Chapter 27 Musculoskeletal disorders
With contribution from Greg de Jong
Introduction
A survey of US adults in December 2007 found that 42% of respondents reported that they were in pain on the day of the survey, 1 in 4 experiencing acute pain, with 72% indicating they had experienced pain in the last 12 months. Of particular interest, 70% of people who reported acute pain, 45% recurrent pain and 20% of chronic pain sufferers indicated that they did not seek medical advice for their condition. The common reason given for the reluctance to seek advice included the perception that people take too many pills, a reluctance to take general medication for pain in a specific location, or that oral prescriptive medications upset their stomachs.1
In light of such statistics and concerns it would appear pertinent to investigate all available options in regard to the management of musculoskeletal care. Interestingly, in a further US study, knowledge of complementary health care providers and interventions specific to the most prevalent musculoskeletal conditions was found to be surprisingly low, with the exception of chiropractic treatment. However, most respondents indicated that they would be interested in accessing complementary health care for musculoskeletal injury and pain if costs were subsidised and that their doctors considered such interventions as reasonable.2
In Australia, national surveys indicate substantial usage of acupuncture, chiropractic and osteopathic treatments, particularly for back complaints. Approximately 1 in 4 Australians surveyed visited 1 of these providers — 16.1% chiropractors, 9.2% acupuncturists and 4.6% osteopaths — amounting to approximately 32.3 million visits per year, with over 90% considering their treatments to be somewhat helpful or very helpful.3
A British survey of patients with chronic musculoskeletal pain demonstrated similarly high levels of usage for all forms of complementary therapies. In the survey, 84% of participants reported having used a complementary treatment in the last year with 65% as present users. Three people used over-the-counter complementary medicines for every 2 who sought treatment from a provider with the most used products being glucosamine and fish oils. Of respondents, 69% used conventional medicines concurrently with their complementary treatment of choice.4
Acute musculoskeletal pain and/or injury management
Acute pain is defined as pain of less than 3 months.5, 6 It may arise as a result of injury, repetitive movement or be insidious in nature. It has been highlighted by the Australian Acute Musculoskeletal Pain Guidelines Group7 that most incidences of acute musculoskeletal pain are of short duration (less than 3 months) and will not lead to chronic pain and disability, although mild symptoms may persist.
Furthermore, in the majority of cases the determination of cause and specific diagnosis is not required, whilst simple interventions, including information, assurance and the maintenance of appropriate levels of activity, when coupled with pharmacological and non-pharmacological approaches will be satisfactory without the need for extensive investigation. What is critical is to identify as early as possible the minority of patients who are either presenting with a serious medical condition (‘red flags’) or are at risk of developing chronic musculoskeletal pain due to psychosocial factors (‘yellow flags’).8 (See Tables 27.1 to 27.3.)
Table 27.1 Identifying features (‘red flags’) of serious conditions associated with acute low back pain
| Feature or risk factor | Factor/condition |
|---|---|
| Infection | |
| Fracture | |
| Tumour | |
| Absence of aggravating features | Aortic aneurysm |
(Source: Australian Acute Musculoskeletal Pain Guidelines Group 2003 Evidence-Based Management of Acute Musculoskeletal Pain. National Health and Medical Research Council)
Table 27.2 Identifying features of serious conditions associated with acute thoracic spinal pain
| Feature or risk factor | Condition |
|---|---|
| Fracture | |
| Infection | |
| Tumour | |
| Other serious conditions |
(Source: Australian Acute Musculoskeletal Pain Guidelines Group 2003 Evidence-Based Management of Acute Musculoskeletal Pain. National Health and Medical Research Council)
Table 27.3 Identifying features of serious conditions associated with acute neck pain
| Feature or risk factor | Condition |
|---|---|
| Infection | |
| Fracture | |
| Tumour | |
| Neurological symptoms in the limbs | Neurological condition |
| Cerebrovascular symptoms or signs, anticoagulant use | Cerebral or spinal haemorrhage |
| Cardiovascular risk factors, transient ischaemic attack | Vertebral or carotid aneurysm |
(Source: Australian Acute Musculoskeletal Pain Guidelines Group 2003 Evidence-Based Management of Acute Musculoskeletal Pain. National Health and Medical Research Council)
Lifestyle, mind–body issues and acute musculoskeletal injury
While lifestyle and mind–body medicine interventions may not be necessary during the initial stage of acute injury management, it is the assessment of these factors that form the core tool for identifying those patients who are most likely to progress onto chronic musculoskeletal conditions (‘yellow flags’) and hence require greater monitoring and follow up.8
For instance, in regard to low back pain, psychosocial and occupational factors are considered to have greater clinical value in predicting chronicity than clinical presentation.9, 10 A systematic review of psychosocial factors in 2008 identified that the most pertinent risks of failure to return to work after a low back injury were a low expectation of recovery and fear-avoidance behaviours.11 Depression, job satisfaction and stress levels did not appear to have an impact on the likelihood of return to work after injury.
A variety of evaluation tools, such as the Acute Low Back Screening Tool,8 Roland Morris Disability Questionnaire, Fear Avoidance Beliefs Questionnaire, Oswestry Low Back Pain and Disability Questionnaire and so forth, have subsequently been developed to assess various aspects of psychosocial behaviours, particularly in regard to low back pain. Where such factors are identified as pertinent during an acute episode of injury early referral to behavioural strategies outlined under chronic musculoskeletal management should be considered.
Remaining active versus bed rest and collars
Current evidence suggests remaining active after an acute musculoskeletal injury is preferable in most instances to bed rest or immobilisation. A Cochrane review in 200512 indicated that advice to remain active was preferable to bed rest for acute low back pain, although there was no indication of difference where sciatic symptoms were present. Fordyce13 compared the use of analgesia, exercise, time contingent and behaviour contingent activity in addressing acute low back pain and found that the latter group who had been advised to ‘let pain be your guide’ were less likely to progress to chronic pain. In the instance of neck pain, remaining active was reported to be of more benefit than rest in a collar after whiplash injuries of the neck.14 Thus it would appear that remaining as active as possible while respecting pain levels is the best encouragement for patients experiencing acute musculoskeletal pain. Exceptions, however, do apply in the instance where musculoskeletal injury is significant enough to require protection from further damage (e.g. strains of ankle and knee ligaments).15
Behavioural therapy
A recent review reported on the rationale and evidence supporting 3 frequently used psychosocial interventions for chronic pain; namely, cognitive behavioural therapy (CBT), operant behavioural therapy and self-hypnosis training.16 The study concluded that CBT and operant behavioural therapy treatments have a focus on factors that exacerbate or maintain suffering in chronic pain, and should be considered as part of a multidisciplinary treatment paradigm. Whereas self-hypnosis training may be of benefit, it appears to be no more (or less) effective than other relaxation strategies that include hypnotic elements.
Education
A summary of findings on patient education from controlled trials on acute low back pain by the Australian Acute Musculoskeletal Guidelines Group7 indicated that practitioner-delivered information was more effective than brochures and booklets. Furthermore, information provided in the mail was less effective than in person. In regard to neck pain in general, a Cochrane review indicated no strong evidence for the effectiveness of educational interventions.17
Exercise
A Cochrane review18 indicated that for acute low back pain exercise was no more effective than no treatment or other conservative treatments. In the subacute phase limited evidence suggests that a graded exercise program may improve absentee rates. A literature review in 200819 supported this view, indicating that the most appropriate advice at an early stage was the continuation of normal activities as effectively as possible rather than an exercise program. Exercise at the subacute stage (>4 weeks) onwards was indicated to decrease pain and disability, although no specific exercise program was indicated as superior.
A Cochrane review of exercises for acute neck pain indicated limited evidence supporting active range of motion exercises or home-based exercise programs, including both mechanical and whiplash associated disorders.20 Exercise has been found beneficial in terms of short-term recovery and long-term function in relation to rotator cuff disease of the shoulder.21
Nutritional supplements
Vitamin D
Increasing evidence indicates the importance of vitamin D deficiency in muscle pain and weakness. In a study of vitamin D deficiency in a community health clinic, 93% of patients with non-specific musculoskeletal pain were found to have vitamin D deficiency, and 100% of those were under 30 years of age.22 The authors highlighted the fact that vitamin D deficiency should be considered in all patients with non-specific muscular pain, including those not usually expected to be deficient — the young and non-house-bound.
A review of papers on vitamin D deficiency in 2006 concluded that vitamin D deficiency should be considered as a differential diagnosis in the evaluation of musculoskeletal complaints and treated accordingly.23 Furthermore, musculoskeletal weakness (e.g. of the thigh muscles) was an additional consequence of vitamin D deficiency. A pilot study of vitamin D deficiency in chronic pain patients found that in those patients with vitamin D deficiency (26%; serum 25-hydroxyvitamin D [25(OH)D<20ng/l) using opioid drugs, the mean morphine equivalent dose and duration of use was significantly higher than non-vitamin D deficient patients.24
It is a misassumption that a sunny environment is necessarily protective against vitamin D deficiency. Case studies in Saudi Arabia and Egypt demonstrate significant relationships between vitamin D deficiency and chronic low back pain.25, 26 In Saudi Arabia 83% of patients with chronic low back pain were found to be vitamin D deficient with the majority successfully treated with vitamin D supplementation over a 3-month period.25 In the Egyptian study 81% of low back pain patients and 60% of controls were found to be vitamin D deficient indicating that despite the sunny climate many Egyptians were vitamin D deficient. Both limited duration of sun exposure and limited area of skin exposure were associated with deficiency findings.26 A small study of urban Australian Aboriginals comparing low back pain subjects with controls also demonstrated a 100% vitamin D deficiency amongst the 8 patients with low back pain.27
Treatment with vitamin D has been found to be effective for many low back pain patients in several case studies. It must be noted, however, that most studies used either intramuscular injections of between 10 and 30 000IU28,29 or high dose supplementation at levels of 50 000IU.30, 31 The one exception was a Saudi Arabian study in which levels of 5000IU/day (<50kg) or 10 000IU/day (>50kg) were used. In all instances clinical improvements were observed in the majority of patients within 3 months.25
A caveat to vitamin D supplementation addresses the question as to whether vitamin D has any effect on diffuse musculoskeletal pain that may be associated with low vitamin D levels. Warner and Arnspiger32 recently reported that low vitamin D levels were not associated with diffuse musculoskeletal pain, and treatment with vitamin D did not reduce pain in patients with diffuse pain and who have low vitamin D levels.
Magnesium and/or alkaline minerals
Anecdotally magnesium is often reported to assist in the alleviation of muscular pain and spasms. Physiologically magnesium plays a significant role in the musculoskeletal system being responsible in part for control of neuronal activity, neuromuscular transmission and muscular contraction/relaxation phases.33
However, whilst studies indicate successful use of magnesium sulfate for tetanic muscle spasms34 and magnesium glycerophosphate in the reduction of muscle spasticity in multiple sclerosis,35 there is minimal current evidence to support or reject magnesium use in the otherwise well patients with musculoskeletal pain/injury.
One open prospective study of 82 patients with chronic low back pain provided an alkaline mineral supplement demonstrated a clinically significant 49% drop on the Arhus Low Back Pain Rating Scale over a 4-week period. Interestingly, of the multi-minerals used in the formula, including potassium, calcium, iron and copper, only magnesium demonstrated changes in serum (11% increase) and plasma readings (3% decrease) after supplementation.36 The authors also noted an increased blood buffering capacity from the alkaline formula and concluded with the view that a disturbed acid-base balance might be responsible for chronic low back pain.36
Omega-3 essential fatty acids
The resolution of acute inflammation is a dynamic process that requires an appropriate host response, tissue protection and resolution of inflammation. Increasing evidence recognises the role of omega-3 derived mediators (e.g. resolvin, protectin) in regulating the resolution of the acute inflammatory process.37, 38 To date no trials have been undertaken in regard to the use of omega-3 supplements during acute inflammation.
However, given the effectiveness of non-steroidal anti-inflammatory drugs (NSAIDs) for both acute and chronic low back pain, and the assumed role of omega-3 essential fatty acids in the inflammatory process, a controlled study was undertaken amongst non-surgical neck and low back pain patients attending a neurosurgical practice.39 Patients were requested to take 1200mg/day of omega-3 supplements (EPA/DHA) and followed up after 1 month. Although response rate to recall by mail was only 50%, 78% remained compliant to recommended dosage, with 22% doubling the dosage themselves. Sixty percent of patients reported that their overall pain had improved, 60% that joint pain had improved and 59% discontinued their NSAID. Eighty percent reported that they were satisfied with their improvement.39 This early evidence indicates that further studies are required in this area, given the lack of complications associated with omega-3 supplementation as compared to NSAIDs.
B Vitamins
A single randomised double-blind placebo-controlled study of 60 patients with non-surgical low back pain found that an active group receiving intramuscular B12 injections showed a statistically significant decrease in pain as measured on an Visual Analogue Scale (VAS) and a disability questionnaire. The active group also had a significant decrease in paracetamol use in compare to the placebo group.40
Clinical trials of low back pain have also been undertaken to establish whether B group vitamins (B1 thiamine nitrate 25mg, B6 pyridoxine hydrochloride, B12 cyanocobalamin 0.25mg; 3 x 2 capsules per day for 3 weeks) added to diclofenac can shorten the need for this medication. A clinically significant difference in diclofenac use in favour of the B vitamin group was noted for patients with severe pain at the beginning of the trial.41 However, no further trials have been undertaken to evaluate the analgesic role of the B group vitamins in this regard.
Herbal medicines
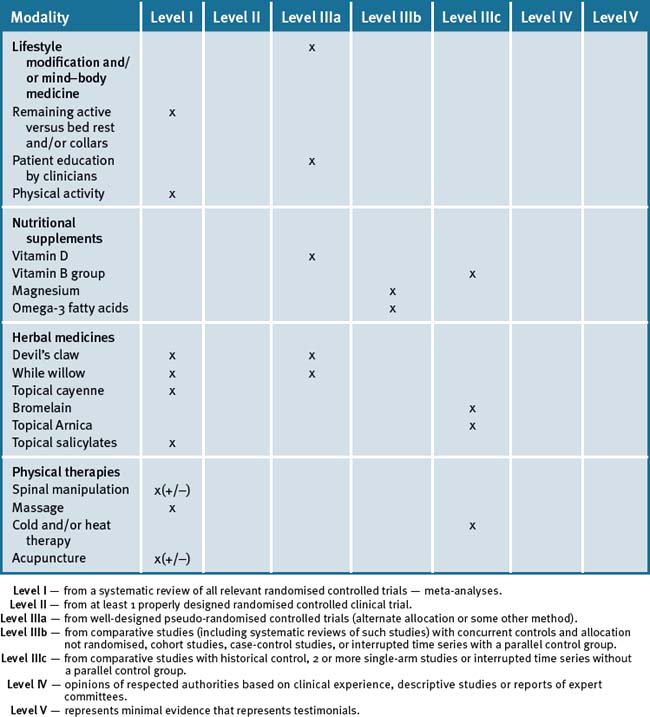
A 2007 Cochrane review of herbal medicines for the low back identified 3 herbs; Harpagophytum procumbens (devil’s claw), Salix alba (white willow bark) and Capsicum frutescens (cayenne) as potentially beneficial in reducing low back pain, however, it was noted that the quality of studies were generally poor.42 While other herbs are often recommended for acute and chronic musculoskeletal conditions, evidence is usually of low quality, by inference from non-human studies or lacking at present.
Devil’s claw (Harpagophytum procumbens)
Reductions in low back pain and muscle stiffness have been reported in a series of double-blind studies using a Devil’s Claw extract Ll 174.43, 44 A double-blind study comparing devil’s claw (50 or 100mg harpagogoside)/day to rofecoxib (12.5mg) found equivalent benefit over a 6 week period,45, 46 with follow up after 1 year47 highlighting that devil’s claw was well tolerated and that treatment gains were sustained.
A recent review investigated 28 trials of which 20 reported adverse events.48 In none of the double-blind RCTs was the incidence of adverse events during treatment with Harpagophytum procumbens higher than during placebo treatment. Also, minor adverse events occurred in approximately 3% of the patients, these being mainly gastrointestinal in nature. A few reports of acute toxicity were found but there were no reports of chronic toxicity. Since the dosage used in most of the studies was at the lower limit and since long-term treatment with Harpagophytum products was advised, more safety data are required.
White willow bark (Salix alba)
In a randomised placebo-controlled study of patients, 39% of active patients treated with white willow bark, standardised to 240mg salicins daily, were found to be pain free. In the control group only 6% achieved the same result over a 4-week trial period.49 In an open trial comparing 240mg salicins daily, 120mg salicins daily and a control group of conventional treatment, results favoured the 240mg salicins daily group (40% pain free over 4 weeks compared to 19% for the 120mg salicin group and 18% for control).50
White willow bark, 240mg salicins daily, has been found to be equivalent to rofecoxib in use for acute episodes of chronic low back pain. The need for rescue dosages of NSAIDs or tramadol was found to be 10% in the white willow bark group and 13% with rofecoxib use.51
Cayenne (Capsicum frutescens)
As noted, a 2007 Cochrane review found 3 low quality trials supporting the use of topical preparations of Capsicum frutescens for low back pain. Cayenne trials were carried out in the form of plaster applications and outcomes were judged to be modest in effect.42
Bromelain
A single open study of the use of bromelian for acute knee pain in the absence of osteoarthritis or rheumatoid arthritis demonstrated that 400mg dosages provided significantly more benefit in pain, function and a decrease in knee joint stiffness as compared to a 200mg dosage.52
Topical analgesia
Arnica
Topical arnica is often advocated to reduce bruising and swelling in acute injury. Whilst no clinical trials have been performed for acute musculoskeletal injury, post-surgical trials involving wound healing after carpal tunnel syndrome (homeopathic arnica and topically applied arnica ointment) indicate reduced pain levels 2 weeks post surgery when compared to placebo subjects.53 Further studies with this gel are required to substantiate its wide spread use for acute injury, swelling and bruising.
Topical salicylates
Salicylate is considered to work as a counter irritant in its role as a topically applied pain reducing agent. A review of the use of topical salicylates for acute injuries such as low back pain, ligamentous strains and mild athletic injuries revealed that 67% of active subjects received greater than 50% pain reduction from topical application as compared to only 18% of controls. No comparison studies have been undertaken to compare the use of such topical applications to other conventional therapies.54
Physical therapies
Manipulation
Reviews are mixed as to the benefits of manipulation in managing acute musculoskeletal back pain. A Cochrane review in 2009 established that manipulation was only more effective when compared to sham treatments or treatments that were considered ineffective or harmful. No clinically significant advantage was noted when compared to general practice care, analgesics, physical therapy, exercise or back school.55 Other reviews, however, have indicated that spinal manipulation may be beneficial in the first 4 weeks post injury.56, 57 A review of the evidence by the American Pain Society/American College of Physicians in 2007 suggested that there was fair evidence for small to moderate benefits from spinal manipulation.58
Two systematic reviews in 2005 of manipulation for acute neck conditions indicated scant evidence for the use of cervical manipulation.59, 60
Massage
A Cochrane review of massage for subacute (4 weeks–3months) low back pain indicated that massage may be of benefit.61
A Cochrane review of massage of mechanical neck disorders made no recommendations due to methodological considerations.62
Cold and/or heat therapies
Despite almost universal acceptance of ice as a first-line treatment to reduce swelling after acute injury, there is a surprising paucity of studies to support or refute its use, with only marginal evidence that ice plus exercise was of benefit after ankle sprains.63, 64 Moderate evidence from a small number of trials indicates that heat wraps may be of benefit during acute episodes of low back pain.65
Acupuncture
A Cochrane review (2009) of the use of acupuncture or dry needling for acute low back pain indicated insufficient evidence to make any recommendations.66 A Cochrane review in 2006 found no trials on acupuncture for acute neck pain.67 A Cochrane review of acupuncture for shoulder pain indicated the possibility of short-term benefit in pain and function, but that evidence was otherwise lacking in its efficacy.68 Acupuncture may also provide short-term relief from lateral elbow pain (tennis elbow), however, no benefit lasting greater than 24 hours has been demonstrated.69
Moreover, a systematic review investigated the effectiveness of acupuncture for non-specific low back pain70 in 23 trials (n = 6359). There was moderate evidence that acupuncture was more effective than no treatment, and strong evidence of no significant difference between acupuncture and sham acupuncture, for short-term pain relief. However, there was strong evidence that acupuncture could be a useful supplement to other forms of conventional therapy for non-specific lower back pain.
Chronic musculoskeletal pain (e.g. low back pain)
The Australian Bureau of Statistics estimated that in 2004–2005 15% of the Australian population experienced low back pain at a cost of $567 million per year.71 In fact it has been estimated that up to 70% of the community of wealthy nations will experience low back pain in their lifetime, with 2–7% of patients developing chronic low back pain (pain>12 weeks) as a result of an acute episode.72 In approximately 85% of cases a specific diagnosis for low back pain cannot be determined despite diagnostic efforts.72 Even in instances where an initial acute episode is resolved, low back pain often follows a recurrent pattern with re-exacerbations likely.73
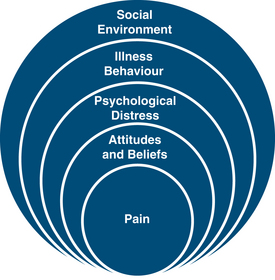
The biopsychosocial model of pain has been adopted to explain the complexities of the pain experience (Figure 27.1).74 Within this approach chronic pain is viewed as a composite response that results from the summation of biological, psychological and social factors individual to the patient’s pain ‘experience’ rather than directly correlating with tissue damage or disease. Although tissue damage may lead to nociception and a painful experience, the level of pain may be modified by many factors such as emotional response, belief structures, personal experience, cultural background, community and work environment and so forth. Alternatively in some instances tissue healing may be complete, yet pain may persist as part of a greater personal experience unique to the individual.
Hence in the context of integrative and complementary medicine the treatment of chronic low back pain may potentially involve the complete spectrum of mind–body therapies. Chronic low back pain should not be viewed solely as a musculoskeletal condition but as an experience of not only the body, but emotions, thought processes, family, social and spiritual network and, in instances of occupational injury, the work community of the patient. However, on the other hand we should not pass over the possibility of prolonged tissue damage or organic imbalance once the patient has entered the classification of chronic pain by assuming that the pain is ‘only’ psychosomatic in origin, for to do so would also risk overlooking the holism that is the individual living within the pain experience.
Lifestyle factors
Genetic
Recent studies indicate genetic influence in the development of some aspects of chronic low back pain. In twin studies related to low back pain, disc height narrowing was the factor found to correlate most with low back pain history, and further found to be genetically correlated. Other genetic correlations were found with the duration of the longest episode of back pain, hospitalisation from back pain and disability from back pain in the year previous to the study.75 Twin studies of adult women demonstrated a heritability of low back pain in adult females in the range of 52–68%, and neck pain in the range of 35–85%.76 A Danish twin study of men and women over the age of 70 indicated a genetic association with low back pain of 25% in men. However, only a modest and non-significant concordance was noted in women such that the conclusion was that genetics did not play a role in low back pain in women over 70.77
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree