CHAPTER 28 Neck
The neck extends from the base of the cranium and the inferior border of the mandible to the thoracic inlet.
SKIN
Cutaneous vascular supply and lymphatic drainage
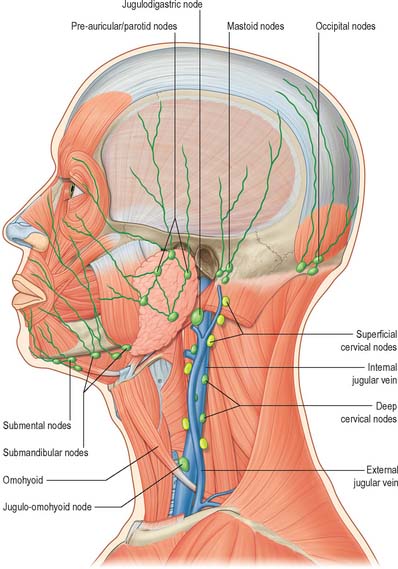
Many lymphatic vessels draining the superficial cervical tissues skirt the borders of sternocleidomastoid to reach the superior or inferior deep cervical nodes. Some pass over sternocleidomastoid and the posterior triangle to drain into the superficial cervical and occipital nodes (see Fig. 28.15). Lymph from the superior region of the anterior triangle drains to the submandibular and submental nodes. Vessels from the anterior cervical skin inferior to the hyoid bone pass to the anterior cervical lymph nodes near the anterior jugular veins, and their efferents go to the deep cervical nodes of both sides, including the infrahyoid, prelaryngeal and pretracheal groups. An anterior cervical node often occupies the suprasternal space.
Cutaneous innervation
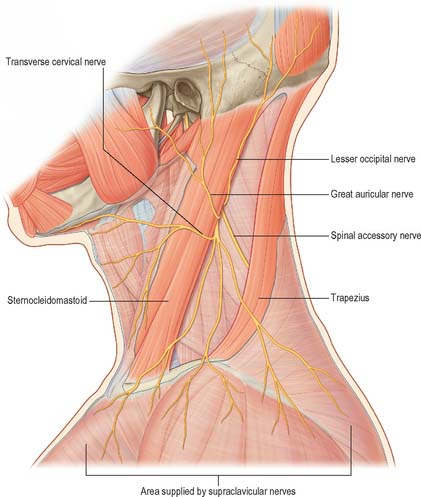
The cervical skin is innervated by branches of cervical spinal nerves, via both dorsal and ventral rami (see Fig. 43.6). The dorsal rami supply skin over the back of the neck and scalp, and the ventral rami supply skin covering the lateral and anterior portions of the neck, and the angle of the mandible (Fig. 28.1). The dorsal rami of the first, sixth, seventh and eighth cervical nerves have no cutaneous distribution in the neck. The greater occipital nerve mainly supplies the scalp; it comes from the medial branch of the dorsal ramus of the second cervical nerve. The medial branches of the dorsal rami of the third, fourth and fifth cervical nerves pierce trapezius to supply skin over the back of the neck sequentially. The ventral rami of the second, third and fourth cervical nerves supply named cutaneous branches (the lesser occipital, great auricular, transverse cutaneous and supraclavicular nerves), via the cervical plexus (Fig. 28.1) (see p. 456 for details of the motor branches of the cervical plexus).
Great auricular nerve
The great auricular nerve is the largest ascending branch of the cervical plexus. It arises from the second and third cervical rami, encircles the posterior border of sternocleidomastoid, perforates the deep fascia and ascends on the muscle beneath platysma with the external jugular vein. On reaching the parotid gland, it divides into anterior and posterior branches. The anterior branch is distributed to the facial skin over the parotid gland and connects in the gland with the facial nerve. This cross innervation between somatic sensory supply (great auricular) and parasympathetic secretomotor fibres to the parotid is considered to be part of the anatomical basis for the phenomenon of gustatory sweating (Frey’s syndrome) seen after parotid surgery, when the nerve is at risk of injury. The posterior branch supplies the skin over the mastoid process and on the back of the auricle (except its upper part); a filament pierces the auricle to reach the lateral surface where it is distributed to the lobule and concha. The posterior branch communicates with the lesser occipital nerve, the auricular branch of the vagus and the posterior auricular branch of the facial nerve.
