Nephrolithiasis
Shane M. Meehan, MBBCh
Key Facts
Terminology
Concretion of urinary mineral or inorganic crystals in kidney
Etiology/Pathogenesis
Causes
25% known cause
50% idiopathic hypercalciuria
25% unknown cause
Clinical Issues
Frequency: 5% of females and 12% of males in USA
Symptoms include renal colic and hematuria
Stones recur in ~ 50% of instances
Treatment includes hydration, thiazide diuretics, shock wave lithotripsy, and nephrolithotomy
Stone mineral content (stone type) is determined by infrared spectroscopy or x-ray diffraction
Diagnostic Checklist
Stones grow at papillary tip from Randall plaques or from crystal plugs in Bellini ducts
Randall plaque is observed in idiopathic calcium oxalate, calcium phosphate (brushite), mixed oxalate and phosphate (hyperparathyroidism), and cystine lithiasis
Bellini duct dilation and stone protrusion at papillary tip seen in calcium phosphate, uric acid, cystine, and some oxalate (enteric) lithiasis
Cortical scarring may occur as a result of obstruction, infection, lithotripsy, or surgical intervention
TERMINOLOGY
Synonyms
Kidney stone disease, renal stone disease, renal calculi, urolithiasis, lithiasis
Definitions
Concretion of urinary mineral or inorganic crystals in collecting system of kidney
ETIOLOGY/PATHOGENESIS
Stone Types by Mineral Content
Calcium-containing stones (~ 80% of all stones) are composed of the following compounds
Calcium oxalate (30%)
Calcium oxalate and calcium phosphate (35-45%)
Calcium phosphate: Hydroxyapatite (3.75-6%)
Calcium monohydrogen phosphate: Brushite (1.25-2%)
Struvite (magnesium-ammonium phosphate and calcium carbonate-apatite) (5-10%)
Uric acid (5-10%)
Cystine (1-2%)
Miscellaneous: Xanthine, 2,8-dihydroxyadenine, drugs (e.g., indinavir, sulphadiazine, silica-containing antacids), melamine
Predisposing Factors
Calcium stones
Hypercalciuria (defined as > 4 mg Ca/kg/day in urine) without hypercalcemia
Idiopathic
Renal tubular acidosis
Medullary sponge kidney
Cadmium and beryllium nephrotoxicity
Hypercalcemia and hypercalciuria: Primary and secondary hyperparathyroidism
Hyperoxaluria
Primary: Autosomal recessive, types I and II
Secondary: Enteric, due to small intestinal malabsorption or excess intake; dietary, due to poisoning (ethylene glycol)
Struvite stones
Infection by urea-splitting organisms: Proteus, Pseudomonas, Providencia species and others
Alkaline urine increases risk
Uric acid stones
Hyperuricosuria
Associated with uric acid lithiasis and with ~ 40% of calcium oxalate lithiasis
Acidic urine with pH < 5.5
Cystine stones
Hereditary disorders of tubular transport with mutations of solute-linked carriers 3A1 and 7A9 genes
General
Low urine volume
Pathophysiology of Stone Formation
Urine is supersaturated with stone constituents
Nucleation is condensation of dissolved salts to solid phase crystals
Homogeneous nucleation: When solubility limits are exceeded
Heterogeneous nucleation: Cell membranes, cell debris, or other types of crystal form a nidus
Heterogeneous nucleation occurs at lower supersaturation than homogeneous nucleation
Randall plaque
Deposition of calcium phosphate as hydroxyapatite (apatite) in renal papillae
Apatite deposits grow beneath papillary urothelium and around Bellini ducts forming Randall plaque
Randall plaque is thought to be heterogeneous nucleation site for calcium oxalate stone formation
Brushite, hydroxyapatite, and cystine stones can develop from deposits within Bellini ducts
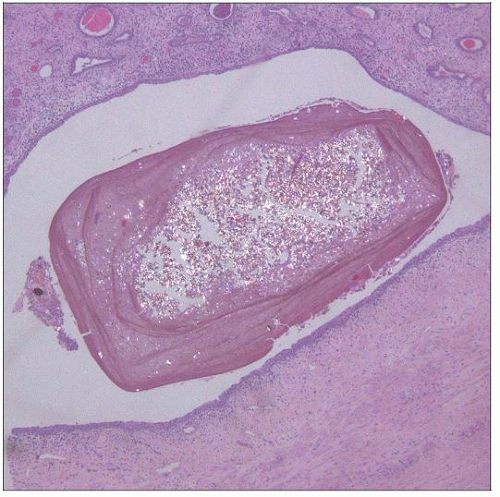
Stone composition: About 95% aggregated crystals and 5% organic mucoprotein matrix
Cut surface of stone has concentrically laminated appearance
Concentric layers are organic matrix skeleton, and crystalline aggregates are in radial arrays
Causes of Nephrolithiasis
25% known causes
Primary hyperparathyroidism and other causes of hypercalcemia
Renal tubular acidosis
Hyperoxaluria
Medullary sponge kidney
Drugs: Antivirals (acyclovir, ganciclovir, indinavir), sulfonamide derivatives, triamterene, glafenine, pyridoxylate
50% idiopathic hypercalciuria
25% unknown cause
CLINICAL ISSUES
Presentation
Frequency: 5% of females and 12% of males in USA
Nonobstructive stones have only hematuria without other symptoms or signs
Renal colic is associated with stone passage, which is dependent on stone size
< 5 mm: High chance of passage
5-7 mm: ~ 50% chance of passage
> 7 mm: Requires intervention for removal
Treatment
Extracorporeal shock wave lithotripsy utilizes ultrasonic waves to break up stones
Endoscopic laser-guided stone disruption
Percutaneous nephrostomy permits removal of larger stones
Medical treatment includes hydration to increase urinary volume and thiazide diuretics to reduce calcium excretion
Prognosis
Stones recur in ~ 50% of instances
Stone formers have higher blood pressure than nonstone formers
Stone formers with high body mass index (> 27) have lower GFR than matched nonstone formers
Almost any stone type can be complicated by urinary obstruction or infection
MACROSCOPIC FEATURES
Morphology of Common Stone Types
Calcium oxalate and apatite
Solitary or multiple; hard, radiopaque; yellow-brown
Struvite
Large and branched (“staghorn”); hard, gray-white, radiopacity dependent on calcium content
Uric acid
Multiple; seldom > 2 cm; hard, smooth surface, yellow-brown; mainly radiolucent
Cystine
Multiple; small, smooth, rounded (rarely “staghorn”); yellow, waxy, radiopaque
80% of stones are unilateral
Stones protrude from Bellini ducts in calcium phosphate, uric acid, cystine, and some cases of enteric oxaluria associated lithiasis
MICROSCOPIC PATHOLOGY
Histologic Features
Mineral deposits
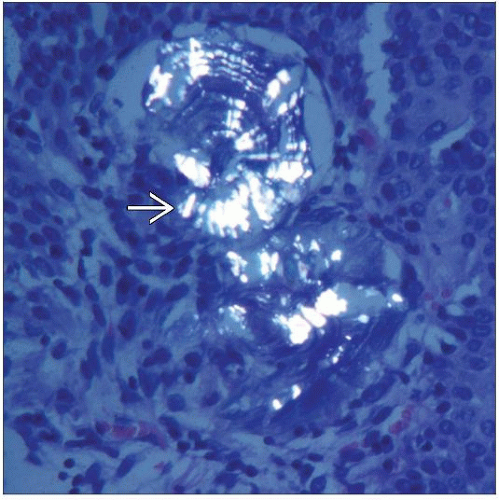
Calcium oxalate forms pale yellow, refractile, sheaves: Birefringent by polarization microscopy
Apatite is basophilic, laminated, and angulate: Confirmed by von Kossa or Yasue staining
Accurate identification of tissue mineral deposits requires infrared spectroscopy
Medullary histology
Papillary suburothelial and periductal apatite deposits correspond to Randall plaque
Apatite deposit in basement membranes of loops of Henle are thought to be earliest lesions of Randall plaque
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree