Musculoskeletal Symptoms and Disorders
LEARNING OBJECTIVES
• ETIOLOGY
Musculoskeletal complaints are among the most frequently encountered primary care visits. Trauma, either acute or overuse, to muscles, ligaments, tendons, bones, or joints is a common cause for symptoms involving the musculoskeletal system. Other diverse etiologies such as autoimmune diseases, vitamin deficiencies, infections, disordered metabolism or clearance, and medication also have to be considered when a patient presents with musculoskeletal symptoms.
• DIAGNOSIS
The diagnosis of specific musculoskeletal complaints requires an organized approach. Eliciting a history of trauma is essential. A positive reply will send the diagnostic process toward traumatic injuries, such as overuse or sports injuries. A negative response directs the inquiries toward nontraumatic causes. Location is the second most important diagnostic clue. Many times different diseases are associated with different locations, e.g., rheumatoid arthritis occurs primarily in the metacarpophalangeal (MCP) joints and proximal interphalangeal (PIP) joints of the hands, whereas osteoarthritis (OA) is predominantly a disease of the weight bearing joints, such as the knee and hip. OA may also affect distal interphalangeal joints (DIP). Whether the pain is in the joint, over a bone, or in a muscular area also helps differentiate etiology. Numbness and tingling or blue, pale discoloration in an extremity are symptoms requiring immediate referral. Finally, physical examination helps confirm the diagnosis. Swelling, decreased or increased range of motion, increased pain on movement, redness, heat, and fever all help discriminate among specific problems.
• COMMON INJURIES RELATED TO TRAUMA/OVERUSE
Plantar Fasciitis
Plantar fasciitis is an overuse injury in runners and walkers; the pain is located on the medial aspect and bottom of the heel. Many times it becomes severe enough to prevent continuation of running for up to 12 months. To avoid the pain, patients tend to walk on the ball and lateral side of the foot. On physical examination, there is pain upon palpation of the medial calcaneal tubercle, passive dorsiflexion of the foot, eversion of the foot, and active dorsiflexion of the big toe. Patients complain of pain in the morning that is worse with the first few steps, or when starting activity with it getting better as they continue to walk or run. It needs to be aggressively treated at the first sign. Continued running will worsen the condition and lead to longer times for healing. Immediate treatment includes ice, but rest, and eventually stretching and strength exercises are the treatments of choice.
Ankle Sprain
Grade 1 sprains include mild swelling, little or no decrease in range of motion, point tenderness over the ligament but no bruising. Grade 2 sprains have moderate swelling, marked decrease in range of motion, and a bruise over the ligament. Grade 3 sprains present with severe swelling, extensive bruising, and severely decreased range of motion. Immediate treatment involves ice, elevation, and rest from 7 days for grade 1 to 4-6 weeks for grade 3.
Tennis and Golfer Elbow (Epicondylitis)
“Tennis elbow” is caused by the repeated use of one-handed backhands. Patients present with tenderness upon palpation just distal to the lateral epicondyle and on resisted extension of the wrist or finger or when the thumb and forefinger are actively opposed like grabbing a tea cup. Two-handed backhands are effective at preventing the initial and any reinjury. Golfer elbow presents with pain upon palpation just distal to the medial epicondyle and resisted flexion of the wrist. Rest should be followed by exercises to stretch and strengthen associated muscles and tendons.
Carpal Tunnel Syndrome
Carpal tunnel syndrome is caused by continuous pressure on the median nerve by the flexor retinaculum along with the other muscles and tendons that form the carpal tunnel that cross the median nerve in the wrist. It was originally thought to be caused by repetitive use of the hands and wrists. It was considered an occupational hazard for typists, barbers, and assembly line workers. However, current evidence has shown that the most important factor is a congenitally narrow carpal tunnel. Overuse of the hands and wrists then contribute to the development of the condition. Patients present with numbness, tingling, or pain in the thumb, first two fingers, and the thumb of the third finger. The opposite side of the third finger and the little finger are not impacted because they are innervated by the ulnar nerve. Diagnosis is confirmed by a positive Tinel sign, which puts pressure on the medial nerve by pressing or tapping over the carpal tunnel. The Phalen test is done by having the patient hold their forearms upright and parallel to the floor, then pointing the fingers down and pressing the backs of the hands firmly together for 1 minute. Positive tests are a duplication of the symptoms.
Knee Injuries
The most common acute knee injuries involve the four primary ligaments of the knee and the meniscus, the layer of cartilage between the tibia and the femur. The ligaments can be strained and sprained (torn). Ligament tears and meniscus damage may have to be repaired surgically to regain full function.
Regardless of the injury, swelling usually occurs. If it occurs immediately, it suggests a ligament tear or fracture of the knee cap. If swelling occurs over a period of hours, then meniscus damage is most likely. In addition, pain upon weight bearing and difficulty bending the knee may also occur. Unfortunately, injuries may involve more than one structure or may not present in a typical fashion. Knees that “give way” or are unstable are usually associated with ligament injuries, while grinding in the knee and the knee that cannot be straightened (“locking”) are typical of meniscus injuries. Injuries to the anterior cruciate (ACL) or posterior cruciate (PCL) ligaments can be tested using drawer tests or versions of classical drawer tests such as the Lachman, which is the most sensitive for PCL injuries. Make sure to test the good knee first for more accurate comparison. Medial collateral (MCL) and lateral collateral (LCL) ligament tears are also detected using drawer tests. Drawer tests put stress on the specific ligament. Excessive movement in a particular direction is diagnostic. Meniscus damage is tested with the McMurray and Apley tests. Any clicking or popping is indicative of meniscus damage. X-rays and MRIs of the knee may be needed to confirm specific diagnoses.
Back Injuries
Most common back injuries involve the lower back and may be fractures, disc injuries, or muscle injuries. The important thing is to recognize symptoms that require immediate medical attention. The most frequent injury involves the muscles of the lower back due to excessive use. These injuries tend to manifest themselves 24 to 48 hours after the inciting incident. Usually, the pain subsides after 72 to 84 hours. Any low back pain that is not getting better after 72 hours needs immediate medical attention. Injuries to the disc are mostly herniated discs (aka protruding, bulging, or ruptured disc). Pain usually is first noticed at the time of injury or immediately thereafter. Sciatica or radiculopathy is nerve pain that shoots down the hip and back of the leg like an electric shock, or numbness and/or tingling in one or more lower extremities and warrants immediate referral for evaluation. If persistent pain occurs in the elderly or is insidious in onset, fractures due to osteoporosis or systemic diseases such as ankylosing spondylitis need to be ruled out. Lack of attention can lead to permanent nerve damage and/or muscle weakness. CT scans, MRIs, x-rays of the spine may be required to confirm suspected diagnoses.
• COMMON ARTHRITIDES
Causes of joint pain include repetitive overuse, repeated trauma, immunologic, metabolic, and infectious disorders. There are several keys to accurate diagnosis including the number and location of joints involved, acute versus insidious onset, other symptoms such as serious eye disease, skin rash, patterns of the discomfort, plus fatigue and malaise.
If the pain is of acute onset and only occurs in a single joint (monoarticular), then traumatic and overuse disorders such as bursitis, tendonitis, sprains, and fractures should be suspected. A careful history regarding overuse or trauma is important in ruling out this cause. In particular, in elderly patients, fracture due to osteoporosis and/or falls should be suspected and ruled out. Infectious causes like septic arthritis and osteomyelitis, should be also suspected. CT scans, MRIs, and arthrocentesis (aspiration of synovial fluid from the affected joint) may be required for diagnosis. The presence of cloudy fluid, white or red blood cells, and bacteria are abnormal findings. Aspirated synovial fluid will be cultured. A CBC will show a typical bacterial infection white count (>10,000 WBC, > 80% mature and immature PMNs) in septic arthritis. Arthrocentesis is also indicated if gout or pseudogout is suspected. Classically associated with the big toe, gout can occur in any joint in the lower body plus hands and wrists. Typically the joint is exquisitely painful, swollen, and warm to the touch. High-plasma uric acid levels due to overproduction or undersecretion are usually present. Synovial fluid contains urate crystals upon microscopic examination. Pseudogout presents in the knee joints of elderly patients with gout-like symptoms. However, the synovial fluid contains precipitated calcium pyrophosphate dihydrate rather than urate crystals.
Acute onset, migratory polyarthritis is most likely gonococcal arthritis or post-streptococcal acute rheumatic fever. Other polyarthritides such as rheumatoid arthritis (and its variants) and systemic lupus erythematosus (SLE) can present acutely but are typically more insidious in onset. Lastly, acute onset polyarthritis occurring in large joints, such as the knees, in young males may indicate Reiter syndrome an autoimmune arthritis associated with conjunctivitis and urethritis.
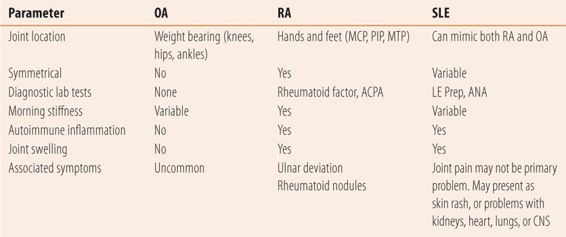
Joint pain occurring in multiple joints with a chronic, intermittent, or insidious onset is associated with noninflammatory arthritis such as OA, autoimmune arthritides such as SLE, and rheumatoid arthritis and its variants. Table 15.1 presents key features used in the differential diagnosis of these common disorders.
| TABLE 15.1 | Differential Diagnosis of Chronic Polyarticular Arthritis |
Osteoarthritis (Degenerative Joint Disease or DJD)
The most frequently occurring arthritis is OA. Nearly 27 million patients suffer from the disease in the United States including 70% of those over 65 years of age. OA is generally regarded as a noninflammatory arthritis, and is associated with aging, repetitive trauma, and obesity. However, recent research into genetics and synovial fluid markers has brought new information regarding the type and role of inflammation and potential genetic links to biostructural issues. OA primarily affects the larger weight bearing joints such as the knees, hips, and ankles, but can involve any previously injured or overused joint including those of the shoulder, spine, and hands. The most common cause is excessive load caused by obesity and/or repetitive overuse. Also deficiencies in biostructure (cartilage, bone, muscle, ligaments), but with a normal load can cause OA.
Diagnosis is primarily a clinical one. Pain and decreased range of motion are primary findings. Crepitus or grinding sensations can be felt over the joint when flexion and extension of the joint occur. Point tenderness on palpation is not uncommon. The degree of pain varies with severity of the disease. In the early stages pain is worse after rest, with the pain disappearing in minutes upon movement. In the later stages pain may be constant and weight bearing activity increases in pain are common. There is generally little swelling, and no associated symptoms, systemic manifestations, or abnormal laboratory tests as there are in autoimmune arthritides such as rheumatoid arthritis. Occasionally, x-ray of the joints reveals degenerative changes, especially joint space narrowing.
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is an autoimmune, inflammatory, erosive arthritis that affects 1.5 million people per year. Two times as many women as men are diagnosed with RA. A systemic disease, early symptoms may include primarily fatigue and malaise with intermittent bouts of joint pain. Multiple small joints are involved usually the MCP, PIP, wrist, metatarsophalangeal (MTP), and ankle joints. The disease tends to be symmetrical, occurring in both the hands or toes but not necessarily the same joints on both hands. It is a naturally cyclical disease, where patients with active disease complain of morning stiffness lasting up to 1 hour. Affected joints are swollen, hot, and painful with decreased range of motion. If untreated the disease progresses with joint erosion and loss of function to cause deformities. As the disease progresses, other joints can become involved. Ulnar deviation of the fingers is common if untreated. The disease can also impact other organs in the body including the heart and lungs. Patients with RA present with elevated erythrocyte sedimentation rate (ESR) due to large quantities of immune complexes in the plasma, and elevated high-sensitivity C-reactive protein (hs-CRP). Unfortunately, these acute phase reactants are not specific for RA. The rheumatoid factor (RF), usually measured as an IgG or IgM autoantibody. Titers of >1:160 are diagnostic. Similarly, anticyclic citrullinated peptide antibodies (ACPA) are more specific for RA and can be found before clinical signs and symptoms of disease are present. Antinuclear antibodies (ANA) are usually absent. Because of the intermittent cyclic nature of the disease and its insidious onset in 90% of the cases, the diagnosis of early disease can be difficult. Serologic diagnosis is complicated by the small percentage of patients with RA who will have positive ANA as well as patients with other autoimmune diseases such as SLE who may have positive RA titers. To aid in the diagnosis of RA, the American College of Rheumatology developed a scoring guideline (Table 15.2).
| TABLE 15.2 | Criteria for the Diagnosis of Rheumatoid Arthritis |
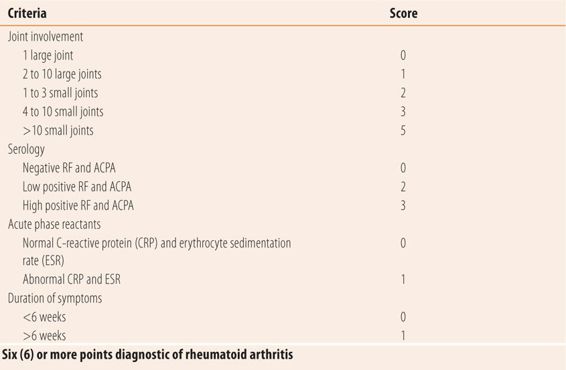
Treatment is centered on stopping the autoimmune-mediated joint destruction. In managing patients with RA, a combination of symptoms set forth in various scoring systems (ACR-20, disease activity score-28, and simplified disease activity index), radiological changes, and acute phase reactants (ESR and hs-CRP) are used to monitor efficacy of drug treatment. Successful treatment is indicated by falling titers of acute phase reactants, no radiographic changes, and decreasing symptom scores.
Common Rheumatoid Arthritis Variants
There are several common arthritides that are variants of RA. Presentation is similar but with specific additional associated symptoms. Felty’s syndrome is RA with leukopenia, and occasionally anemia or thrombocytopenia and/or splenomegaly. Sjogren syndrome is RA plus conjunctiva sicca (dry eyes) and xerostomia (dry mouth). Psoriatic arthritis occurs in about 10% of patients with psoriasis.
Systemic Lupus Erythematosus
SLE is a systemic disease that can present with joint pain that can mimic both RA and OA. The number of patients with SLE is similar to that of RA. Eighty-five percent of patients with SLE are women and initial diagnosis occurs between the ages of 15 and 45. If untreated, the disease is commonly fatal. Sixty years ago the 5-year survival rate was less than 50%. Today the 15-year survival rate is over 80%. Because of its systemic nature, diagnosis should be suspected if patients present with two or more common systemic symptoms. Those include skin rash, photosensitivity, arthritis, renal damage, pulmonary symptoms, cardiac symptoms, CNS symptoms such as seizures or psychosis, hematological abnormalities, and constitutional symptoms such as fatigue, malaise, fever, or weight loss. Laboratory tests historically included LE Prep, a test using blue dye to detect SLE antibodies. This test has been replaced due to its limited accuracy by ANA which is diagnostic. Over 90% of patients with active SLE will have elevated titers. Double-stranded ANA is specific for SLE, but is present in less than half of the patients. Anti-Smith antibodies are also more specific than ANA titers. About 50% of patients will have low complement levels (C3 and C4). Patients suspected of SLE need urinalysis and renal function tests, LFTs, CBC to help identify specific organ system involvement and monitor disease progression. Treatment with immunosuppressives helps to prevent multiorgan damage and eventually death.
Other Autoimmune Arthritides
There are two other autoimmune arthritides of interest. Ankylosing spondylitis occurs in males with HLA B27 antigen. It causes inflammation of the spine, which eventually leads to ossification of the discs and surrounding connective tissue, leading to vertebral fusion. Scleroderma occurs primarily in females and involves an inflammatory process that increases the deposition of collagen in many tissues especially blood vessels. It causes an autoimmune vasculitis, leading to Raynaud’s phenomenon, plus a tightening and thickening of the esophagus and skin of the finger and face. Eventually it can involve the thyroid, intestinal tract, heart, lungs, and kidneys. Scleroderma is also known as progressive systemic sclerosis.
• BONE DISEASES THAT CAN BE CONFUSED WITH JOINT PAIN
Osteopenia is a generalized term describing the loss of bone mineral from trabecular portions of bones. Generally, the presence of osteopenia is detected by dual energy x-ray absorptiometry (DEXA) of the hip bones. DEXA results are expressed as T scores, which estimate bone mineral density. T scores are based on the number of standard deviations from the mean of healthy 30-year-old women of the patient’s ethnicity. Normal is a score of –1.0 or higher. A T score of –1.0 to –2.5 is osteopenia and a T score >–2.5 (more negative) is considered diagnostic of osteoporosis. Ultrasound of the heel bone is not as accurate as DEXA because the test measures cortical rather than trabecular or porous bone.
There are two primary types of osteopenia. Osteomalacia is due to vitamin D deficiency and involves bone mineral density only. Patients with lactase deficiencies, those on enzyme-inducing anticonvulsants, and/or who have little or no sun exposure are at higher risk for developing osteomalacia. In children, it is called rickets. The bones soften and become misshapen because the cartilaginous matrix is still in place but without the stiffening influence of calcium and phosphate. Therapy with vitamin D and calcium and sometimes vitamin K restore bone mass and strength. In adults, there is no misshapen bone structure and symptoms include dull, unrelenting, aching pain with widespread distribution. When asked to point to where the pain is located, patients will point to the long bones of the forearms and legs rather than the joints. The pain is usually not relieved by NSAIDs. Most will have serum 25-OH vitamin D levels well below 20 ng/mL. Bone scans will reveal Looser’s lines, small linear microfractures in the bone.
The other causes of osteoporosis is age and postmenopausal status. Osteoporosis, rather than being a vitamin D deficiency, is due to a disorder of bone turnover. Normally, there is a balance between osteoclast activity, which breaks down bone tissue, and osteoblast activity that rebuilds bones. Osteoporosis is an imbalance of osteoclast/osteoblast activity where osteoclast activity dominates, causing bone mineral loss as well as loss of cartilaginous bone matrix. This is most harmful to the more porous trabecular bone that contains the marrow. Cortical or dense bone is less affected. Therefore, the complication of osteoporosis is fractures of bone that is primarily trabecular, i.e., spinal vertebrae, hip, and wrist. After onset of osteoporosis, the patient, regardless of treatment, can never completely regain all lost bone mass due to the loss of matrix.
• KEY REFERENCES
1. Kiriakidou M. Systemic lupus erythematosus. Ann Intern Med. 2013;159(7):ITC4-1.
2. Aletaha D, Neogi T, Silman AJ, et al. 2010 Rheumatoid arthritis classification system: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69:1580-1588.
3. Bijlsma JWJ, Berenbaum F, Lafeber FPJG. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377:2115-2126.
4. Sinusas K. Osteoarthritis: diagnosis and management. Am Fam Physician. 2012;85:49-56.
5. Jackson JL, O’Malley PG, Kronke K. Evaluation of acute knee pain in primary care. Ann Intern Med. 2003;139:575-588.
6. Grover M. Evaluating acutely injured patients for internal derangement of the knee. Am Fam Physician. 2012;85:247-252.
7. Sembrano JN, Polly DW. How often is low back pain not coming from the back? Spine. 2008;34:E-27-E32.
8. Czajka CM, Tran E, Cai AN, DiPreta JA. Ankle sprains and instability. Med Clin North Am. 2014;98:313-329.
9. Rosembaum AJ, DiPeta JA, Misner D. Plantar heel pain. Med Clin North Am. 2014;98:339-352.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