BONES, JOINTS AND CARTILAGES
The bones and cartilages of the neck are the cervical vertebrae and the hyoid bone, and the cartilages of the upper respiratory tract, including the larynx. The cervical vertebrae, occipital bone and the atlantooccipital and atlanto-axial joints are described in Chapter 42, and the laryngeal cartilages are described in Chapter 34.
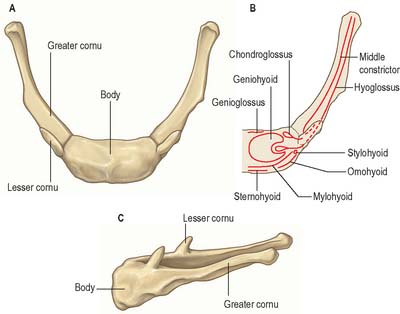
HYOID BONE
The U-shaped hyoid bone (Fig. 28.2) is suspended from the tips of the styloid processes by the stylohyoid ligaments. It has a body, two greater and two lesser horns, or cornua.
TRIANGLES OF THE NECK
Anterolaterally the neck appears as a somewhat quadrilateral area, limited superiorly by the base of the mandible and a line continued from the angle of the mandible to the mastoid process, inferiorly by the upper border of the clavicle, anteriorly by the anterior median line, and posteriorly by the anterior margin of trapezius. This quadrilateral area can be further divided into anterior and posterior triangles by sternocleidomastoid, which passes obliquely from the sternum and clavicle to the mastoid process and occipital bone (Fig. 28.3). It is true that these triangles and their subdivisions are somewhat arbitrary, because many major structures – arteries, veins, lymphatics, nerves, and some viscera – transgress their boundaries without interruption, nevertheless they have a topographical value in description. Moreover, some of their subdivisions are easily identified by inspection and palpation and provide invaluable assistance in surface anatomical and clinical examination.
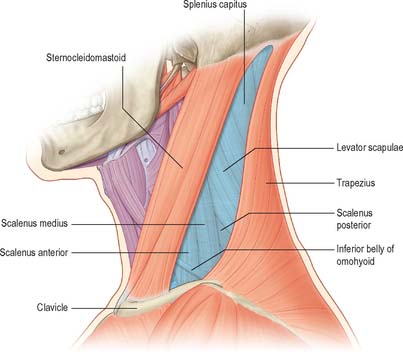
Fig. 28.3 The anterior and posterior triangles of the neck, left lateral aspect. See note in caption for Fig. 28.1
(Adapted from Drake, Vogl and Mitchell 2005.)
ANTERIOR TRIANGLE OF THE NECK
The anterior triangle of the neck is bounded anteriorly by the median line of the neck and posteriorly by the anterior margin of sternocleidomastoid. Its base is the inferior border of the mandible and its projection to the mastoid process, and its apex is at the manubrium sterni. It can be subdivided into suprahyoid and infrahyoid areas above and below the hyoid bone, and into digastric, submental, muscular and carotid triangles by the passage of digastric and omohyoid across the anterior triangle (see Fig. 28.5).
Submental triangle
The single submental triangle is demarcated by the anterior bellies of both digastric muscles. Its apex is at the chin, its base is the body of the hyoid bone and its floor is formed by both mylohyoid muscles. It contains lymph nodes and small veins that unite to form the anterior jugular vein. The structures within the digastric and submental triangles are described in more detail with the floor of the mouth (on p. 501).
POSTERIOR TRIANGLE OF THE NECK
The posterior triangle is delimited anteriorly by the posterior edge of sternocleidomastoid, posteriorly by the anterior edge of trapezius, and inferiorly by the middle third of the clavicle (Fig. 28.3). Its apex is between the attachments of sternocleidomastoid and trapezius to the occiput and is often blunted, so that the ‘triangle’ becomes quadrilateral. The roof of the posterior triangle is formed by the investing layer of the deep cervical fascia. The floor of the triangle is formed by the prevertebral fascia overlying splenius capitis, levator scapulae and the scalene muscles. It is crossed, approximately 2.5 cm above the clavicle, by the inferior belly of omohyoid, which subdivides it into occipital and supraclavicular triangles. The contents of the posterior triangle include fat, lymph nodes (level V – see later), spinal accessory nerve, cutaneous branches of the cervical plexus, inferior belly of omohyoid, branches of the thyrocervical trunk (transverse cervical and suprascapular arteries), the third part of the subclavian artery, and the external jugular vein. The anterior and lateral groups of prevertebral muscles form the floor of the posterior triangle.
Occipital triangle
The occipital triangle constitutes the upper and larger part of the posterior triangle, with which it shares the same borders, except that inferiorly it is limited by the inferior belly of omohyoid. Its floor, from above down, is formed by splenius capitis, levator scapulae, and scaleni medius and posterior; semispinalis capitis occasionally appears at the apex. The triangle is covered by skin, superficial and deep fasciae and inferiorly by platysma. The spinal accessory nerve pierces sternocleidomastoid and crosses levator scapulae obliquely downwards and backwards to reach the deep surface of trapezius. The surface marking of its course is in a line from the junction of the superior one-third and inferior two-thirds of sternocleidomastoid, to the junction of the inferior one-third and superior two-thirds of trapezius. Cutaneous and muscular branches of the cervical plexus emerge at the posterior border of sternocleidomastoid. Inferiorly, supraclavicular nerves, transverse cervical vessels and the uppermost part of the brachial plexus cross the triangle. Lymph nodes lie along the posterior border of sternocleidomastoid from the mastoid process to the root of the neck.
CERVICAL FASCIA
SUPERFICIAL CERVICAL FASCIA
The superficial cervical fascia is usually a thin lamina covering platysma and is hardly demonstrable as a separate layer. It may, however, contain considerable amounts of adipose tissue, especially in females. Like all superficial fascia it is not a separate stratum, but merely a zone of loose connective tissue between dermis and deep fascia, and is joined to both. In the lower cervical region, aponeurotic fibres of platysma gradually fan out in the superficial fascia: they either become skin ligaments or continue into the fascia covering pectoralis major and deltoid. These aponeurotic fibres cover the anterior and lateral cervical regions and often mimic the investing layer of deep cervical fascia, forming a tissue barrier (Nash et al 2005).
DEEP CERVICAL FASCIA
Descriptions of the organization of the deep cervical fascia are largely based on the classic work of Grodinsky & Holyoke in 1938. However recent anatomical studies using techniques such as sheet plastination and confocal microscopy have indicated that the arrangement of the deep cervical fascia is more complicated than was previously thought (Zhang & Lee 2002, Nash et al 2005) (Fig. 28.4).
Tissue spaces and the spread of infection and injectate
The fascial layers of the neck define a number of potential tissue ‘spaces’ above and below the hyoid bone. In health, the tissues within these spaces are closely applied to each other or are filled with relatively loose connective tissue. However, infections arising superiorly, such as dental, tonsillar, vertebral or intervertebral disc-related infections, can alter these relationships. The organisms responsible are often betahaemolytic streptococci or a variety of anaerobes. Streptococci produce proteolytic enzymes which digest the loose connective tissue and so open up the tissue spaces. Since there are no tissue barriers running horizontally in the neck, infections which are not treated promptly can rapidly spread from the infratemporal fossa down to the mediastinum below (see Ch. 55), cross the midline through the sublingual and submental spaces and even track into the axilla.
Understanding the configuration of the cervical fasciae and spaces is essential for the placement of local anaesthetic cervical plexus blocks in the neck to facilitate operations such as thyroidectomy, parathyroidectomy and carotid endarterectomy (Pandit et al 2000). For example, injection of local anaesthetic either in the superficial fascial plane or under the investing fascia of the posterior triangle can provide a similarly effective cervical plexus block (Pandit et al 2003), presumably because the investing fascia between sternocleidomastoid and trapezius is not a well-defined fascial sheet and is indistinguishable from the surrounding loose connective tissue (Zhang & Lee 2002).
The tissue spaces above the hyoid bone are the submandibular and submental spaces beneath the inferior border of the mandible; the pharyngeal spaces; and the prevertebral space near the base of the skull. These spaces are described on pages 524 and 568. Tissue spaces around the larynx are described on page 584.
Radiologically, the portion of the pretracheal space between the strap fascia and the fascia of the thyroid gland is referred as the anterior cervical space. The posterolateral border of the space is the carotid sheath or the fascia of sternocleidomastoid. The anterior cervical space often provides a symmetric landmark on transverse imaging (Smoker & Harnsberger 1991).
In general, cellulitis around the jaw is only likely to develop when the tissues are infected by virulent and invasive organisms at a point where there is access to the fascial spaces: the predisposing causes do not often coincide, and cellulitis is therefore uncommon. Cellulitis in the region of the maxilla is even more uncommon, but fascial space infections may develop in various sites as the result of infected local anaesthetic needles. Since there are no barriers running horizontally with respect to the tissue spaces in the neck, infection entering in this site can rapidly spread more or less unhindered down the neck and may enter the mediastinum (see Ch. 55).
All forms of cellulitides of the neck or deep neck space infections are potentially serious. Narrowing of the upper airway can occur as a result of inflammation and oedema, leading to dyspnoea or obstruction of the upper airway (with stridor) and reduced oxygenation of the lungs. This situation can be extremely difficult to manage by conventional techniques. The increased rigidity and reduced compliance of the tissues mean that manoeuvres such as manual anterior jaw thrust or laryngoscopy may fail to re-open the airway. Specialized techniques, e.g. flexible fibreoptic-assisted tracheal intubation or surgical tracheostomy under local anaesthesia, may be required to provide general anaesthesia to facilitate the surgical drainage and treatment of the cellulitis or deep space abscess.
MUSCLES
The muscles that form part of the musculoskeletal column in the neck are described in Chapter 42. They can be considered in three groups, anterior, lateral and posterior; very broadly speaking, the muscles in these groups lie anterior, lateral or posterior to the cervical vertebrae. The anterior and lateral groups include longi colli and capitis; recti capitis anterior and lateralis; scaleni anterior, medius, posterior and minimi (when present). The posterior muscle group is composed of the cervical components of the intrinsic muscles of the back, overlaid by some of the extrinsic ‘immigrant’ muscles of the back that run between the upper limb and the axial skeleton (trapezius, levator scapulae, see Ch. 42). The intrinsic muscles are arranged in superficial and deep layers. The superficial layer contains splenius capitis and cervicis. The deeper layers include the transversospinal group (semispinales cervicis and capitis, multifidus and rotatores cervicis), interspinales and intertransversarii, and the suboccipital group (recti capitis posterior major and minor and obliquus capitis superior and inferior).
The muscles associated with the pharynx and larynx are described in Chapters 33 and 34 respectively.
Sternocleidomastoid
Sternocleidomastoid (Fig. 28.5) descends obliquely across the side of the neck and forms a prominent surface landmark, especially when contracted. It is thick and narrow centrally, and broader and thinner at each end. The muscle is attached inferiorly by two heads. The medial or sternal head is rounded and tendinous, arises from the upper part of the anterior surface of the manubrium and sterni and ascends posterolaterally. The lateral or clavicular head, which is variable in width and contains muscular and fibrous elements, ascends almost vertically from the superior surface of the medial third of the clavicle. The two heads are separated near their attachments by a triangular interval which corresponds to a surface depression, the lesser supraclavicular fossa. As they ascend, the clavicular head spirals behind the sternal head and blends with its deep surface below the middle of the neck, forming a thick, rounded belly. Sternocleidomastoid inserts superiorly by a strong tendon into the lateral surface of the mastoid process from its apex to its superior border, and by a thin aponeurosis into the lateral half of the superior nuchal line. The clavicular fibres are directed mainly to the mastoid process; the sternal fibres are more oblique and superficial, and extend to the occiput. The direction of pull of the two heads is therefore different, and the muscle may be classed as ‘cruciate’ and slightly ‘spiralized’.
MUSCLES OF THE ANTERIOR TRIANGLE OF THE NECK
Apart from the superficial neck muscles already described, the anterior triangle contains two of the suprahyoid muscles, namely digastric and stylohyoid, and the four infrahyoid strap muscles (Fig. 28.5). The other suprahyoid muscles, namely mylohyoid and geniohyoid, are described with the floor of the mouth on page 501.
Digastric
Digastric has two bellies and lies below the mandible, extending from the mastoid process to the chin (Fig. 28.5). The posterior belly, which is longer than the anterior, is attached in the mastoid notch of the temporal bone, and passes downwards and forwards. The anterior belly is attached to the digastric fossa on the base of the mandible near the midline, and slopes downwards and backwards. The two bellies meet in an intermediate tendon which perforates stylohyoid and runs in a fibrous sling attached to the body and greater cornu of the hyoid bone and is sometimes lined by a synovial sheath. The two bellies of digastric mark out the borders of the submandibular triangle.
Stylohyoid
Stylohyoid arises by a small tendon from the posterior surface of the styloid process, near its base. Passing downwards and forwards, it inserts into the body of the hyoid bone at its junction with the greater cornu (and just above the attachment of the superior belly of omohyoid). It is perforated near its insertion by the intermediate tendon of digastric (Fig. 28.5). The muscle may be absent or double. It may lie medial to the external carotid artery and may end in the suprahyoid or infrahyoid muscles.
Stylohyoid ligament
The stylohyoid ligament is a fibrous cord extending from the tip of the styloid process to the lesser cornu of the hyoid bone. It gives attachment to the highest fibres of the middle pharyngeal constrictor and is intimately related to the lateral wall of the oropharynx. Below, it is overlapped by hyoglossus. The ligament is derived from the cartilage of the second branchial arch, and may be partially calcified.
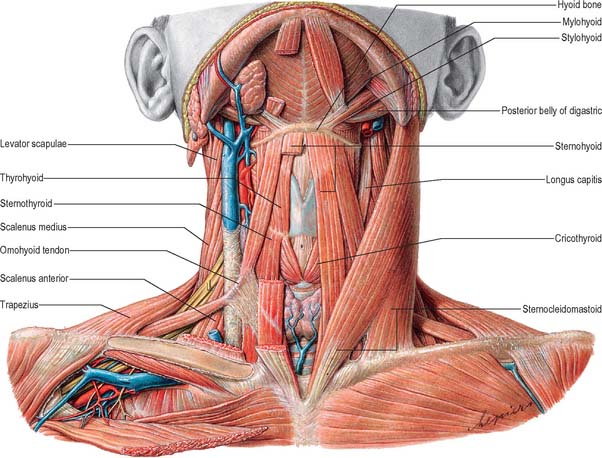
INFRAHYOID MUSCLES
The infrahyoid muscles are organized so that sternohyoid and omohyoid lie superficially and sternothyroid and thyrohyoid lie more deeply (Fig. 28.5). The muscles are involved in movements of the hyoid bone and thyroid cartilage during vocalization, swallowing and mastication and are mainly innervated from the ansa cervicalis.
Sternohyoid
Sternohyoid is a thin, narrow strap muscle that arises from the posterior surface of the medial end of the clavicle, the posterior sternoclavicular ligament and the upper posterior aspect of the manubrium (Fig. 28.5). It ascends medially and is attached to the inferior border of the body of the hyoid bone. Inferiorly, there is a considerable gap between the muscle and its contralateral fellow, but the two usually come together in the middle of their course, and are contiguous above this. Sternohyoid may be absent or double, augmented by a clavicular slip (cleidohyoid), or interrupted by a tendinous intersection.
Omohyoid
Omohyoid consists of two bellies united at an angle by an intermediate tendon (Fig. 28.5). The inferior belly is a flat, narrow band, which inclines forwards and slightly upwards across the lower part of the neck. It arises from the upper border of the scapula, near the scapular notch, and occasionally from the superior transverse scapular ligament. It then passes behind sternocleidomastoid and ends there in the intermediate tendon. The superior belly begins at the intermediate tendon, passes almost vertically upwards near the lateral border of sternohyoid and is attached to the lower border of the body of the hyoid bone lateral to the insertion of sternohyoid. The length and form of the intermediate tendon varies, although it usually lies adjacent to the internal jugular vein at the level of the arch of the cricoid cartilage. The angulated course of the muscle is maintained by a band of deep cervical fascia, attached below to the clavicle and the first rib, which ensheathes the tendon. A variable amount of skeletal muscle may be present in the fascial band; either belly may be absent or double; the inferior belly may be attached directly to the clavicle and the superior is sometimes fused with sternohyoid.
Sternothyroid
Sternothyroid is shorter and wider than sternohyoid, and lies deep and partly medial to it (Fig. 28.5). It arises from the posterior surface of the manubrium sterni inferior to the origin of sternohyoid and from the posterior edge of the cartilage of the first rib. It is attached above to the oblique line on the lamina of the thyroid cartilage, where it delineates the upward extent of the thyroid gland. In the lower part of the neck the muscle is in contact with its contralateral fellow, but the two diverge as they ascend.
Thyrohyoid
Thyrohyoid is a small, quadrilateral muscle that may be regarded as an upward continuation of sternothyroid (Fig. 28.5). It arises from the oblique line on the lamina of the thyroid cartilage, and passes upwards to attach to the lower border of the greater cornu and adjacent part of the body of the hyoid bone.
