Diagnostic Testing
Imaging
- Plain radiography of the cervical spine should be used judiciously in patients with nonspecific mechanical neck pain.
- Use of plain radiographs in evaluating neck pain has two important limitations:
- First, cervical spondylosis is extremely common in asymptomatic individuals and increases with age.
- Second, plain radiographs are of very limited value in assessing nerve root or spinal cord compression.
- Nonetheless, plain films should generally be done in patients with radiculopathy to evaluate for serious bony abnormalities.
- First, cervical spondylosis is extremely common in asymptomatic individuals and increases with age.
- Plain cervical spine films are warranted when a serious disorder is suspected or in cases that are related to significant trauma.
- If plain films are unrevealing but strong suspicion still exists, other imaging studies, such as computed tomography (CT) or magnetic resonance imaging (MRI), should be done.
- Use of plain radiographs in evaluating neck pain has two important limitations:
- CT or MRI is recommended when tumor, infection, fracture, or other space-occupying lesion is strongly suggested by the clinical findings or in the setting of serious neurologic signs and symptoms.
- In the absence of severe or progressive neurologic symptoms, it is generally not necessary to do a CT or MRI for patients with typical radiculopathy.
- Many patients with cervical radiculopathy have substantial improvement in a few weeks.
- If symptoms have not improved with several months of conservative management and the patient is an appropriate potential candidate for surgery, CT or MRI may be useful.
- In the absence of severe or progressive neurologic symptoms, it is generally not necessary to do a CT or MRI for patients with typical radiculopathy.
Electrodiagnostic Testing
Electrodiagnostic tests are usually not indicated in individuals with obvious radiculopathy. They are probably most useful when the cause of upper extremity pain is unclear, for example, differentiating C6 radiculopathy from median nerve entrapment, or if surgery is being considered.
TREATMENT
- Simple conservative therapy is appropriate for the majority of patients with nonspecific mechanical neck pain. In most cases, the pain improves in several weeks.
- Modest activity restriction is generally believed to be appropriate.
- Patients should avoid activities that worsen their neck pain.
- Bed rest is not indicated, and patients should be encouraged to continue most daily activities.
- Soft cervical collars are also frequently recommended and may reduce symptoms in some patients. These collars are not particularly effective at reducing neck motion but may serve as a reminder to the patient to limit movements that can increase pain. Rigid cervical collars should not be prescribed by the untrained.
- Patients should avoid activities that worsen their neck pain.
- Pharmacotherapy with acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) may provide relief for nonspecific mechanical neck pain. Opiate analgesics may be an effective time-limited option for patients with acute severe neck pain. Some patients may find muscle relaxants effective, but sedation is a common side effect. Supportive data are limited for all of these medications.2
- Neck mobilization and manipulation appear to be effective for short-term and intermediate relief.3
- Stretching and strengthening exercises of the cervical and shoulder/thoracic area may be effective for chronic mechanical neck disorders.4
- There are very limited data regarding electrotherapy and electromagnetic therapy; a definitive statement of their effectiveness is not possible.5
- Simple application of local heat or ice is an option for symptomatic relief.
- Limited evidence suggests that myofascial trigger point injections with lidocaine may be effective.2
- Acupuncture appears to be moderately effective for chronic neck pain.6
- Traction has unclear efficacy for neck pain with or without radiculopathy due to the lack of high-quality data.7
- The medical benefit of massage is unknown.8
- Surgery has no role in the relief of neck pain secondary to cervical spondylosis in the absence of significant persistent neurologic involvement.
- Whiplash does not seem to respond as well to conservative treatments, but they are frequently used, and their effectiveness is unclear.9
- For patients with chronic cervical zygapophyseal joint pain after whiplash confirmed with double-blind placebo-controlled local anesthesia, percutaneous radiofrequency neurotomy may provide lasting relief.10,11
- A small study suggests that the acute treatment with high-dose methylprednisolone may be beneficial in preventing extensive sick leave after whiplash.2,12
- For patients with chronic cervical zygapophyseal joint pain after whiplash confirmed with double-blind placebo-controlled local anesthesia, percutaneous radiofrequency neurotomy may provide lasting relief.10,11
- Neck pain with radiculopathy is generally treated in a manner similar to that of nonspecific mechanical neck pain.
- Patients with prolonged severe radicular symptoms may benefit from surgical decompression. Those who are agreeable to surgery and are medically appropriate surgical candidates can be referred to a neurosurgeon.
- Patients with persistent radicular pain secondary to cervical spondylosis may respond to fluoroscopically guided therapeutic selective nerve root block.13
- Patients with prolonged severe radicular symptoms may benefit from surgical decompression. Those who are agreeable to surgery and are medically appropriate surgical candidates can be referred to a neurosurgeon.
- Myelopathy often requires surgical treatment and is best managed in conjunction with a neurosurgeon, neurologist, or both.
Low Back Pain
GENERAL PRINCIPLES
Epidemiology
- Low back pain (LBP) is an exceedingly common complaint, with a lifetime incidence of >70%.
- Patients present along a wide spectrum of pain and disability, which unfortunately often does not correlate well with the seriousness of the underlying etiology.
- The medical and societal costs are enormous (up to $50 billion a year), with the majority due to a small percentage of patients with temporary or permanent disability.
- There is an epidemiologic association between LBP and obesity. Whether or not losing weight reduces LBP is a largely unanswered question.
- There is also an association with smoking, but true cause and effect are unknown.14–16
Etiology
- Many of the etiologies of LBP are presented in Table 34-2.17 The distribution of diagnoses varies somewhat among populations and degree of chronicity.
- Regardless, the large majority of cases are due to mechanical causes with lumbar sprain/strain accounting for the biggest proportion (about 70%).
- The pathologic corollary to sprain/strain is unknown, and the concept of skeletal muscle “spasm” is not universally accepted.
- Regardless, the large majority of cases are due to mechanical causes with lumbar sprain/strain accounting for the biggest proportion (about 70%).
- Ultimately, in approximately 85% of cases, a specific diagnosis cannot be made, so-called nonspecific musculoskeletal (or idiopathic) LBP. Medical LBP specialists and surgeons will see a higher percentage of specific pathologies.17
- Spondylosis is a generalized degenerative change of the spine, including disc degeneration, with disc space narrowing and osteoarthritic changes of the facet joints. Spondylosis is just as common in asymptomatic as in symptomatic individuals. In general, LBP patients with spondylosis have the same prognosis as those without spondylosis.
- Spondylolisthesis is the forward movement of the body of one vertebra on the vertebra below it or on the sacrum. Minor degrees of spondylolisthesis are fairly common and usually asymptomatic. Individuals with LBP that is presumed to be secondary to spondylolisthesis usually follow a similar course as those with nonspecific LBP. When the slippage is severe, it may cause back pain and radiculopathy.
- Lumbar disc herniation is common and increases with age.
- Of disc herniations, 95% occur at the L4–L5 or L5–S1 levels.
- Disc herniation may result in LBP, sciatica, or both. However, disc herniations may also be totally asymptomatic.
- Large midline disc herniations occasionally cause cauda equina syndrome.
- Of disc herniations, 95% occur at the L4–L5 or L5–S1 levels.
- Sciatica refers to a symptom of sharp, burning pain radiating from the low back or buttock and into the posterolateral aspect of lower extremity and extends below the knee. It is most commonly caused by L5 or S1 radiculopathy.
- Spinal stenosis is usually caused by hypertrophy of the ligamentum flavum and facet joints, resulting in narrowing of the spinal canal, often at multiple levels.
- This narrowing may result in entrapment of nerve roots, with resultant symptoms in the legs.
- Pseudoclaudication or neurogenic claudication is characterized by back pain and numbness of the lower extremities that worsen with walking and extension of the spine. It is relieved with spinal flexion (bending forward).
- This narrowing may result in entrapment of nerve roots, with resultant symptoms in the legs.
- Several reputed conditions are not universally accepted as valid diagnoses, including discogenic LBP, facet joint syndrome, piriformis syndrome, and sacroiliac joint dysfunction (without sacroiliitis or spondyloarthropathy).18–21 None has sufficiently distinct historical or physical findings allowing for certain diagnosis. All are reportedly substantiated by injection into the potentially pathogenic area. Gold standard tests are lacking. These diagnoses are made frequently by some clinicians and rarely or never by others. Their exact incidence and prevalence are unknown. Potentially effective and unique therapies are being investigated, but none has been clearly shown to be effective in randomized controlled trials.
- A very small number of patients have serious systemic diseases that affect the spine or have referred pain.
TABLE 34-2 Etiologies of Low Back Pain
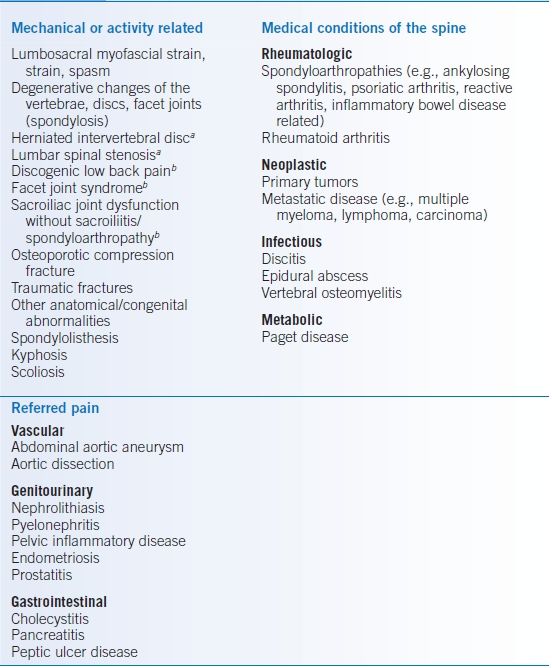
aOften associated with neurogenic leg pain.
bValidity of the diagnosis, method of precise diagnosis, and optimal unique management not universally accepted.
Data from Deyo RA, Weinstein JN. Low back pain. N Engl J Med 2001;26:153–159.
DIAGNOSIS
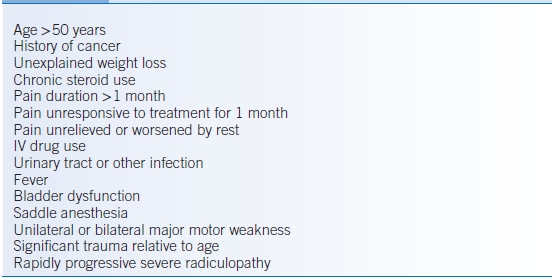
- In the vast majority of patients, the primary diagnostic tool is a careful but focused history and physical examination searching for red flags that suggest a potentially serious underlying condition or a neurologic urgency (Table 34-3).22
- In primary care, individual red flags may have a very high false-positive rate.23,24
- The red flags listed in Table 34-3 were initially described in reference to acute LBP; however, they have some validity with regard to chronic LBP as well.
- In the absence of red flags, special diagnostic tests are rarely indicated during the 1st month of pain.
TABLE 34-3 Red Flags of Low Back Pain
Clinical Presentation
History
- Symptoms and historical features potentially suggestive of malignancy include current or prior malignancies, breast or prostate masses, smoking, family history of cancer, and systemic symptoms (e.g., weight loss, night sweats, fever, and decreased appetite).
- Symptoms and historical features potentially suggestive of infection include HIV, chronic use of steroids or other immunosuppressants, history of IV drug abuse, hemodialysis, osteomyelitis/abscess, endocarditis, fever, chills, and sweats.
- Those that suggest fracture include female sex, trauma relative to age, age >70 years, and prolonged steroid use.23
- Symptoms compatible with cauda equina syndrome include bowel and/or bladder dysfunction, saddle anesthesia, bilateral lower extremity sciatica, sensory changes, and/or weakness.
- Pain worst with standing is typical of lumbar spinal stenosis, while pain worst with sitting or flexing the spine suggests disc herniation.
- Associated leg pain with standing and ambulation may represent spinal stenosis–related pseudoclaudication. True claudication generally does not occur just with standing. Some patients with spinal stenosis will have leg pain only. Flexion of the spine may improve the symptoms. The discomfort typically lasts longer after walking than it does in true vascular claudication.
- Sciatica is most specifically defined as pain radiating down the posterolateral leg below the knee. The sensitivity of the symptom of sciatica, defined as pain radiating into the buttocks and down the leg below the knee, is sufficiently high (0.95) that its absence makes a clinically significant disc herniation unlikely.25 Coughing, sneezing, and Valsalva maneuver can worsen sciatica secondary to disc herniation.
- Questions about personal or family history of spondyloarthropathies and RA may suggest these as potential causes. Morning stiffness may also provide a clue to these diagnoses.
- All patients should be asked about their occupational history, including current employment and exactly what kinds of physical activities are involved.
- There does not appear to be a relationship between leisure time sport or exercises, sitting, and prolonged standing/walking and LBP. Evidence is conflicting regarding home repair, gardening, whole-body vibration, nursing tasks, heavy physical work, and working with the trunk in a bent/twisted position.26
- Low job satisfaction and insufficient social support in the workplace are associated with the development of new-onset LBP.27
- The presence of nonorganic signs, high levels of maladaptive pain coping behaviors, high baseline functional impairment, psychiatric comorbidities, and low general health status have been shown to predict which patients with acute LBP will develop chronic LBP.28 Interventions that break the cycle of fear and avoidance might be of benefit.29
Physical Examination
- Look for fever and tachycardia as potential clues to infection or inflammatory arthropathy.
- ROM, kyphosis, scoliosis, costovertebral angle tenderness, surgical scars, and spinal/paravertebral tenderness/spasm. Unfortunately, assessments of ROM and tenderness/spasm are not particularly reproducible nor are they sensitive or specific.25
- A thorough joint exam may reveal evidence of synovitis.
- Evaluate peripheral pulses to distinguish true claudication from pseudoclaudication.
- A rectal exam may reveal prostatitis or a prostate mass.
- Decreased perianal sensation or rectal tone is worrisome for spinal neurologic involvement.
- Straight leg raise (SLR) testing may be performed with the patient supine or sitting up; it is considered positive if reproduction or worsening of sciatic pain occurs at <60 degrees. The ipsilateral SLR has a high sensitivity (0.85) and low specificity (0.52), while the contralateral (crossed) SLR has a high specificity (0.84) and low sensitivity (0.30).30
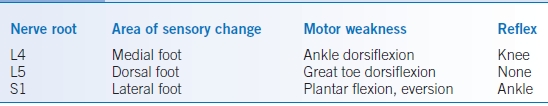
- An abbreviated neurologic examination can be done in most patients without neurologic symptoms (Table 34-4).
- When neurologic symptoms other than sciatica are present, a complete neurologic examination is warranted. Patients with the cauda equina syndrome typically have saddle anesthesia, bilateral radicular findings, and decreased anal sphincter tone.
- Often referred to as “Waddell signs” or “nonorganic signs,” the presence of three or more behavioral responses to being examined suggests that the patient does not have simply a straightforward physical problem.31 These signs, however, do not exclude organic causes or do they specifically detect secondary gain and/or malingering.32 True malingering is, in general, quite unusual.
- Superficial tenderness
- Nonanatomic tenderness
- Pain on axial loading of the skull
- Pain on passive rotation of the shoulders and pelvis
- Sitting and supine straight leg raising discrepancy
- Regional weakness
- Regional sensory change
- Inconsistent “overreaction” to examination (e.g., tremor, sweating, collapse, exaggerated verbalizing, inappropriate sighing, guarding, bracing, rubbing, insistence on standing or changing position, and questionable use of walking aids or equipment)
- Superficial tenderness
TABLE 34-4 Neurologic Examination for Sciatica
Diagnostic Testing
Assuming there are no red flags present, it is reasonable to hold off any imaging or laboratory tests for the 1st month because the majority of patients will be significantly improved during that period of time with or without intervention.
Laboratories
- The use of laboratory tests should be judicious and guided by the history and physical examination. The large majority of patients will not need any laboratory tests specifically for the purpose of elucidating the cause of LBP.
- If the history and physical examination suggest the possibility of serious diagnoses (e.g., malignancy, infection, rheumatologic, and conditions that can cause referred LBP), appropriate laboratory tests should be done.
- Some have advocated the erythrocyte sedimentation rate (ESR) as a nonspecific screening test for potentially serious and related conditions.33
Imaging
- A clinical guideline by the American College of Physicians advises against imaging in most patients with acute LBP. They stress that routine imaging has not been shown to improve clinical outcomes.
- Early imaging may be linked to worse health outcomes and increased risk of surgery.
- The radiation exposure from plain lumbar films is not inconsequential. For women, the gonadal irradiation from plain lumbar films is estimated to be equal to a plain chest film every day for several years.
- They recommend imaging in patients with severe progressive neurologic deficits or signs or symptoms of a serious disorder, for example, malignancy, infection, cauda equina syndrome, fracture, or spinal cord compression.
- For those with persistent pain and symptoms of radiculopathy or spinal stenosis, MRI (preferred) or CT should be considered only in patients who would be candidates for surgery or epidural steroid injections.34
- Early imaging may be linked to worse health outcomes and increased risk of surgery.
- Plain radiographs of the lumbosacral spine correlate poorly with the presence of LBP. Many patients without back pain have degenerative changes, and many patients with back pain will have no or nondiagnostic radiographic abnormalities.
- Degenerative changes increase with age and are extremely common in the elderly. Therefore, when degenerative changes are present, it is very difficult to know if they are causative.
- Plain films cannot detect disc herniation, spinal stenosis, or nerve root impingement and may not clearly show evidence of infection or malignancy.
- In the final analysis, plain films will often be nondiagnostic and generally do not detect abnormalities not already suggested by the history and physical examination. Nonetheless, when red flags are present, plain films are reasonable.34
- In patients with very chronic LBP, the red flag of duration of >1 month should not be interpreted as a mandate for plain films.
- Of course, clinical judgment may override these general guidelines at any time.
- One study suggests that while patients may be more “satisfied” when plain films are done, short-term pain and other clinical outcomes are not improved.35
- Degenerative changes increase with age and are extremely common in the elderly. Therefore, when degenerative changes are present, it is very difficult to know if they are causative.
- The obvious advantages of CT and MRI over plain films are much clearer delineation of bony and soft tissue abnormalities.
- Both are capable of disclosing disc herniation, spinal stenosis, nerve root and spinal cord compression, malignancy, fractures, and infection.
- On the other hand, they also detect more nondiagnostic degenerative changes.36–38
- Degenerative findings on MRI are poorly predictive of the subsequent development of LBP.39,40
- This does not mean that such findings cannot be the cause of LBP in some patients.41,42
- Both are capable of disclosing disc herniation, spinal stenosis, nerve root and spinal cord compression, malignancy, fractures, and infection.
Diagnostic Procedures
- Myelography and CT-myelography are generally only indicated in special situations for preoperative planning in consultation with a surgeon.
- Bone scintigraphy is rarely needed in the diagnostic evaluation of patients with LBP. Bone scans may have a high yield for spinal metastases in patients with a known history of cancer. However, when they are positive, other diagnostic tests are usually required (i.e., CT or MRI).
- Electrophysiologic tests are usually not indicated in individuals with obvious radiculopathy or in those with only LBP. These tests appear to be most useful in the diagnostic evaluation of patients with leg pain when the diagnosis is unclear.
TREATMENT
In the absence of red flags, treatment for most patients with acute nonspecific LBP can be simple and conservative. Most patients improve in approximately 1 month with or without treatment. Pain that has persisted without improvement for more than a month should be reevaluated. The goals of treatment are to reduce pain, increase mobility, return to functioning at home, return to work, and prevent the development of chronic pain and disability.
Medications
- Acetaminophen is a reasonable first-line choice for the treatment of acute and chronic LBP.43
- NSAIDs are more effective than placebo in patients with acute nonspecific LBP.43,44
- Tramadol (50 to 100 mg qid) is a reasonable alternative for patients who fail to respond to or who cannot take nonselective or selective NSAIDs, but side effects are common (e.g., nausea, constipation, and drowsiness).
- Muscle relaxants have been shown to be superior to placebo for acute LBP.43,45,46 The concept of muscle spasm is ill defined, and these drugs do not directly relax skeletal muscles. Their exact mechanism of action is unknown. There is insufficient evidence to suggest that one muscle relaxant is better than the others. Many patients will experience significant sedation.
- Opiates may be considered as a time-limited option for severe acute LBP. The use of opiates in chronic LBP continues to be controversial. Due to their substantial risk, experts recommend opiates for LBP only when their administration results in improved function rather than merely pain relief.47,48
- Notwithstanding, chronic LBP is a very common nonmalignant reason for prescribing chronic opioids.
- Long-term opioid use for LBP is associated with increased rates of substance abuse disorders and aberrant medication-taking behaviors.48
- Patients should be carefully screened for opioid misuse and fully informed of the risks and benefits. A written plan (pain agreement/contract) may be helpful. All patients on chronic opioid therapy should be monitored with urine drug screens. For high-risk patients, urine drug screen testing is essential to rule out use of illicit drugs and confirm adherence to the plan. Interpretation of urine drug screen testing is complex, and expert assistance is often required.
- Notwithstanding, chronic LBP is a very common nonmalignant reason for prescribing chronic opioids.
- Antidepressants may be useful in patients with chronic LBP with or without depression, though reviews have come to contradictory conclusions.43,49
- Antidepressants that inhibit the uptake of norepinephrine (tricyclics) seem to produce moderate symptomatic benefit.
- Based on limited evidence, pure selective serotonin reuptake inhibitors (SSRIs) do not appear to be effective.
- Venlafaxine and duloxetine are SSRIs that also inhibit the uptake of norepinephrine—there is limited evidence to suggest that both may be effective for other chronic pain conditions.
- Antidepressants are not indicated for the treatment of acute LBP.
- Potential risks of therapy should be carefully considered especially in the elderly.
- Antidepressants that inhibit the uptake of norepinephrine (tricyclics) seem to produce moderate symptomatic benefit.
- Anticonvulsants are increasingly being used to modulate chronic LBP. Some supportive evidence is beginning to emerge, particularly regarding topiramate and gabapentin (for sciatica).43,50,51
Other Nonpharmacologic Therapies
- Education: The overall good prognosis of acute LBP should be stressed but not oversold. Although acute LBP may rapidly and completely resolve, it certainly does not always do so, and recurrences are common. Patients should be encouraged to notify the physician if symptoms change significantly. Intensive education may reduce pain.42
- In the occupational setting, back school appears to be effective for reducing pain and improving function.53
- Bed rest may actually delay recovery and potentially contribute to the development of chronic back pain. Patients with acute nonspecific LBP should be advised to continue ordinary activities as much as possible. Patients with sciatica also should be encouraged to go about daily activities as much as tolerated.54
- Activity restriction: It is reasonable to advise the patient to limit temporarily activities that are known to increase mechanical stress on the spine, including prolonged unsupported standing, heavy lifting, and bending or twisting the back while lifting.
- Physical therapy (PT, trunk-strengthening exercises) has not been clearly shown to be beneficial in acute LBP. However, exercise therapy is somewhat effective.55,56
- Local heat or cold may be efficacious and is relatively low cost with minimal risk of side effects, particularly low-level heat wraps.57 Patients should be warned against sleeping with heating pads and placing ice in direct contact with the skin due to the potential for burns and frostbite.
- Massage might be beneficial for subacute or chronic LBP, but it can be relatively expensive.58
- Spinal manipulation (chiropractic) continues to engender controversy. Multiple reviews and meta-analyses have been published with somewhat differing conclusions. However, recent systematic reviews suggest that there is no benefit in acute LBP but may benefit chronic LBP when compared with other interventions.56,59,60 The occurrence of adverse outcomes appears to be very rare.
- Injection therapies have been tried in multiple different areas of the spine, including the facet joints, the epidural space, and soft tissue (trigger points, acupuncture points, or ligaments). Corticosteroids, local anesthetics, and saline have all been used.
- Trigger point injections are done fairly frequently. The theory of trigger points as a cause or perpetuator of LBP is controversial at best. Evidence is insufficient to recommend for or against their use in either acute or chronic LBP.61
- Facet joint injections have been advocated for the treatment of the so-called facet joint syndrome. The syndrome is diagnosed clinically in patients with lumbar pain that improves with the injection of corticosteroid or local anesthetic into or near the facet joints. The efficacy of such treatment is unclear but can be considered in selected patients with chronic LBP in whom more conservative treatment has failed.61
- Epidural steroid injections have been recommended for subacute or chronic LBP with and without sciatica. Results from multiple studies have been conflicting. Epidural steroids can be considered for patients in whom conservative therapy has failed.61
- Prolotherapy (proliferative injection therapy), the injection of an irritant solution intended to strengthen weakened lumbosacral ligaments), does not appear to be an effective sole treatment for chronic LBP.62
- The efficacy of sacroiliac joint injections is unknown.
- Trigger point injections are done fairly frequently. The theory of trigger points as a cause or perpetuator of LBP is controversial at best. Evidence is insufficient to recommend for or against their use in either acute or chronic LBP.61
- Data regarding the utility of acupuncture are contradictory, but it may be effective for those with chronic LBP.56,63,64
- Data support the use of cognitive-behavioral therapies for subacute and chronic LBP.56,65
- Multidisciplinary biopsychosocial therapy attempts to address all aspects of LBP, involving physicians, psychologists, physical/occupational therapists, and social workers. It requires the patient to take part in a substantial amount of active therapies (>100 hours) that incorporate the concept of functional restoration. Though expensive and not widely available, it has been shown to be effective for chronic LBP.66
- Lumbar supports do not appear to be useful for preventing LBP, and their role in treatment is unclear.67
- Traction as a single therapy is ineffective for LBP with or without sciatica.68
- Data do not support the use of transcutaneous electrical nerve stimulation (TENS) for LBP.69
- Data regarding therapeutic insoles are severely limited. They do not appear to prevent back pain in relatively young, highly active populations. Efficacy in treating LBP is unknown.70
- Nonsurgical spinal decompressive therapy (e.g., Vax-D) is of unproven benefit.71
- Data regarding low-level laser therapy are insufficient to draw conclusions.72
- Radiofrequency denervation may be effective for facet joint syndrome.11 Likewise, intradiscal radiofrequency thermocoagulation might be useful for discogenic LBP, but data are very limited.73
Surgical Management
- There is good evidence that surgical discectomy provides effective relief of sciatica for properly selected patients.74–76
- The primary benefit of discectomy appears to be the more rapid relief of symptoms in those individuals in whom conservative therapy has failed.
- Whether there is a significant difference in long-term outcomes is less clear.77
- The primary benefit of discectomy appears to be the more rapid relief of symptoms in those individuals in whom conservative therapy has failed.
- Similarly, surgery for appropriately selected patients with lumbar spinal stenosis is effective, but the effect diminishes over time.75,78,79 Surgical intervention for spinal stenosis with spondylolisthesis may also be effective.80
- Surgical treatment for degenerative lumbar spondylosis is especially controversial. Surgical treatments may include decompression, spinal fusion, or both. The data available are limited, sometimes of poor quality, and conflicting and often focus on technical rather than patient-centered outcomes. A 2009 review concluded that for nonradicular back pain associated with degenerative changes, spinal fusion is no more effective than intensive rehabilitation but more beneficial compared with standard nonsurgical therapies.75 A 2013 review was more optimistic about the effects of fusion surgery for patients with disc degeneration.81 Regardless, for the large majority, surgical intervention for nonspecific mechanical back should only be considered for those with prolonged pain who have failed all more conservative interventions and who are appropriate medical candidates.
Shoulder Pain
GENERAL PRINCIPLES
- The glenohumeral (GH) joint is very shallow and is the most commonly dislocated joint.
- The rotator cuff supports the GH joint and consists of the tendons of four muscles: supraspinatus, infraspinatus, teres minor, and subscapularis.
- The tendons of these muscles blend with the shoulder joint capsule and insert on the greater and lesser tuberosities of the humeral head.
- The rotator cuff muscles assist in internal and external rotation and depress the humeral head during shoulder elevation.
- This action holds the humeral head down, minimizing impingement on the acromion process and the intervening tissues.
- The tendons of these muscles blend with the shoulder joint capsule and insert on the greater and lesser tuberosities of the humeral head.
- The subacromial bursa lies deep to the deltoid muscle and superficial to the insertion point of the supraspinatus tendon. This bursa protects the rotator cuff from the acromion.
- The long head of the biceps originates from the glenoid labrum. The biceps tendon emerges from the GH joint through the bicipital groove.
- Patients with acute shoulder problems have a better prognosis than those with chronic shoulder pain.82
- The shoulder impingement syndrome causes the majority of painful nontraumatic shoulder problems. It is due to mechanical impingement of the rotator cuff structures by the humeral head against the subacromial structures. This is related to a continuum of inflammation, degeneration, and attrition of the rotator cuff structures, especially the supraspinatus tendon. As a result, the rotator cuff fails to prevent upward migration of the humeral head during shoulder elevation. Several interrelated conditions are involved in the impingement syndrome; all may occur simultaneously.
- Rotator cuff tendonitis refers to a spectrum of changes that affect the tendons of the rotator cuff, particularly the supraspinatus. Acute inflammation with hemorrhage and edema can occur secondary to trauma or overuse, particularly in younger patients. Acute rotator cuff tendonitis is sometimes associated with calcification of the supraspinatus and biceps tendons (so-called calcific tendonitis). The pain of calcific tendonitis can be severe and may lead to a frozen shoulder. With aging, the tendons undergo degenerative changes and attenuation related to chronic inflammation and repeated mechanical insults.83
- Rotator cuff tears can occur suddenly secondary to falling on an outstretched arm or with lifting a heavy object. Tears can also occur more indolently in older patients with attrition of the rotator cuff or with a chronic inflammatory condition such as RA or the Milwaukee shoulder (progressive, destructive shoulder arthropathy associated with bloody shoulder effusions and the deposition of hydroxyapatite crystals).
- Subacromial bursitis and bicipital tendonitis may accompany rotator cuff tendonitis. In fact, it is often difficult to distinguish these entities, as they frequently occur simultaneously. Occasionally, the proximal biceps tendon ruptures.
- Rotator cuff tendonitis refers to a spectrum of changes that affect the tendons of the rotator cuff, particularly the supraspinatus. Acute inflammation with hemorrhage and edema can occur secondary to trauma or overuse, particularly in younger patients. Acute rotator cuff tendonitis is sometimes associated with calcification of the supraspinatus and biceps tendons (so-called calcific tendonitis). The pain of calcific tendonitis can be severe and may lead to a frozen shoulder. With aging, the tendons undergo degenerative changes and attenuation related to chronic inflammation and repeated mechanical insults.83
- Adhesive capsulitis (frozen shoulder) may complicate any painful shoulder condition and has been associated with myocardial infarction, diabetes mellitus, apical lung cancer, cervical disc disease, metastatic lesions, and thyroid disease. However, such clinical associations are often lacking. The precise pathophysiology of adhesive capsulitis is not entirely clear but appears to involve initial hypervascular synovitis and subsequent fibrosis. What triggers this process is unknown.84 It is not unusual for frozen shoulder to develop subsequently in the contralateral shoulder.
- Osteoarthritis does not commonly occur as a primary process in the GH joint, with two exceptions: (a) rapidly progressive osteoarthritis of the shoulder in elderly women and (b) the Milwaukee shoulder. Secondary osteoarthritis may occur as a result of RA, trauma, repetitive manual labor, calcium pyrophosphate deposition disease, and long-standing rotator cuff tears (cuff tear/rotator arthropathy).
- Shoulder instability and dislocation: The shoulder joint is inherently unstable and the most commonly dislocated joint. Acute GH dislocation occurs most frequently in young active adults after a fall on an outstretched arm and results in anterior displacement of the humeral head. Recurrent dislocation is not unusual, with subsequent episodes requiring less force. Some patients have a chronic syndrome of GH instability with subluxation. This is often seen in athletes such as baseball pitchers.
- Inflammatory arthropathies such as RA and lupus can affect the GH joint.
- Crystalline arthropathies occasionally occur in the shoulder, such as the above-mentioned Milwaukee shoulder (hydroxyapatite crystals) and pseudogout/pyrophosphate arthropathy (calcium pyrophosphate dihydrate crystals). Gout is relatively rare.
- The acromioclavicular joint can also be painful due to sprain/separation and arthritic changes.
- Referred pain from the chest, abdomen, and cervical spine or from myocardial ischemia should be considered. With referred pain, intrinsic shoulder movement is not painful. Aching pain over the superior shoulder that involves the lateral upper arm or the medial border of the scapula is likely from C5 cervical radiculopathy.
DIAGNOSIS
Clinical Presentation
History
- Intrinsic shoulder pain is typically worse at night and aggravated by lying on the affected shoulder.
- Motion of the shoulder generally increases the discomfort, particularly full forward-flexed elevation and abduction to 90 degrees.
- A history of recent trauma, new physical activity, and prior dislocation are important.
- Patients with shoulder instability may complain that the shoulder has a disconcerting “going out” sensation.
- Referred pain tends to be poorly localized.
- Impingement syndrome patients may have a history of repetitive overhead arm motion. Pain tends to be focal and anterior, occurring at night or when the patient is lying on the shoulder. Activities such as throwing, working with arms overhead, and swimming aggravate the pain.
- Adhesive capsulitis is most common in women in the fifth and sixth decades of life. The key historical feature is a painful and significant reduction in ROM. The onset can be fairly acute or chronic. As the condition progresses, pain subsides, but the limitation of ROM may become quite severe. After months of symptoms, some patients have a slow progressive improvement in ROM.
- Individuals with GH instability complain of a chronic feeling of the shoulder “going out” with certain activities and sometimes pain. A history of significant trauma (usually related to sports) and pain is elicited from patients with acute GH dislocation and acromioclavicular separation.
Physical Examination
- Physical examination of the shoulder should include observation, palpation of the bony and soft tissues, assessment of passive and active ROM, strength testing, and certain provocative tests.
- Normal abduction of the internally rotated (palm down) shoulder is approximately 120 degrees and externally rotated (palm up) shoulder is 180 degrees.
- Normal elevation (forward flexion) of the shoulder is 180 degrees, extension 40 degrees, and internal and external rotation 90 degrees.
- If active ROM is limited, passive ROM should be carefully tested.
- Marked loss of both active and passive ROM is consistent with adhesive capsulitis.
- Crepitus during ROM may be appreciated with osteoarthritis.
- There are many named physical exam tests for the shoulder. The evidence that any one test is pathognomonic for a condition is poor.85
- Cross-chest abduction (touch the opposite shoulder) tests internal rotation and adduction.
- The Apley scratch test evaluates external rotation and abduction from above (scratch between the scapulae from above) or internal rotation and adduction from below.
- Patients with acute anterior dislocation have a loss of the shoulder’s normally rounded appearance. The acromion process becomes the most lateral structure. A prominence of the humeral head is present anterior and inferior to the glenoid. ROM is painfully restricted. Patients with acute dislocation should have a detailed neurovascular examination, specifically the motor and sensory innervation of the axillary nerve.
- The impingement sign is elicited by passive forward flexion of the arm by the physician. Passive abduction to 90 degrees with internal rotation also causes pain. Painful arc sign is present when pain is elicited with between 80 and 120 degrees during abduction. Both suggest subacromial bursitis or rotator cuff tendonitis.
- The apprehension sign is elicited by having the patient place their arm in the throwing position. The examiner places one hand over the posterior shoulder and exerts pressure onto the wrist. The patient’s apprehension is evident when shoulder instability is present.
- Neer impingement sign: With the patient in the seated position, elbow extended, and forearm pronated (humerus internally rotated), passively elevate (forward flex) the GH joint with the examiner’s hand distal to the elbow while the other stabilizes the posterior aspect of the shoulder. Pain indicates a positive sign, especially near the end of the ROM. Sensitivity and specificity are estimated to be 0.72 and 0.60, respectively.85
- Hawkins impingement sign: With patient sitting or standing, grasp the arm at the elbow and wrist, flex the elbow and shoulder to 90 degrees, then passively internally rotate the shoulder. Pain, particularly at the end of the ROM, is a positive test—sensitivity 0.80 and specificity 0.56.83
- Yocum test consists of having the patient place the palm on the affected side on the opposite shoulder and then to raise the elbow without elevating the shoulder. Pain is indicative of impingement—sensitivity 0.79 and specificity 0.40.86
- The drop arm sign to demonstrate a rotator cuff tear is performed by assisting the patient in abducting and elevating the shoulder. When the examiner withdraws support of the upper arm, the patient is unable to hold the arm up if there is a complete tear of the rotator cuff.
- The lift-off test tests specifically for weakness of the subscapularis. The patient places the hand of the affected side on the small of the back, with the palm oriented posteriorly, and pushes against resistance. Normally, the patient should be able to push the examiner’s hand away from the back.
- Anterior instability is most common and is suggested by pain with the anterior apprehension test.
- With the patient supine, the shoulder is initially at 90 degrees of abduction and neutral rotation, and the arm is externally rotated (as in a throwing position). The examiner places one hand under the shoulder and applies pressure backward against the wrist.
- The patient’s discomfort is apparent through verbal and nonverbal cues.
- The relocation test is performed immediately after the apprehension test. The examiner moves his or her hand from behind the shoulder to the front and applies pressure. Improvement in pain or impending dislocation is a positive test.
- Impingement produces an apprehension sign, but it is not significantly altered by relocation.
- With the patient supine, the shoulder is initially at 90 degrees of abduction and neutral rotation, and the arm is externally rotated (as in a throwing position). The examiner places one hand under the shoulder and applies pressure backward against the wrist.
- The posterior apprehension test is performed by having the patient flex the elbow and elevate the internally rotated shoulder to 90 degrees (hand on opposite shoulder). The examiner pushes backward onto the elbow, and apprehension is apparent.
- Yergason sign produces pain and tenderness over the bicipital groove with resisted supination of the forearm while the elbow is flexed and held at the side. Passive extension of the shoulder may also reproduce the pain of bicipital tendonitis.
- Speed test is thought to identify tendonitis/inflammation of the biceps tendon-superior labral complex. The patient flexes the shoulder at 30 degrees against resistance with the elbow extended and the forearm supinated. Pain is noted along the long head of the biceps brachii tendon. Estimated sensitivity and specificity for superior labral tears are 0.20 and 0.78, respectively.85
- Rupture of the biceps tendon is evident as the Popeye sign, a mass of contracted muscle midway between the shoulder and the elbow.
Diagnostic Testing
- In many cases, using a combination of history and specific examination tests will allow reasonable diagnostic accuracy. For example, for patients with a painful shoulder, the following three criteria help diagnose supraspinatus tendinopathy: age >39, painful arc sign, and self-report of popping or clicking. When 2 of 3 are present, the sensitivity and specificity are 0.75 and 0.81. When all three are present, the sensitivity and specificity are 0.38 and 0.99.85
- Plain radiographs are not necessary or appropriate in the initial evaluation of every patient with shoulder pain, especially if the history and physical examination suggest impingement.
- In patients with no history of a fall or a shoulder deformity, plain radiographs are very unlikely to provide any useful information.
- Anteroposterior (AP) views of the GH joint in internal and external rotation and an axillary view are typically done.
- Arthritis of the GH and acromioclavicular joints and calcification of the rotator cuff tendons can be visualized. Osteoarthritis is indicated by joint space narrowing and, in more advanced cases, flattening of the humeral head, subchondral cysts, and marginal osteophytes.
- Detection of shoulder dislocation may require special views.
- Plain films should be obtained in patients who do not appear to be responding to conservative treatment for impingement syndrome. The primary value of a radiograph in this situation is to assess the degree of impingement, based on the vertical distance between the inferior aspect of the acromion and the superior aspect of the humeral head. Normally, the width of a ballpoint pen should fit in between the acromion and the humeral head. Narrowing of this space suggests that the patient has chronic rotator cuff disease, in which case conservative treatment may be inadequate.
- Diffuse osteopenia is sometimes seen with adhesive capsulitis.
- In patients with no history of a fall or a shoulder deformity, plain radiographs are very unlikely to provide any useful information.
- MRI, or, in some centers, a diagnostic ultrasound, can assess the degree of supraspinatus tendon pathology. If the tendon is significantly narrowed or partially or completely torn, the patient should be referred to an orthopedist who is experienced in shoulder surgery.
TREATMENT
Impingement Syndrome
- Treatment goals are to reduce pain and improve shoulder function and ROM.
- The optimal management of impingement syndrome is unclear. However, in older patients with chronic shoulder pain, no history of an injury, and findings consistent with impingement syndrome, a trial of PT is reasonable. Imaging prior to PT for chronic shoulder pain is not necessary.
- Methodologically strong trials are limited and, therefore, it is difficult to provide evidence-based recommendations.
- The individual entities can be difficult to distinguish clinically, often coexist, and can overlap with other shoulder disorders. They are usually self-limited, and conservative treatments are generally sufficient. Some cases, however, are resistant to treatment, and recurrences can occur.
- Relative rest of the shoulder is reasonable. Patients should avoid activities and movements that aggravate the pain but must not stop moving the shoulder all together.
- Gentle ROM exercises are usually recommended to maintain ROM and avoid adhesive capsulitis. Pendulum exercises are easy for patients to do at home and consist of flexing at the waist 90 degrees, supporting the upper body on a low table, and loosely swinging the arm like a pendulum against gravity. The arc of movement is slowly increased over time.
- Referral to PT for careful strengthening of the shoulder muscles may be beneficial.87
- Evidence is insufficient to clearly support the use of physiotherapy modalities (e.g., ultrasound, laser, heat, cold, manipulation, and electrotherapy).87
- Application of heat or ice may be comforting.
- NSAIDs are probably effective for the pain of impingement syndrome.
- Local corticosteroid injections (subacromial bursa and rotator cuff region) may have a temporary benefit for adhesive capsulitis, rotator cuff disease, and subacromial bursitis, but evidence is limited.88–91 Triamcinolone acetonide 40 mg is a typical dose for a larger joint. Repeated injections should be avoided. Potential complications of steroid injections include infections, skin atrophy, and tendon weakening and rupture. Steroid injections may be inadvisable for patients with more than small rotator cuff tears.
- Referral to an orthopedist who is experienced in shoulder surgery is appropriate for patients who would consider surgery and who have prolonged pain and limitation of function. Early referral should be considered for all patients with moderate-to-large rotator cuff tears.
Other Conditions
- Treatment for adhesive capsulitis is generally noninvasive including PT and NSAIDs.
- Many patients will have resolution over 1 to 2 years.
- Corticosteroid injections directly into the GH joint (usually done under fluoroscopy) may be of some benefit, particularly early in the course. Oral steroids may also provide short-term relief (<6 weeks).92
- Arthroscopic capsular release is sometimes recommended for recalcitrant cases.
- Many patients will have resolution over 1 to 2 years.
- Osteoarthritis treatment is also generally conservative, including NSAIDs and PT. Patients with advanced cases may require a total shoulder arthroplasty for pain relief.
- Treatment of acute shoulder dislocation is best handled by immediate orthopedic consultation.
- Patients with chronic GH instability are treated conservatively with a program of PT and avoiding activities that provoke subluxation. Surgery may be indicated for some young patients and for those with continued intolerable symptoms.
Elbow Pain
GENERAL PRINCIPLES
- Elbow pain is a fairly common complaint in the ambulatory setting. In general, only one of a few conditions is causative.
- Lateral epicondylitis or tendinosis (tennis elbow) is the most common cause of elbow pain. The condition is caused by chronic overuse of the wrist extensors and supinators that originate from the lateral epicondyle. This results in repetitive microtears and angiofibroblastic degeneration or tendinosis of the origins of these muscles. No significant degree of inflammatory reaction appears to occur.93
- Medial epicondylitis or tendinosis (golfer’s elbow) is very similar to but less common than lateral epicondylitis. It involves overuse and degenerative changes of the tendinous origins of the wrist flexor/pronator muscles at the medial epicondyle.
- Ulnar nerve entrapment (cubital tunnel syndrome) results from compression of the ulnar nerve as it passes behind the medial epicondyle through the cubital tunnel, where it is very superficial. Direct pressure, repetitive elbow bending, prolonged elbow flexion, elbow arthritis, diabetes, and certain occupations and activities have all been associated with the condition. A firm direct blow to this area produces the familiar “funny bone” sensation.
- Olecranon bursitis (student’s elbow) is a common condition that results from acute inflammation of the olecranon bursa. This bursa does not connect with the synovial cavity of the elbow. The cause may be infectious or noninfectious. The most common infectious agent is Staphylococcus aureus. Common noninfectious causes include repetitive trauma, gout, pseudogout, and RA. It can be difficult to differentiate an infectious from a noninfectious inflammatory bursitis.
DIAGNOSIS
Clinical Presentation
History
- Patients usually complain of pain but may also report stiffness or swelling, or both.
- A history of acute trauma is important and may suggest fracture, dislocation, or tendon rupture.
- Repetitive overuse is a major cause of elbow pain, and patients should be asked about recreational and occupational activities.
- The specific location of the pain may be the key to proper diagnosis.
- Patients with lateral epicondylitis complain of lateral elbow pain that worsens with certain activities, usually related to sports (e.g., racquet sports) or other repetitive uses that involve wrist extension and power gripping (e.g., carpentry or lifting with the palm facing down). Tenderness may extend to the proximal lateral forearm. Symptoms may develop acutely or more slowly. A direct blow to the outside of the elbow can also trigger lateral epicondylitis.
- Patients with medical epicondylitis also complain of pain and tenderness but over the medial epicondyle that is worsened by certain activities. It too is often related to sports (golf and throwing activities) and work.
- A history of weakness and sensory changes should also be sought.
- With ulnar nerve entrapment, patients complain of medial elbow pain and sensory changes (numbness and paresthesias) in the ulnar nerve distribution, particularly the fourth and fifth digits. The symptoms may be worse at night. Weakness is sometimes reported.
- Olecranon bursitis typically presents with tender painful swelling of the posterior elbow that may develop acutely or more slowly. A history of trauma should be sought.
Physical Examination
- The elbow examination should include inspection, palpation, ROM, and neurologic assessment.
- The point of maximal tenderness should be determined if possible.
- The normal range of extension and flexion is 0 to 140 degrees. Normal supination and pronation are 80 degrees each way.
- The neck, shoulder, and wrist should be examined to evaluate for referred pain.
- With lateral epicondylitis, the diagnostic maneuver involves shaking hands on the affected side, cupping the patients elbow with your other hand, and moving your thumb over and just anterior to the lateral epicondyle. Reproducible pain at this site while the patient resists the shaking hand from supinating confirms the diagnosis.
- With medial epicondylitis, the tenderness expectedly increases over the medial epicondyle. The pain may be reproduced by resisted wrist flexion.
- Ulnar entrapment findings include sensory changes and weakness in the ulnar nerve distribution. Light touch and pinprick sensation are decreased in the ring and little fingers. Tapping the ulnar nerve where it passes behind the medial epicondyle causes pain along the inner elbow and paresthesias in the fourth and fifth digits (Tinel sign). Full elbow flexion can produce a similar result (elbow flexion test). Weakness in the abductor digiti minimi, which is innervated only by the ulnar nerve, may be seen. Testing is performed by having the patient place the palm on a desktop and moving the fifth digit across the desktop while the examiner applies resistance to this digit. Reduced grip strength and intrinsic hand muscle weakness may be present. With prolonged nerve compression, atrophy of the intrinsic muscles may be seen.
- With bursitis, the exam is most notable for an obvious swelling (goose egg) of the olecranon bursa, which may be quite large. Infectious and noninfectious causes may be indistinguishable on examination. Both can present with erythema, tenderness, and warmth. Marked findings are more likely to be traumatic or infectious in origin. Chronic or recurrent bursitis may be nontender.
Diagnostic Testing
- Plain radiographs of the elbow typically include the AP and lateral views.
- In many cases, plain films are nondiagnostic (e.g., lateral and medial epicondylitis).
- They should probably be done in all patients with significant acute trauma to evaluate for dislocation and fracture.
- With ulnar nerve entrapment, they are generally unnecessary unless a bony abnormality causing nerve compression is suspected.
- Special views are sometimes taken to evaluate the olecranon fossa and radial head.
- In many cases, plain films are nondiagnostic (e.g., lateral and medial epicondylitis).
- CT and MRI are occasionally indicated for better delineation of the bony and soft tissues.
- Nerve conduction studies and electromyography may be useful when the diagnosis of ulnar nerve entrapment is uncertain or surgery is being considered.
- When the olecranon bursa is acutely swollen, aspiration of the bursal fluid should be done to evaluate for infection. The fluid should be sent for Gram stain, culture, cell count, and crystal examination. Synovial fluid cell counts in infectious bursitis are generally lower (several thousand cells/mL) than in septic arthritis. The bursal fluid may be obviously bloody in cases of trauma.
TREATMENT
- Treatment of lateral epicondylitis is usually conservative.
- Relative rest (i.e., initially avoiding the activities that cause pain) is appropriate.
- Topical NSAIDs provide relief in the short term, while there is insufficient evidence to make recommendations for or against oral NSAIDs.94
- A compressive strap worn just below the elbow (tennis elbow splint) might be useful, but data are contradictory.95
- Some patients find local application of ice comforting.
- Proper racquet size and backhand technique may also be of value.
- Local corticosteroid injection (e.g., 40 mg triamcinolone) is an often-recommended alternative for patients who fail to respond to simple measures. It is generally believed to be effective, at least in the short term.91
- Multiple other treatments are available, but their effectiveness is uncertain.95
- Surgery is rarely necessary.
- Relative rest (i.e., initially avoiding the activities that cause pain) is appropriate.
- Treatment of medial epicondylitis is similar to that of lateral epicondylitis. Local corticosteroid injection may be effective in the short term for those who do not respond to more conservative therapy, but due to the proximity of the nerve and artery, this is usually performed by an orthopedic surgeon.
- Treatment of ulnar nerve entrapment is also usually conservative.
- The elbow should be kept straight as much as possible. A splint can be worn at night to prevent flexion of the elbow during sleep.
- If possible, the patient’s work environment should be altered to prevent further compression. A cushioning elbow pad can be worn to protect the nerve during work.
- A trial of NSAIDs is reasonable for pain.
- Surgery may be necessary for patients with recalcitrant symptoms.
- The elbow should be kept straight as much as possible. A splint can be worn at night to prevent flexion of the elbow during sleep.
- Aspiration of the olecranon bursa is not only diagnostic but also therapeutic for olecranon bursitis.
- Fluid reaccumulation is not unusual in noninfectious cases, and repeat aspiration may be necessary. A compression dressing can be applied to help prevent recurrence, and an elbow pad can be used to prevent trauma.
- NSAIDs are frequently given.
- Injection of 20 mg methylprednisolone into the bursa may also reduce recurrence in patients with nonseptic olecranon bursitis.96 Corticosteroid injection is contraindicated in infectious bursitis.
- Empiric antibiotic treatment (e.g., dicloxacillin or a cephalosporin) should be given when infection is suspected with pending culture results. Daily aspiration is usually necessary for septic bursitis.
- Fluid reaccumulation is not unusual in noninfectious cases, and repeat aspiration may be necessary. A compression dressing can be applied to help prevent recurrence, and an elbow pad can be used to prevent trauma.
Wrist and Hand Pain
GENERAL PRINCIPLES
- Wrist and hand complaints are common in primary care. Because of their obvious functional importance, careful diagnosis and treatment are particularly important.
- Stenosing tenosynovitis is an inflammation and thickening of tendons, sheaths, and synovium in the hand, sometimes with nodular enlargement of the tendon. It is frequently related to repetitive overuse, particularly those activities that involve gripping.
- Trigger finger or thumb is caused by stenosing tenosynovitis of the flexor tendons of the fingers and thumb.
- de Quervain tenosynovitis is a very similar condition that affects the tendons and sheaths of the abductor pollicis longus and the extensor pollicis brevis.
- Dupuytren contracture is a fibroproliferative disorder that results in painless thickening and nodularity of the palmar aponeurosis. The flexor tendons of the hand are not primarily involved. The fibrosis of the palmar fascia draws the fingers (most commonly the ring and little finger) into flexion at the metacarpophalangeal (MCP) joint. The condition generally affects men >40 years and appears to have a strong genetic component. It is also associated with diabetes, alcoholism, repetitive trauma, and seizure disorders.
- de Quervain tenosynovitis is a very similar condition that affects the tendons and sheaths of the abductor pollicis longus and the extensor pollicis brevis.
- Carpal tunnel syndrome (CTS) is the most frequently occurring entrapment neuropathy.
- It results from compression of the median nerve as it passes through the carpal tunnel.
- It is most common in middle-aged women and usually affects the dominant hand.
- CTS is known to occur with increased frequency in patients with diabetes, amyloidosis, renal failure on hemodialysis, RA and other arthropathies of the wrist, acromegaly, pregnancy, hypothyroidism, and previous wrist trauma. It is often related to repetitive overuse of the hands and wrists.
- It results from compression of the median nerve as it passes through the carpal tunnel.
- Ulnar nerve entrapment can occasionally occur at the wrist as the nerve passes through the canal of Guyon. It may be caused by repetitive trauma (e.g., operating a jackhammer, using the hand as a hammer, and resting the ulnar side of the wrist and hand on the edge of a desk or keyboard) or a space-occupying lesion (e.g., ganglion or lipoma).
- Arthritic conditions of the wrist and hand are common. RA characteristically involves the wrist, MCP, and proximal interphalangeal joints. The erosive synovitis causes pain, stiffness, deformity, and loss of functionality. Osteoarthritis typically involves the distal interphalangeal and carpometacarpal joints (especially of the thumb). See Chapter 33 for a full discussion of the management of these conditions.
- Infectious causes of hand/finger pain include paronychia and felons. The latter are a more serious infection of the entire distal pulp of the fingertip. The most common organism is S. aureus. They are generally caused by a puncture wound to the thumb or index finger.
- Subungual hematoma is a very common traumatic cause of finger pain.
DIAGNOSIS
Clinical Presentation
History
- With trigger finger/thumb, digit extension is limited when the affected tendon catches on the pulley at the base of the digit. This results in pain with use, and the affected digit can become painfully stuck in flexion. The finger may need to be forcibly extended with the other hand, often with a painful and audible pop.
- Patients with de Quervain tenosynovitis complain of pain, tenderness, and swelling on the radial side of the wrist just proximal to the wrist crease in the region of the anatomic snuffbox. Ulnar deviation of the wrist and movement of the thumb exacerbate the pain, and a squeaking or creaking sensation may be described. Onset is often after overuse of the wrist and thumb (e.g., prolonged writing or carrying an infant car seat).
- Affected patients with Dupuytren contracture complain of painless nodules in the palm, an inability to extend the fingers fully, and difficulty in picking up large objects.
- Patients with CTS usually complain of an aching pain in the wrist and hand, which may radiate up the forearm. Intermittent paresthesias and numbness in the median nerve distribution (palmar surface of the thumb, index, long, and radial side of the ring fingers) are typical.
- Less-than-classic descriptions of the location of discomfort are not unusual.
- Symptoms are frequently worse at night and with overuse of the hands.
- The patient may describe shaking out the hand to improve the symptoms (the flick sign). The sensitivity and specificity are low, however.97
- Weakness, clumsiness, and a tendency to drop objects may also be reported.
- Patients should be questioned about trauma, work-related duties, hobbies, and activities.
- Less-than-classic descriptions of the location of discomfort are not unusual.
Physical Examination
- Palpation at the distal palmar crease in trigger finger may reveal a thickened tendon sheath or a tender nodule, or both, usually overlying the MCP joint of the affected finger.
- Finkelstein sign is diagnostic for de Quervain tenosynovitis. The patient makes a fist enclosing the thumb; if this does not produce pain, the examiner forces the wrist into ulnar deviation as an additional stress. Focal tenderness is usually present over the radial styloid.
- With Dupuytren contracture, examination reveals painless thickening and nodularity of the palmar fascia with flexion deformity of one or more fingers.
- In CTS, the examination classically reveals decreased sensation (hypalgesia) in the median nerve distribution, weakness of thumb abduction, and Tinel and Phalen signs.
- In the Phalen maneuver, the wrists are held in unforced flexion for 30 to 60 seconds. Reproduction or worsening of the symptoms constitutes a positive sign.
- Tinel sign is the development of paresthesias in the median nerve distribution when the median nerve is tapped at the distal wrist crease.
- When compared with electrodiagnostic testing, however, Tinel and Phalen signs may have limited diagnostic value.98
- Thenar atrophy can occur with long-standing CTS.
- In the Phalen maneuver, the wrists are held in unforced flexion for 30 to 60 seconds. Reproduction or worsening of the symptoms constitutes a positive sign.
Diagnostic Testing
- Radiographs of the hands and wrists may provide diagnostic information, particularly if arthritis is suspected.
- However, definitive changes may not be apparent until the disease has been present for an extended period of time.
- In cases of significant trauma, plain films are usually mandatory.
- However, definitive changes may not be apparent until the disease has been present for an extended period of time.
- Electrodiagnostic testing (median nerve conduction) is generally thought to be the gold standard for CTS, but false positives and false negatives do occur. Such testing should be considered only when the diagnosis is uncertain or surgical treatment is being considered or in cases of work-related injury compensation.
TREATMENT
- Treatment of trigger finger initially consists of splitting the MCP joint in extension and a short course of NSAIDs. Corticosteroid injection (methylprednisolone, 15 to 20 mg) with lidocaine into the flexor digital tendon sheath can also be effective.99 Recurrence is common, and surgical release may be required.
- de Quervain tenosynovitis is treated with a short opponens splint, supplemented by NSAIDs. Refractory cases may respond to corticosteroid injection (methylprednisolone, 20 to 30 mg) with lidocaine.100 Surgical release is sometimes required.
- Apart from gently stretching the fingers, there is no known effective conservative treatment for Dupuytren contracture. Surgical treatment can be considered for the severely affected, but recurrences are common.
- Treatment for CTS is likewise initially conservative.
- There is very limited evidence to support benefits of wrist splint (worn primarily at night), exercise and mobilization, and ultrasound therapy.101–103
- Work-related ergonomic modifications should be undertaken if necessary.
- If these simple measures fail, the patient can be referred for a single corticosteroid injection (40 mg triamcinolone) with lidocaine (10 mg) into the area close to the carpal tunnel, which may be effective for up to 4 weeks.104
- Definitive treatment entails surgical release, a simple outpatient procedure in which the flexor retinaculum is incised, relieving the pressure on the median nerve. Surgery is very effective in treating CTS, provided that the diagnosis has been confirmed electrodiagnostically and is more effective than splinting.105
- There is very limited evidence to support benefits of wrist splint (worn primarily at night), exercise and mobilization, and ultrasound therapy.101–103
Hip Pain
GENERAL PRINCIPLES
- Hip pain has many potential causes, but only a few are common.
- Pain may emanate from the hip joint, periarticular soft tissues, pelvic bones, and sacroiliac joint or be referred from another location (usually the lumbosacral spine).
- Osteoarthritis of the hip joint is very common and increases with age. It is characterized by loss of the articular cartilage of the joint. Predisposing factors include childhood hip disorders, leg-length anomalies, and work that involves heavy lifting and carrying. The diagnosis and treatment of osteoarthritis are discussed in Chapter 33.
- Trochanteric bursitis is another common cause of hip pain. It can occur in association with iliotibial band syndrome, hip joint pathology, previous hip surgery, leg-length discrepancy, and mechanical back pain.
- Avascular necrosis (osteonecrosis, AVN) is the death of a variable amount of trabecular bone in the femoral head.
- The precise pathophysiology is not known, but it is unusual in the absence of known risk factors, which include corticosteroid treatment (especially in those with lupus), alcoholism, trauma or prior fracture, RA, HIV infection, sickle cell disease, myeloproliferative disorders, and radiation.
- A high index of suspicion should be maintained in patients with these risk factors. The condition may be bilateral.
- Severe AVN can cause collapse of the femoral head.
- The precise pathophysiology is not known, but it is unusual in the absence of known risk factors, which include corticosteroid treatment (especially in those with lupus), alcoholism, trauma or prior fracture, RA, HIV infection, sickle cell disease, myeloproliferative disorders, and radiation.
- Meralgia paresthetica is an entrapment neuropathy caused by compression of the lateral femoral cutaneous nerve. It may be related to one or more factors, including obesity, pregnancy, diabetes, wearing tight garments around the waist (e.g., pantyhose, tool belts), local surgery, trauma, repetitive hip extension (joggers, cheerleaders who do splits frequently) and, rarely, intrapelvic masses.
- Hip fractures are particularly common in elderly women and usually occur at the femoral neck or the intertrochanteric area. They are associated with a high morbidity and mortality. Age, Caucasian race, female sex, osteoporosis, and falls are common predisposing factors.
DIAGNOSIS
Clinical Presentation
History
- Patients typically complain of painful limited ROM and difficulty ambulating.
- The location of the pain can be the key to proper diagnosis.
- True hip joint pain usually affects the groin and radiates to the buttock. Bearing weight worsens the pain.
- Buttock pain alone without groin pain is likely to originate in the low back, sacroiliac joint, or ischial tuberosity.
- Lateral proximal thigh pain suggests trochanteric bursitis.
- Anterolateral thigh pain suggests either lateral femoral cutaneous nerve entrapment or sciatica.
- Pain that radiates down the posterior thigh is frequently due to lumbosacral radiculopathy.
- True hip joint pain usually affects the groin and radiates to the buttock. Bearing weight worsens the pain.
- Patients with chronic progressive disease have increasing difficulty in ambulating and performing the activities of daily living.
- Patients with trochanteric bursitis complain of lateral hip pain that may radiate down the leg. The pain is worse with exercise and at night, especially when the patient lies on the affected side. Some patients complain of a limp.
- AVN pain tends to come on suddenly and can be severe, but the onset can be more gradual. A few patients may be asymptomatic. The pain is typically in the groin radiating to the buttocks and is increased with weight bearing.
- Meralgia paresthetica is remarkable for pain, burning, and dysesthesia in the groin and anterolateral thigh. The discomfort may extend to the lateral knee. No motor symptoms occur.
- Most patients with hip fracture report a fall and subsequent inability to walk. They have pain in the groin that radiates to the buttocks. A few patients may be able to walk with assistance, but pain increases with weight bearing.
Physical Examination
- The patient should be observed standing and walking. A limp or expression of pain may be demonstrative of the patient’s complaint.
- The abductor lurch (Trendelenburg gait) suggests intra-articular hip pathology. The patient shifts weight over the affected leg to unload weakened abductors.
- The Trendelenburg test should be done. Ask the standing patient to raise the knee on the unaffected side so that weight is borne on the affected side. Normally, the pelvis elevates on the raised-knee side. A drop in the pelvis on the raised-knee side suggests weakness of the hip abductors on the straight-knee (affected) side.
