Myxoinflammatory Fibroblastic Sarcoma
Elizabeth A. Montgomery, MD
Key Facts
Clinical Issues
Slow-growing infiltrative mass usually affecting distal extremities (hands and feet) of adults
Recurrences are common, but metastases are rare
Microscopic Pathology
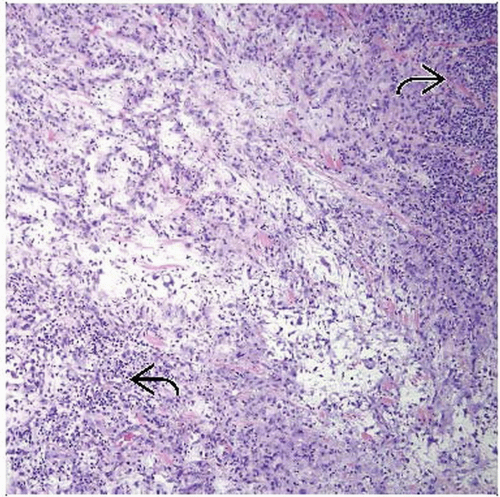
Poorly marginated tumor with fibrosis, hyalinization, myxoid stroma, and inflammatory components
Inflammatory component shows variable mixtures of lymphoplasmacytic cells, eosinophils, neutrophils, histiocytes
Scattered enlarged atypical fibroblasts, some with macronucleoli
Areas with prominent myxoid change
Low mitotic rate
Lesional cells are fibroblasts ultrastructurally
Ancillary Tests
Variable expression of CD34, CD68, EGFR, CD163, CD117, EMA
t(1;10) and amplification of 3p11-12, which it shares with hemosiderotic fibrolipomatous tumour
Negative CD15, CD30, CD45 in cells with macronucleoli
Top Differential Diagnoses
Extranodal Hodgkin disease
Myxofibrosarcoma
Pigmented villonodular tenosynovitis
Hemosiderotic fibrohistiocytic lipomatous lesion
Viral infection
Epithelioid sarcoma
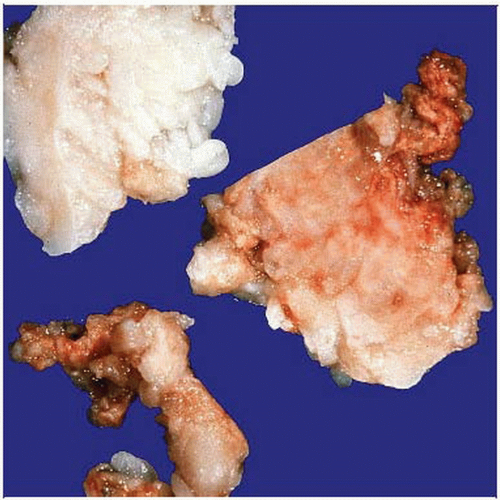 This is a gross specimen of a myxoinflammatory fibroblastic sarcoma. This particular lesion was highly infiltrative and clinically mistaken for pigmented villonodular tenosynovitis. |
TERMINOLOGY
Synonyms
Acral myxoinflammatory fibroblastic sarcoma, inflammatory myxohyaline tumor
Definitions
Low-grade fibroblastic sarcoma characterized by typical acral presentation and inflammatory background often rich in eosinophils
CLINICAL ISSUES
Presentation
Slow-growing infiltrative mass usually affecting distal extremities (hands and feet) of adults
Prognosis
Recurrences are common, but metastases are rare
MACROSCOPIC FEATURES
General Features
Infiltrative masses
Size
1-10 cm, usually 3-4 cm
MICROSCOPIC PATHOLOGY
Histologic Features
Poorly marginated tumor with fibrosis, hyalinization, myxoid stroma, and inflammatory components
Various lesions have different proportions of each component
Inflammatory component shows variable mixtures of lymphoplasmacytic cells, eosinophils, neutrophils, histiocytes
Lesional cells are fibroblasts ultrastructurally
Scattered enlarged atypical fibroblasts, some with macronucleoli
Areas with prominent myxoid change
Fibroblasts often vacuolated as “pseudolipoblasts”
Low mitotic rate
Low proliferative index using Ki-67
ANCILLARY TESTS
Immunohistochemistry
Variable expression of CD34, CD68, EGFR, CD163, CD117, EMA
Negative CD15, CD30, CD45 in cells with macronucleoli
No demonstration of various viral agents
Cytogenetics
t(1;10) and amplification of 3p11-12, which myxoinflammatory fibroblastic sarcoma shares with hemosiderotic fibrolipomatous tumor
t(2;6)(q31;p21.3) reported
DIFFERENTIAL DIAGNOSIS
Extranodal Hodgkin Disease
Patients usually have history of nodal disease
Usually no myxoid areas
Background mostly lymphoid cells, neutrophils not common
Reed-Sternberg cells label with CD15, CD30, and are lymphoid rather than fibroblastic
Myxofibrosarcoma
Usually in proximal extremities of older persons
Typically superficial and lobulated rather than infiltrative
Abundance of myxoid stroma
Richly vascular
Inflammatory cells a minor component
No hyalinized zones
Pigmented Villonodular Tenosynovitis
Also termed tenosynovial giant cell tumor, diffuse type
Often presents in knee joint area of young women
Proliferated around joint space
Proliferation of uniform rounded cells
Background of hemosiderin, histiocytes, lymphoplasmacytic cells
Eosinophils and neutrophils not a feature
Not myxoid
No enlarged atypical cells
Hemosiderotic Fibrohistiocytic Lipomatous Lesion
Classically involves the feet
May form spectrum with both myxoinflammatory fibroblastic sarcoma and with pleomorphic hyalinizing angiectatic tumor
However, no metastases have been recorded for either hemosiderotic fibrohistiocytic lipomatous lesion or pleomorphic hyalinizing angiectatic tumor
Shares t(1;10) and amplification of 3p11-12
Tracks along connective tissue septa
Spindle cells, abundant hemosiderin, histiocytes
Neutrophils and eosinophils not features
Strongly CD34(+)
Viral Infection
Usually involves organs and lymph nodes
Infectious agents can be demonstrated by immunohistochemistry or molecular testing
Viral cytopathic effect consists of nuclear (Cytomegalovirus and herpes simplex virus) or cytoplasmic (Cytomegalovirus) inclusions
Cytomegalovirus effect best seen in stromal cells
Herpes simplex viral effect often seen in epithelial cells
Epithelioid Sarcoma
Distal extremities of adults
Neoplastic cells surround zones of necrosis
Appearance mimics granulomatous process
Minimal inflammation
CD34(+), pankeratin(+), CK5/6(-), loss of nuclear INI1
Malignant
Metastases to regional nodes as well as systemic metastases and death