17 Neurological disease
Approach to the patient
Imaging plays a key role in diagnosis.
Alterations in consciousness
Table 17.1 Glasgow Coma Score (GCS)
| Category | Response | Score |
|---|---|---|
| Eye opening (E) | Spontaneous | 4 |
| To speech | 3 | |
| To pain | 2 | |
| Nil | 1 | |
| Speech/verbal response (V) | Appropriate and orientated | 5 |
| Confused | 4 | |
| Inappropriate words | 3 | |
| Incomprehensible sounds | 2 | |
| Nil | 1 | |
| Motor response (M) | Obeys commands appropriately | 6 |
| Localizes to pain | 5 | |
| Withdraws to pain | 4 | |
| Flexes to pain | 3 | |
| Extends to pain | 2 | |
| Nil | 1 |
GCS = E + V + M. Minimum score 3, maximum score 15.
Coma is a life-threatening emergency. Assessment must be swift and comprehensive, and occur in tandem with life support measures and initial investigations (Box 17.1, p. 624, and see Fig. 20.21 (p. 722)).
Box 17.1 Management of the comatose patient
This is a neurological emergency (see also Fig. 20.21). Enlist the help of an experienced nurse. The immediate priority is cardiorespiratory resuscitation.
Initial assessment
Investigations where cause of coma is unknown after initial assessment
Acute confusional state (delirium)
Delirium is characterized by abnormalities of perception and cognition, often without a decrease in the level of consciousness. Impairment in consciousness, if present, can vary and fluctuates with confusion, usually being worse at night. It is very common, especially in elderly hospitalized patients. There are a wide variety of causes, often occurring in combination, in a patient vulnerable by virtue of age or impaired cognitive reserve. Common causes include systemic infection, hypoxia, electrolyte imbalance, liver or renal failure, and drug/alcohol intoxication or withdrawal (especially anticonvulsants, anxiolytics, opiates), as well as brain injury, encephalitis/meningitis or deficiency states such as Wernicke–Korsakoff encephalopathy.
Management
Delirium tremens (DTs)
This is the most serious alcohol withdrawal state and occurs 1–3 days after alcohol cessation. Patients have disorientation, agitation, tremor and visual hallucinations. For treatment, see Box 17.2.
Stroke
![]() N.B. Stroke is a medical emergency and prompt treatment can improve prognosis.
N.B. Stroke is a medical emergency and prompt treatment can improve prognosis.
Pathophysiology
Clinical evaluation
• General physical examination
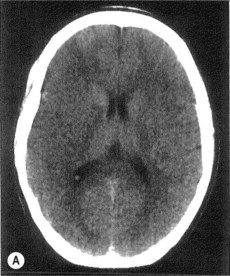
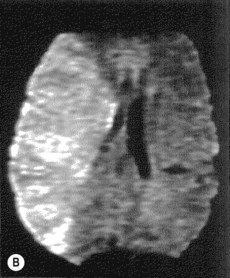
Stroke is primarily a clinical diagnosis, supported by imaging.
Immediate management (see Emergencies in Medicine p. 721)
• Imaging in acute stroke
Thrombolysis (Box 17.3)
Box 17.3
(Amended from Adams HP, et al. 2007)
Thrombolysis in acute ischaemic stroke
Exclusion criteria
Clinical
Further management
• Secondary prevention
• Identification of embolic source
Transient ischaemic attacks (TIAs)
| •Age > 60 years | 1 point |
| •BP > 140 mmHg systolic and/or > 90 mmHg diastolic | 1 point |
| •Clinical features | |
| Unilateral weakness | 2 points |
| Isolated speech disturbance | 1 point |
| Other | 0 points |
| •Duration of symptoms (mins) | |
| > 60 | 2 points |
| 10–59 | 1 point |
| < 10 | 0 points |
| •Diabetes | |
| Present | 1 point |
| Absent | 0 points |