Answers
A.1 The patient’s presentation is consistent with small bowel obstruction. Since there is little vomiting with this patient, her obstruction is likely to be in the distal small bowel. The most common cause of small bowel obstruction in the developed world is surgical adhesions. The next most common cause is an abdominal wall hernia. Rarer causes include neoplasms and intussusception. Large bowel obstruction may be the result of volvulus, neoplasia or diverticular disease. The patient’s prior bowel surgery suggests adhesive obstruction or possible cancer recurrence.
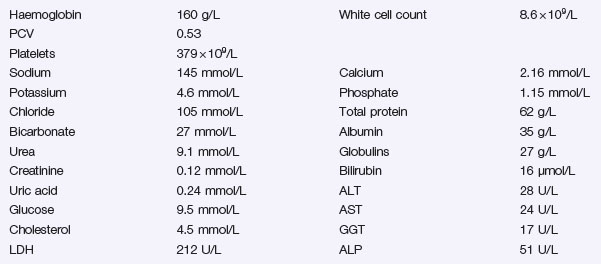
A.2 A complete blood count and basic chemistry panel will help assess the patient’s degree of dehydration. Abdominal films will confirm your diagnosis of a bowel obstruction.
A.3 An elevated haematocrit and blood urea confirm the patient’s dehydration. Elevated blood glucose suggests need for improved diabetes management. The upright and supine abdominal films show dilated loops of small bowel and air–fluid levels. No gas is seen in the colon or stoma confirming the diagnosis of a small bowel obstruction. It is also noted there are no gas shadows overlying the hernial orifices, nor is there gas in the biliary tree which would suggest a rare cause of small bowel obstruction, gallstone ileus.
A.4 Intravenous rehydration with an isotonic solution supplemented with potassium and – if vomiting – intestinal decompression with a nasogastric tube are the mainstays of initial therapy (see Problem 1). Intravenous fluid replacement must take into consideration that lost through nasogastric decompression. Analgesia is prescribed for any discomfort. Because of her elevated blood glucose and a history of poor diabetes control, the patient is started on an insulin infusion. The patient will require close and regular assessment to alert the managing physician to any changes that would alter the conservative plan. These changes include a change in the nature of the pain (colicky to constant), localized tenderness and tachycardia. In addition the patient’s need for analgesia might increase.
A.5 The patient has now been obstructed for at least 3 days and there are no apparent signs of resolution with this plan of conservative management. A CT scan of the abdomen might help define the site and nature of the obstruction. With her past history of bowel cancer she could have recurrence of the disease. It is likely the patient is now going to require surgical intervention.
A.6 There are numerous dilated and fluid-filled loops of small bowel. These loops descend into the pelvis and there appears to be a transition point in the right iliac fossa. No mass lesions are seen.
A.7 The midline wound should be reopened and a careful laparotomy undertaken looking for the site and nature of the obstruction. Any evidence of recurrence of the malignancy should be sought. The viability of the bowel must be carefully assessed. Patients with adhesion-obstruction frequently have areas of ischaemia, either at the site of obstruction or in a closed loop. Since the woman is obese and is diabetic, consideration must be given to delayed primary closure of the superficial layers of the wound to reduce the chance of wound infection.
For determination of wound management in general surgery a simple scoring system can be used that includes the type and complexity of operation, whether the surgery is considered contaminated, the clinical history of the patient including factors of age, smoking and alcohol abuse, steroid use and preoperative albumin level. The greater the score, the more delayed primary wound closure can be considered. Stringent blood glucose in the postoperative patient has been shown to reduce wound infection rates and the best way to achieve this tight blood glucose control is by the use of an insulin infusion with a change to long-acting insulin when appropriate. It should be noted that prior undiagnosed diabetes mellitus is a common problem in patients hospitalized for other reasons.
A.8 Bariatric surgery has seen a dramatic increase over the last decade as obesity-related problems have reached epidemic proportions in a number of Western countries. The surgery has been shown to be effective in producing weight loss in this patient group and also in correcting the complications of diabetes, hypertension and sleep apnoea associated with morbid obesity. There are several different types of operations that are currently employed and these are either restrictive (e.g. gastric band) or malabsorptive (e.g. gastric bypass). Patients with BMIs in excess of 45 are probably best treated with a malabsorptive procedure where success is less dependent on dietary compliance. For those with lesser degrees of obesity and better motivation to modify their dietary habits the reversible laparoscopic band procedure may be a better option.