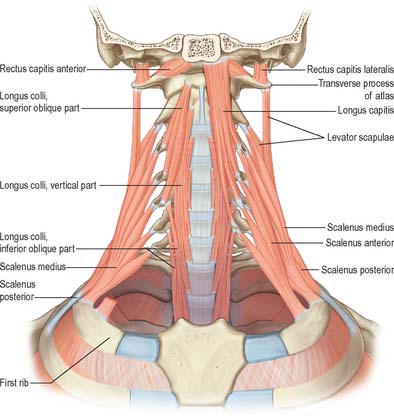
ANTERIOR VERTEBRAL MUSCLES
The anterior vertebral group of muscles are longi colli and capitis, and recti capitis anterior and lateralis (Fig. 28.6), all of which are flexors of the head and neck to varying degrees. Together with the lateral vertebral muscles they form the prevertebral muscle group.
Longus capitis
Longus capitis (Fig. 28.6) has a narrow origin from tendinous slips from the anterior tubercles of the transverse processes of the third, fourth, fifth and sixth cervical vertebrae and becomes broad and thick above, where it is inserted into the inferior surface of the basilar part of the occipital bone.
Longus colli
Longus colli (Fig. 28.6) is applied to the anterior surface of the vertebral column, between the atlas and the third thoracic vertebra. It can be divided into three parts which all arise by tendinous slips. The inferior oblique part is the smallest, running upwards and laterally from the fronts of the bodies of the first two or three thoracic vertebrae to the anterior tubercles of the transverse processes of the fifth and sixth cervical vertebrae. The superior oblique part passes upwards and medially from the anterior tubercles of the transverse processes of the third, fourth and fifth cervical vertebrae to be attached by a narrow tendon to the anterolateral surface of the tubercle on the anterior arch of the atlas. The vertical intermediate part ascends from the fronts of the bodies of the upper three thoracic and lower three cervical vertebrae to the fronts of the bodies of the second, third and fourth cervical vertebrae.
LATERAL VERTEBRAL MUSCLES
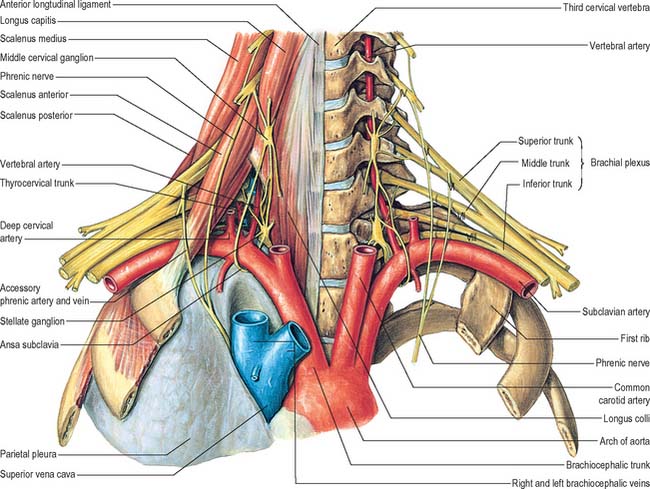
Scaleni anterior, medius and posterior extend obliquely between the upper two ribs and the cervical transverse processes. Scalenus minimus (pleuralis) is associated with the suprapleural membrane and cervical pleura, and is described in Chapter 57.
Scalenus anterior
Scalenus anterior lies at the side of the neck deep (posteromedial) to sternocleidomastoid (Fig. 28.5; see also Fig. 28.18). Above, it is attached by musculotendinous fascicles to the anterior tubercles of the transverse processes of the third, fourth, fifth and sixth cervical vertebrae. These converge, blend and descend almost vertically, to be attached by a narrow, flat tendon to the scalene tubercle on the inner border of the first rib, and to a ridge on the upper surface of the rib anterior to the groove for the subclavian artery.
Scalenus medius
Scalenus medius, the largest and longest of the scaleni, is attached above to the transverse process of the axis and the front of the posterior tubercles of the transverse processes of the lower five cervical vertebrae (Fig. 28.6). It frequently extends upwards to the transverse process of the atlas. Below it is attached to the upper surface of the first rib between the tubercle of the rib and the groove for the subclavian artery.
The anterolateral surface of the muscle is related to sternocleidomastoid (Fig. 28.5). It is crossed anteriorly by the clavicle and omohyoid, and it is separated from scalenus anterior by the subclavian artery and ventral rami of the cervical spinal nerves. Levator scapulae and scalenus posterior lie posterolateral to it. The upper two roots of the nerve to serratus anterior and the dorsal scapular nerve (to the rhomboids) pierce the muscle and appear on its lateral surface.
Scalenus posterior
Scalenus posterior is the smallest and most deeply situated of the scalene muscles (Fig. 28.6). It passes from the posterior tubercles of the transverse processes of the fourth, fifth, and sixth cervical vertebrae to the outer surface of the second rib, behind the tubercle for serratus anterior, where it is attached by a thin tendon.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
ARTERIES OF THE NECK
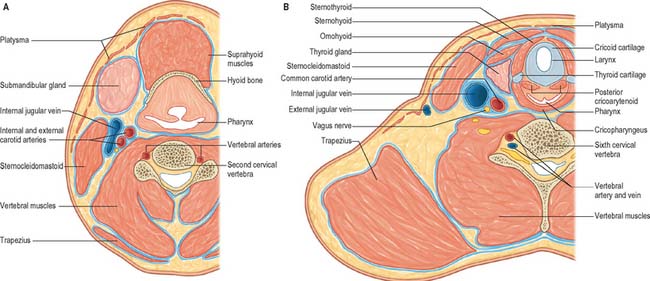
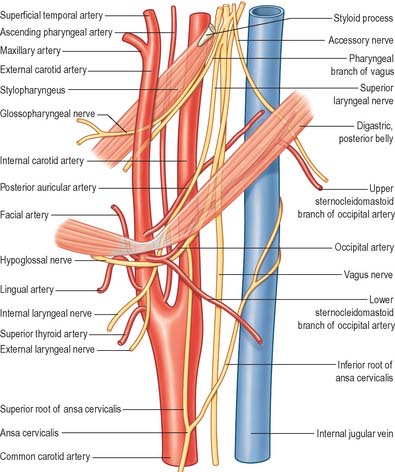
The common carotid, internal carotid, and external carotid arteries provide the major source of blood to the head and neck (Figs 28.7A, 28.8). Additional arteries arise from branches of the subclavian artery, particularly the vertebral artery.
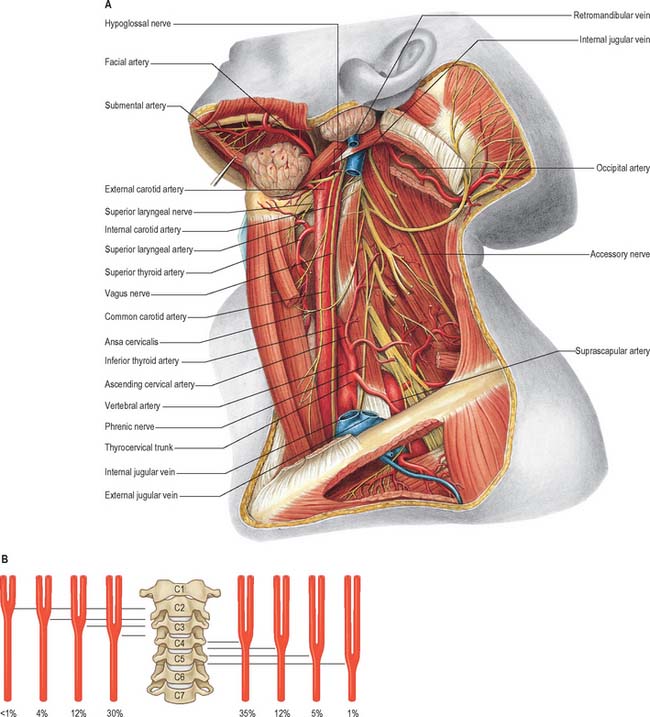
Fig. 28.7 A, Vessels and nerves of the neck, left lateral view: sternocleidomastoid and the greater part of omohyoid and the internal jugular vein have been removed. Compare with Fig. 28.17, which shows a deeper level of dissection. B, Variation in levels of bifurcation of the common carotid artery, related to the cervical vertebrae.
(A, From Sobotta 2006.) (Redrawn with permission from Sobatta 2006.)
Common carotid artery