBMs may already have crossed the corpus callosum and will be involving both cerebral hemispheres. Radiographically this may appear as the shape of a butterfly.
What is the treatment of GBM?
Surgical removal, radiation, and chemotherapy, but the prognosis remains very poor
What primary brain neoplasm originates from the dura mater or arachnoid?
Meningioma
How would a meningioma appear microscopically?
The tumor is composed of spindled cells arranged in a whorled pattern and may contain “psammoma bodies” which are laminated calcifications.
From what cell type are acoustic neuromas derived?
Schwann cells, although termed acoustic neuroma because they are often localized to cranial nerve VIII
What neurocutaneous syndrome is associated with bilateral acoustic neuromas?
Neurofibromatosis 2
What is the most common location for a tumor developing from oligodendrocytes to arise?
Oligodendrogliomas most often arise in the frontal lobes
What physical examination finding is associated with pituitary adenoma?
Bitemporal hemianopia due to compression of the optic chiasm
Among pituitary adenoma, what is the most common secreted hormone?
Prolactin
What tumor is common in children, located in the cerebellum or third ventricle, and histologically has brightly eosinophilic Rosenthal fibers?
Pilocytic (low-grade) astrocytoma
What is the most common supratentorial brain tumor in children?
Craniopharyngioma—histologically, composed of nests and trabeculae of squamous epithelium, often with abundant keratin resembling a follicular cyst
What physical examination finding is associated with craniopharyngioma?
Bitemporal hemianopia due to compression of the optic chiasm (may be confused clinically with pituitary adenoma)
The clinical findings of retinal angiomas and polycythemia in a child with a brain tumor might make a physician suspicious of which type of pediatric brain tumor?
Hemangioblastoma
What clinical syndrome might the physician want to consider in a patient with retinal angiomas and hemangioblastoma?
von Hippel-Lindau syndrome
Finding cells arranged in a “rosette” pattern on microscopic evaluation of a pediatric cerebellar tumor would suggest the diagnosis of what?
Medulloblastoma
How might medulloblastomas cause increased ICP?
By mass effect of the tumor or by compression of the fourth ventricle and resulting obstructive hydrocephalus
What neurologic findings are associated with tuberous sclerosis?
Clinically, patients may present with seizures, developmental delay, and behavioral problems. Within the CNS, patients develop cortical/subcortical tubers which are believed to be foci of abnormal neural migration, subependymal nodules, and giant cell astrocytomas.
Vascular
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree