Chapter 20 Neoplasia
Alkylators
MOA (Mechanism of Action)
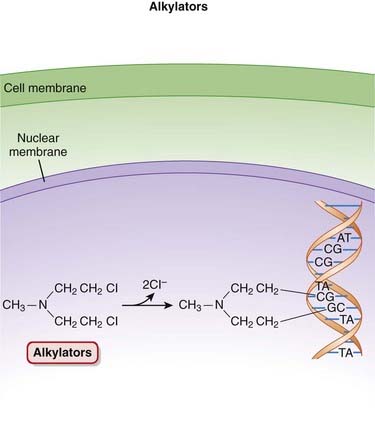
 The alkylating agents transfer alkyl (chemical) groups to DNA. DNA alkylation in the nucleus leads to the death of the cell.
The alkylating agents transfer alkyl (chemical) groups to DNA. DNA alkylation in the nucleus leads to the death of the cell. Once in the cell, the alkylating agents undergo a structural rearrangement that results in the formation of an unstable intermediate, an ethylene immonium ion.
Once in the cell, the alkylating agents undergo a structural rearrangement that results in the formation of an unstable intermediate, an ethylene immonium ion. This ion either directly, or via another intermediate, a carbonium ion, transfers alkyl groups to nucleic acids such as guanine or to other cellular constituents.
This ion either directly, or via another intermediate, a carbonium ion, transfers alkyl groups to nucleic acids such as guanine or to other cellular constituents. Alkylation of guanine or other bases results in abnormal base pairing as well as the excision of these bases, which in turn leads to strand breakage.
Alkylation of guanine or other bases results in abnormal base pairing as well as the excision of these bases, which in turn leads to strand breakage. Alkylating agents are considered to be cell cycle phase nonspecific, with cells in G1 and S phases being most susceptible (Figure 20-1).
Alkylating agents are considered to be cell cycle phase nonspecific, with cells in G1 and S phases being most susceptible (Figure 20-1). The connection between DNA alkylation and death of the cancer cell has not been established; however, one of the likely mechanisms is damage to DNA that is sufficient to activate proapoptotic proteins such as p53, leading to cell death.
The connection between DNA alkylation and death of the cancer cell has not been established; however, one of the likely mechanisms is damage to DNA that is sufficient to activate proapoptotic proteins such as p53, leading to cell death. Nitrosoureas have an additional mechanism of action. Nitrosoureas undergo another reaction, referred to as carbamoylation, with lysine residues of proteins. Carbamoylation is the transfer of carbamoyl (NH2CO) groups to an amino group, such as that found in amino acids.
Nitrosoureas have an additional mechanism of action. Nitrosoureas undergo another reaction, referred to as carbamoylation, with lysine residues of proteins. Carbamoylation is the transfer of carbamoyl (NH2CO) groups to an amino group, such as that found in amino acids. The product of this reaction is referred to as a carbamoylated protein, and this process appears to limit the ability of the cancer cell to repair DNA. This unique mechanism of action limits cross-resistance between nitrosoureas and other members of this class.
The product of this reaction is referred to as a carbamoylated protein, and this process appears to limit the ability of the cancer cell to repair DNA. This unique mechanism of action limits cross-resistance between nitrosoureas and other members of this class.Pharmacokinetics
 Oral dosage forms are available for cyclophosphamide, melphalan, chlorambucil, and busulfan. Lomustine is available only in oral dosage forms. The rest are all intravenous.
Oral dosage forms are available for cyclophosphamide, melphalan, chlorambucil, and busulfan. Lomustine is available only in oral dosage forms. The rest are all intravenous. Nitrosoureas are highly lipid soluble and readily cross the blood-brain barrier; therefore they are useful in the treatment of brain tumors.
Nitrosoureas are highly lipid soluble and readily cross the blood-brain barrier; therefore they are useful in the treatment of brain tumors.Side Effects
 Nausea, vomiting: These are common side effects with cytotoxic agents, which tend to target rapidly dividing cells, including those of the GI tract.
Nausea, vomiting: These are common side effects with cytotoxic agents, which tend to target rapidly dividing cells, including those of the GI tract. Alopecia: Cytotoxic chemotherapy agents tend to target tissues with rapidly dividing cells, such as those in hair follicles. This effect is seen most often with cyclophosphamide.
Alopecia: Cytotoxic chemotherapy agents tend to target tissues with rapidly dividing cells, such as those in hair follicles. This effect is seen most often with cyclophosphamide.Serious
 Myelosuppression: Typical of cytotoxic agents, alkylators tend to target cells that are actively dividing, such as those found in the bone marrow.
Myelosuppression: Typical of cytotoxic agents, alkylators tend to target cells that are actively dividing, such as those found in the bone marrow. Hemorrhagic cystitis (cyclophosphamide and ifosfamide) is caused by acrolein, a metabolite of cyclophosphamide and ifosfamide. This effect can be managed by increasing fluid intake and by administering sulfhydryl donors such as N-acetylcysteine or mesna (an antioxidant). These agents bind with acrolein and form a nontoxic compound.
Hemorrhagic cystitis (cyclophosphamide and ifosfamide) is caused by acrolein, a metabolite of cyclophosphamide and ifosfamide. This effect can be managed by increasing fluid intake and by administering sulfhydryl donors such as N-acetylcysteine or mesna (an antioxidant). These agents bind with acrolein and form a nontoxic compound.Important Notes
 A number of the alkylating agents (cyclophosphamide, ifosfamide, estramustine, melphalan, and chlorambucil) are also known as nitrogen mustards. These agents are related to mustard gas, a biologic warfare agent used during World War I.
A number of the alkylating agents (cyclophosphamide, ifosfamide, estramustine, melphalan, and chlorambucil) are also known as nitrogen mustards. These agents are related to mustard gas, a biologic warfare agent used during World War I. Cyclophosphamide has a significant effect on lymphocytes; therefore it is also used as an immunosuppressant to prevent rejection of transplanted organs, as well as in conditions such as rheumatoid arthritis and nephrotic syndrome. Cyclophosphamide has a steroid-sparing effect, meaning that it can reduce the need for use of corticosteroids.
Cyclophosphamide has a significant effect on lymphocytes; therefore it is also used as an immunosuppressant to prevent rejection of transplanted organs, as well as in conditions such as rheumatoid arthritis and nephrotic syndrome. Cyclophosphamide has a steroid-sparing effect, meaning that it can reduce the need for use of corticosteroids. Estramustine is a combination of estrogen and a mustine called chlormethine. Accordingly, it has both cytotoxic and hormonal actions and is used primarily in prostate cancer.
Estramustine is a combination of estrogen and a mustine called chlormethine. Accordingly, it has both cytotoxic and hormonal actions and is used primarily in prostate cancer. Patients with defective DNA repair mechanisms (ataxia-telangiectasia, Fanconi’s anemia, Bloom’s syndrome, and xeroderma pigmentosa) are more sensitive to DNA-damaging agents.
Patients with defective DNA repair mechanisms (ataxia-telangiectasia, Fanconi’s anemia, Bloom’s syndrome, and xeroderma pigmentosa) are more sensitive to DNA-damaging agents.FYI
 The first rationally designed anticancer agent was a nitrosourea (methyl nitrosourea), developed in 1898.
The first rationally designed anticancer agent was a nitrosourea (methyl nitrosourea), developed in 1898. The U.S. Army played a role in the development of nitrogen mustards, deriving the prototype to this class (mechlorethamine) from the mustard gases used in the first World War. After an accidental exposure, it was discovered that nitrogen mustard produced lymphopenia, inspiring its use in malignant proliferative disorders.
The U.S. Army played a role in the development of nitrogen mustards, deriving the prototype to this class (mechlorethamine) from the mustard gases used in the first World War. After an accidental exposure, it was discovered that nitrogen mustard produced lymphopenia, inspiring its use in malignant proliferative disorders.Anthracyclines
MOA (Mechanism of Action)
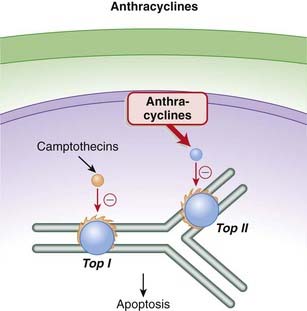
 Topoisomerase II (Top II) plays a key role during DNA synthesis, nicking and resealing the DNA helix so that it does not become tangled during replication.
Topoisomerase II (Top II) plays a key role during DNA synthesis, nicking and resealing the DNA helix so that it does not become tangled during replication. The anthracyclines prevent the resealing step from occurring by intercalating into and inhibiting the DNA–topoisomerase II complex after the nicking phase. This results in a large number of DNA fragments, eventually prompting the cancer cell to undergo apoptosis (Figure 20-2).
The anthracyclines prevent the resealing step from occurring by intercalating into and inhibiting the DNA–topoisomerase II complex after the nicking phase. This results in a large number of DNA fragments, eventually prompting the cancer cell to undergo apoptosis (Figure 20-2). As a secondary mechanism, anthracyclines produce free radicals, and these free radicals in turn damage cell membranes, proteins, and lipids. The generation of free radicals is also believed to mediate an important toxicity associated with this class (see Side Effects).
As a secondary mechanism, anthracyclines produce free radicals, and these free radicals in turn damage cell membranes, proteins, and lipids. The generation of free radicals is also believed to mediate an important toxicity associated with this class (see Side Effects). In addition anthracyclines are DNA intercalators, meaning that they insert themselves into DNA structure, inhibiting transcription and replication.
In addition anthracyclines are DNA intercalators, meaning that they insert themselves into DNA structure, inhibiting transcription and replication.Pharmacokinetics
 Doxorubicin was the first anthracycline to be encapsulated in liposomes to facilitate targeted delivery of the drug and therefore avoid cardiotoxicity (see Side Effects). One of the key mechanisms for this targeted delivery relies on the fact that the liposomes readily extravasate in tissues that have a disrupted vasculature, such as that found in tumors. Blood vessels in tumors tend to be “leaky” owing to the constant angiogenesis that is taking place. Conversely, the liposomes have difficulty exiting vessels in tissues such as the myocardium.
Doxorubicin was the first anthracycline to be encapsulated in liposomes to facilitate targeted delivery of the drug and therefore avoid cardiotoxicity (see Side Effects). One of the key mechanisms for this targeted delivery relies on the fact that the liposomes readily extravasate in tissues that have a disrupted vasculature, such as that found in tumors. Blood vessels in tumors tend to be “leaky” owing to the constant angiogenesis that is taking place. Conversely, the liposomes have difficulty exiting vessels in tissues such as the myocardium. The anthracyclines are eliminated through hepatic metabolism, through a variety of routes. Because of the toxicities associated with these agents, dose adjustments should be considered in patients with significant hepatic impairment.
The anthracyclines are eliminated through hepatic metabolism, through a variety of routes. Because of the toxicities associated with these agents, dose adjustments should be considered in patients with significant hepatic impairment.Contraindications
 Severe cardiac disease: Anthracyclines should be used only with extreme caution and after a careful risk-benefit assessment in these patients. See Side Effects.
Severe cardiac disease: Anthracyclines should be used only with extreme caution and after a careful risk-benefit assessment in these patients. See Side Effects.Side Effects
 Nausea and vomiting are common side effect with cytotoxic agents, which tend to target rapidly dividing cells, including those of the GI tract.
Nausea and vomiting are common side effect with cytotoxic agents, which tend to target rapidly dividing cells, including those of the GI tract. Alopecia: Cytotoxic chemotherapy agents tend to target tissues with rapidly dividing cells, such as those in hair follicles. The hair loss is reversible.
Alopecia: Cytotoxic chemotherapy agents tend to target tissues with rapidly dividing cells, such as those in hair follicles. The hair loss is reversible. Mucositis or stomatitis is an inflammatory condition of the mouth. Cytotoxic chemotherapy agents tend to target tissues with rapidly dividing cells, such as those in the oral mucosa.
Mucositis or stomatitis is an inflammatory condition of the mouth. Cytotoxic chemotherapy agents tend to target tissues with rapidly dividing cells, such as those in the oral mucosa. Soft tissue necrosis: If the anthracyclines become extravascular, they can damage surrounding tissue. Infusions should be carried out slowly to reduce the risk of extravasation.
Soft tissue necrosis: If the anthracyclines become extravascular, they can damage surrounding tissue. Infusions should be carried out slowly to reduce the risk of extravasation.Serious
 Cardiotoxicity: The free radicals generated by the anthracyclines cause peroxidation of the cardiac sarcoplasmic reticulum, leading to a Ca2+-dependent cardiac necrosis. The reason this toxicity is selective for cardiac tissue is that catalase, able to neutralize these free radicals, is not found in cardiac tissue.
Cardiotoxicity: The free radicals generated by the anthracyclines cause peroxidation of the cardiac sarcoplasmic reticulum, leading to a Ca2+-dependent cardiac necrosis. The reason this toxicity is selective for cardiac tissue is that catalase, able to neutralize these free radicals, is not found in cardiac tissue.Important Notes
 Cardiotoxicity associated with anthracyclines can occur both acutely and chronically. Acute toxicity is characterized by abnormal electrocardiograms (ECGs) and reductions in systolic function. Chronic toxicity is cumulative and dose related. It manifests as congestive heart failure, and once it has reached this point it has a very high mortality rate. This chronic cardiotoxicity is of greater concern, and it is addressed using a number of strategies, including limitations on doses used, as well as use of liposomal formulations and adjuvant agents, as described later.
Cardiotoxicity associated with anthracyclines can occur both acutely and chronically. Acute toxicity is characterized by abnormal electrocardiograms (ECGs) and reductions in systolic function. Chronic toxicity is cumulative and dose related. It manifests as congestive heart failure, and once it has reached this point it has a very high mortality rate. This chronic cardiotoxicity is of greater concern, and it is addressed using a number of strategies, including limitations on doses used, as well as use of liposomal formulations and adjuvant agents, as described later. Mitoxantrone has a chemical structure that is distinct from that of the anthracyclines, and it is believed to be less cardiotoxic than the anthracyclines. It does not generate free radicals.
Mitoxantrone has a chemical structure that is distinct from that of the anthracyclines, and it is believed to be less cardiotoxic than the anthracyclines. It does not generate free radicals.Advanced
 Strategies to minimize cardiotoxicity include the use of a cardioprotective drug such as dexrazoxane. The generation of free radicals by anthracyclines is iron dependent. Dexrazoxane chelates iron that is bound in anthracycline complexes, and this prevents the formation of the free radicals that damage the myocardium. Dexrazoxane does not appear to impair the antitumor activity of the anthracyclines.
Strategies to minimize cardiotoxicity include the use of a cardioprotective drug such as dexrazoxane. The generation of free radicals by anthracyclines is iron dependent. Dexrazoxane chelates iron that is bound in anthracycline complexes, and this prevents the formation of the free radicals that damage the myocardium. Dexrazoxane does not appear to impair the antitumor activity of the anthracyclines.Drug Interactions
 It appears that the cardiotoxic effects of anthracyclines may be worsened by concurrent administration of trastuzumab. Trastuzumab is a monoclonal antibody that is used in the treatment of breast cancers expressing the HER2/neu receptor. A number of anthracyclines are used in treating breast cancer.
It appears that the cardiotoxic effects of anthracyclines may be worsened by concurrent administration of trastuzumab. Trastuzumab is a monoclonal antibody that is used in the treatment of breast cancers expressing the HER2/neu receptor. A number of anthracyclines are used in treating breast cancer.Antimetabolites
MOA (Mechanism of Action)
Folate Analogues
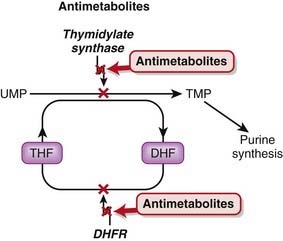
 Tetrahydrofolate (THF) is an essential cofactor in the transformation of 2’-deoxyuridylate (dUMP) to 2’-deoxythymidylate (dTMP). This is a required step in the synthesis of purines and thus DNA.
Tetrahydrofolate (THF) is an essential cofactor in the transformation of 2’-deoxyuridylate (dUMP) to 2’-deoxythymidylate (dTMP). This is a required step in the synthesis of purines and thus DNA. THF is synthesized by the actions of dihydrofolate reductase (DHFR). Methotrexate has a high affinity for DHFR and competitively inhibits DHFR (Figure 20-3).
THF is synthesized by the actions of dihydrofolate reductase (DHFR). Methotrexate has a high affinity for DHFR and competitively inhibits DHFR (Figure 20-3).Pyrimidine Analogues
 Fluorouracil is a uracil analogue. It is converted to FdUMP (fluorodeoxyuridine monophosphate) and although it interacts with thymidylate synthetase, it cannot be converted to dTMP because of the fluoro component and therefore results in a deficiency of dTMP. Without dTMP, DNA synthesis cannot occur. It is considered to be a fraudulent nucleotide.
Fluorouracil is a uracil analogue. It is converted to FdUMP (fluorodeoxyuridine monophosphate) and although it interacts with thymidylate synthetase, it cannot be converted to dTMP because of the fluoro component and therefore results in a deficiency of dTMP. Without dTMP, DNA synthesis cannot occur. It is considered to be a fraudulent nucleotide. Inhibitors of other enzymes important in dTMP synthesis include raltitrexed (thymidylate synthetase inhibitor) and pemetrexed (thymidylate transferase inhibitor).
Inhibitors of other enzymes important in dTMP synthesis include raltitrexed (thymidylate synthetase inhibitor) and pemetrexed (thymidylate transferase inhibitor). Cytarabine, also known as cytosine arabinoside, is an analogue of 2’-deoxycytidine (essentially, cytosine). On entering the cell, it is converted to cytosine arabinoside triphosphate by the same phosphorylation reaction that 2’-deoxycytidine undergoes. The cytosine arabinoside triphosphate competitively inhibits DNA polymerase, inhibiting both DNA synthesis and repair.
Cytarabine, also known as cytosine arabinoside, is an analogue of 2’-deoxycytidine (essentially, cytosine). On entering the cell, it is converted to cytosine arabinoside triphosphate by the same phosphorylation reaction that 2’-deoxycytidine undergoes. The cytosine arabinoside triphosphate competitively inhibits DNA polymerase, inhibiting both DNA synthesis and repair.Purine Analogues
 Fludarabine inhibits DNA polymerases, leading to inhibition of DNA synthesis and repair. It also incorporates into DNA and may also promote apoptosis by an undetermined mechanism.
Fludarabine inhibits DNA polymerases, leading to inhibition of DNA synthesis and repair. It also incorporates into DNA and may also promote apoptosis by an undetermined mechanism. Pentostatin inhibits adenosine deaminase, an enzyme that transforms adenosine to inosine. This leads to accumulation of intracellular adenosine and deoxyadenosine, which can block DNA synthesis by inhibiting ribonucleotide reductase. Ribonucleotide reductase catalyzes the formation of deoxyribonucleotides from ribonucleotides. Deoxyribonucleotides are used in the synthesis of DNA.
Pentostatin inhibits adenosine deaminase, an enzyme that transforms adenosine to inosine. This leads to accumulation of intracellular adenosine and deoxyadenosine, which can block DNA synthesis by inhibiting ribonucleotide reductase. Ribonucleotide reductase catalyzes the formation of deoxyribonucleotides from ribonucleotides. Deoxyribonucleotides are used in the synthesis of DNA.Pharmacokinetics
 Methotrexate can be administered orally, intravenously, intramuscularly, or intrathecally. It is not able to cross the blood-brain barrier, so entry into the central nervous system (CNS) can be achieved only by intrathecal administration.
Methotrexate can be administered orally, intravenously, intramuscularly, or intrathecally. It is not able to cross the blood-brain barrier, so entry into the central nervous system (CNS) can be achieved only by intrathecal administration. Only a small fraction of methotrexate is metabolized; most of it is eliminated unchanged in the urine. Because of its potential for nephrotoxicity, dose adjustments must be considered in patients with renal impairment.
Only a small fraction of methotrexate is metabolized; most of it is eliminated unchanged in the urine. Because of its potential for nephrotoxicity, dose adjustments must be considered in patients with renal impairment. The purine analogues mercaptopurine and thioguanine are available in oral dosage forms. They are metabolized by the liver. One of the enzymes responsible for mercaptopurine metabolism is xanthine oxidase; therefore inhibitors of this enzyme, such as allopurinol, can lead to toxicity. The elimination half-life of mercaptopurine is relatively short (<1 hour).
The purine analogues mercaptopurine and thioguanine are available in oral dosage forms. They are metabolized by the liver. One of the enzymes responsible for mercaptopurine metabolism is xanthine oxidase; therefore inhibitors of this enzyme, such as allopurinol, can lead to toxicity. The elimination half-life of mercaptopurine is relatively short (<1 hour). Fludarabine and cladribine can be administered intravenously or orally, and pentostatin is administered intravenously. All are primarily eliminated by renal excretion. Dose adjustments should be considered in patients with renal impairment.
Fludarabine and cladribine can be administered intravenously or orally, and pentostatin is administered intravenously. All are primarily eliminated by renal excretion. Dose adjustments should be considered in patients with renal impairment. Cytarabine is administered intravenously or subcutaneously, and 5-fluorouracil is administered intravenously or topically. Cytarabine (cytarabine triphosphate) and 5-fluorouracil (5-fluorodeoxyuridine monophosphate and triphosphate) are converted to active metabolites in the body. Both are largely metabolized by the liver, and dose adjustments should be considered in patients with hepatic impairment.
Cytarabine is administered intravenously or subcutaneously, and 5-fluorouracil is administered intravenously or topically. Cytarabine (cytarabine triphosphate) and 5-fluorouracil (5-fluorodeoxyuridine monophosphate and triphosphate) are converted to active metabolites in the body. Both are largely metabolized by the liver, and dose adjustments should be considered in patients with hepatic impairment.Side Effects
Folate Analogues
 Myelosuppression: Conventional chemotherapy agents work by targeting rapidly dividing cells. This nonspecific effect can also target rapidly dividing cells in other areas of the body, including bone marrow and the GI tract.
Myelosuppression: Conventional chemotherapy agents work by targeting rapidly dividing cells. This nonspecific effect can also target rapidly dividing cells in other areas of the body, including bone marrow and the GI tract. Alopecia: Cytotoxic chemotherapy agents tend to target tissues with rapidly dividing cells, such as those in hair follicles.
Alopecia: Cytotoxic chemotherapy agents tend to target tissues with rapidly dividing cells, such as those in hair follicles.Purine Analogues
 Myelosuppression develops more gradually than with the folate analogues. It tends to be worse with thioguanine.
Myelosuppression develops more gradually than with the folate analogues. It tends to be worse with thioguanine.Important Notes
 High-dose regimens of methotrexate may require rescue with folinic acid, also known as leucovorin. Folinic acid is a reduced form of folic acid. Methotrexate is an “antifolate” drug, and patients who are taking high doses or receiving chronic therapy are likely to experience severe symptoms of folate deficiency unless they are treated adjunctively with leucovorin.
High-dose regimens of methotrexate may require rescue with folinic acid, also known as leucovorin. Folinic acid is a reduced form of folic acid. Methotrexate is an “antifolate” drug, and patients who are taking high doses or receiving chronic therapy are likely to experience severe symptoms of folate deficiency unless they are treated adjunctively with leucovorin. The drug interaction between mercaptopurine and allopurinol is particularly relevant because patients taking conventional chemotherapy are predisposed to development of uric acid crystals, also known as gout. Allopurinol is one of the key drugs used for treating gout, thus increasing the likelihood that these agents may be administered simultaneously.
The drug interaction between mercaptopurine and allopurinol is particularly relevant because patients taking conventional chemotherapy are predisposed to development of uric acid crystals, also known as gout. Allopurinol is one of the key drugs used for treating gout, thus increasing the likelihood that these agents may be administered simultaneously.Advanced
Pharmacogenetics
 Thiopurine methyltransferase (TPMT) plays a role in the metabolic inactivation of mercaptopurine. Approximately 15% of Caucasians have reduced activity of this enzyme, and these individuals are at greater risk for toxicity. TPMT genotyping is now readily available, and genotype-based dosage recommendations are available.
Thiopurine methyltransferase (TPMT) plays a role in the metabolic inactivation of mercaptopurine. Approximately 15% of Caucasians have reduced activity of this enzyme, and these individuals are at greater risk for toxicity. TPMT genotyping is now readily available, and genotype-based dosage recommendations are available.