- Patrick test or the FABERE sign (flexion-abduction-external rotation-extension) is performed by placing the supine patient’s heel on the contralateral knee. The examiner then pushes the knee and thigh downward to put the hip into external rotation, producing pain in intrinsic hip disease. Pain in the groin on the side with the flexed knee suggests hip pathology, while pain in the contralateral buttock to the flexed knee suggests sacroiliac joint pathology.
- Palpation of the hip joint and surrounding area is done to elicit tenderness.
- ROM should be tested. Normal hip flexion is approximately 120 degrees; normal internal rotation is 30 degrees and external rotation 60 degrees. Hip joint pathology tends to affect internal rotation most.
- Strength of the adductors, abductors, and flexors should be tested. The lumbar spine and the sacroiliac joints should be examined.
- The groin is examined, looking for evidence of an inguinal or femoral hernia.
- Local tenderness over the trochanteric prominence can be demonstrated with trochanteric bursitis, and hip ROM should be unrestricted.
- With AVN, internal and external rotation of the hip is painful and sometimes reduced. The patient often has a limp.
- Examination in meralgia paresthetica usually reveals hypoesthesia or dysesthesia, or both, in the lateral femoral cutaneous nerve distribution. Examination of the hip is normal unless coexistent hip pathology is present.
- Hip fracture classically reveals an externally rotated, abducted, and foreshortened leg. Ecchymosis or hematoma formation may be present at the hip.
- Pulses should be evaluated to rule out vascular claudication or Leriche syndrome (aortoiliac occlusive disease).
Diagnostic Testing
- Plain radiographs, when indicated, should include AP and lateral views of the hip and an AP view of the pelvis.
- CT or MRI is occasionally needed to evaluate the hip further (e.g., occult hip fractures and osteonecrosis).
- Films in AVN may show sclerosis of the femoral head. Collapse of the femoral head is seen in advanced cases. If initial radiographs are normal, an MRI should be considered because of its high sensitivity for this diagnosis.
- Hip fractures are usually obvious, but plain films are occasionally negative. A bone scan, CT scan, or MRI may be necessary for diagnosis.
TREATMENT
- Trochanteric bursitis is slow to respond to therapy but almost never becomes chronic.
- NSAIDs often provide symptomatic relief, and PT for modalities and iliotibial band stretching can be helpful. Patients should be encouraged to continue with stretching exercises at home.
- A corticosteroid injection (30 to 40 mg methylprednisolone) with local anesthetic (3 mL/1% lidocaine) into the greater trochanteric bursa usually brings at least temporary relief.106,107
- NSAIDs often provide symptomatic relief, and PT for modalities and iliotibial band stretching can be helpful. Patients should be encouraged to continue with stretching exercises at home.
- Limited weight bearing with a cane or walker may be sufficient for some patients with AVN, but orthopedic consultation should always be obtained to evaluate the need for surgical core decompression or total hip arthroplasty. If corticosteroid therapy remains necessary, efforts should be made to reduce the dose as much as possible.
- For meralgia paresthetica, treatment consists of eliminating the source of nerve compression or repetitive trauma. Weight loss in obese patients can be effective.
- Treatment of hip fractures is almost always surgical, and an orthopedic consultation is mandatory. A patient with an osteoporotic fracture should have bone density measured by dual x-ray absorptiometry as a baseline and should be started on medications to increase bone density and decrease the risk of subsequent fracture (Chapter 3).
Knee Pain
GENERAL PRINCIPLES
- With normal use, the knee is subject to considerable wear and tear and is vulnerable to injury (often sports related). As such, knee pain is a common complaint. Degenerative disease, trauma, and inflammatory processes are the most frequent causes.
- Osteoarthritis of the knee is an extremely common condition and an important source of disability.
- Important associations include age, wear and tear, obesity, genetic factors, prior trauma (e.g., fractures, ligamentous injuries that cause instability, and meniscal damage), and prior knee surgery. Osteoarthritis may affect any or all of the three compartments of the knee (medial and lateral tibiofemoral and patellofemoral).
- The medial compartment is the most commonly involved.
- The diagnosis and treatment of osteoarthritis are discussed in Chapter 33.
- Important associations include age, wear and tear, obesity, genetic factors, prior trauma (e.g., fractures, ligamentous injuries that cause instability, and meniscal damage), and prior knee surgery. Osteoarthritis may affect any or all of the three compartments of the knee (medial and lateral tibiofemoral and patellofemoral).
- The inflammatory conditions can be divided into noninfectious and infectious causes.
- Noninfectious causes include RA, lupus, psoriatic arthritis, reactive arthritis, gout, and pseudogout.
- The most common infectious causes are gonococcal arthritis (especially in sexually active young adults) and S. aureus. Extra-articular infections, previous damage to the joint, prosthetic joints, serious underlying chronic illness, immunosuppression, corticosteroid therapy, and IV drug use are predisposing factors for septic arthritis.
- The treatment of inflammatory arthropathies is discussed in Chapter 33.
- Noninfectious causes include RA, lupus, psoriatic arthritis, reactive arthritis, gout, and pseudogout.
- Patellofemoral pain syndrome (PFPS) is characterized by retropatellar or peripatellar pain and crepitation with certain activities.
- The condition is ill defined and poorly understood, but nonetheless anterior knee pain of this type is very common and may become chronic and limit activity.
- Multiple associations and predisposing factors have been proposed, including overuse/overloading, maltracking of the patella, patellar subluxation, obesity, malalignment of the knee extensor mechanism, quadriceps weakness, and trauma. Many patients, however, have no such associations.
- The relationship of PFPS to chondromalacia of the patella is controversial. PFPS can occur without chondromalacia, and patients with chondromalacia may have no symptoms.108
- The condition is ill defined and poorly understood, but nonetheless anterior knee pain of this type is very common and may become chronic and limit activity.
- Ligamentous injuries are generally seen after trauma in athletic young adults. These injuries comprise a spectrum from torn and stretched ligamentous fibers to complete tear or rupture. Collateral and cruciate ligament injuries can occur alone or together, with or without meniscal damage.
- Meniscal tears typically occur after a twisting injury, and the medial meniscus is much more commonly affected. This type of injury can occur in isolation or with a medial collateral or anterior cruciate ligament (ACL) tear, or both. Older individuals may experience a degenerative meniscal tear after minimal trauma.
- Bursitis can occur at several locations in the knee. Bursae are lined with synovium and produce a small amount of fluid that decreases friction between adjacent structures. Chronic overuse, trauma, and friction can result in inflammation.
- Prepatellar bursitis is usually caused by repeated trauma involving a lot of kneeling (e.g., housemaid’s knee and clergyman’s knee).
- The pes anserine bursa lies under the insertion of the hamstrings on the proximal medial tibia. It can become inflamed with overuse (e.g., walking or running) and in those with osteoarthritis of the knee.
- Prepatellar bursitis is usually caused by repeated trauma involving a lot of kneeling (e.g., housemaid’s knee and clergyman’s knee).
- Baker cyst (popliteal cyst or semimembranosus-gastrocnemius bursitis) is a fluid-filled sac located in the popliteal fossa, usually on the medial side. It frequently connects with the joint cavity. It is often associated with knee effusions, posterior meniscal tears, and degenerative arthropathy.109 It is also very common in RA.110
- Iliotibial band friction syndrome is a common overuse injury in runners and cyclists. Repetitive movement of a tight iliotibial over the lateral femoral condyle causes friction and pain, particularly with climbing stairs and running down hills.
- Tibial tubercle apophysitis (Osgood-Schlatter disease) generally presents in adolescents, with pain localized to the insertion of the patellar tendon at the tibial tubercle. It is often related to an ossicle of bone within the tibial tendon anterior to the tubercle. Pain usually resolves with time when the ossicle fuses with the underlying bone. Until that time, pain should limit athletic activity.
DIAGNOSIS
Clinical Presentation
History
- Knee disorders usually present with one or more of the following: pain, stiffness, swelling, redness, warmth, tenderness, giving way, locking, and cracking.
- Patients should be carefully asked about exacerbating activities, sports, and prior episodes of trauma. A history of pain in the contralateral knee or other joints, or both, can be important.
- With mechanical causes, pain is typically worsened with activity and improved with rest.
- Acute knee pain is often traumatic, and the mechanism of injury should be detailed. An audible pop is sometimes heard. Subacute and chronic knee discomfort is also common.
- The possibility of septic arthritis (discussed in detail in Chapter 33) should always be considered with acute monoarticular arthritis of the knee.
- Synovitis presents with pain, stiffness, and an effusion. Infection, gout, and pseudogout are the usual causes.
- PFPS patients complain of anterior knee pain with activities such as going down steps or hills, squatting, running, jumping, and prolonged sitting (the theater sign).
- ACL tears are usually caused by a significant twisting injury. A popping sensation may be described. Pain is immediate, quickly followed by the development of a large effusion, giving way, and great difficulty in walking.
- Collateral ligament tears usually follow an abduction or adduction force (medial or lateral collateral ligaments, respectively). These patients complain of pain, stiffness, and localized swelling. Most are able to ambulate after the injury.
- With meniscal injuries, patients usually report pain, swelling, and stiffness after a significant twisting injury. Pain may be referred to the popliteal area. Clicking, locking, or giving way may also be described. Most patients are able to walk after the injury.
- Many Baker cysts are asymptomatic, but swelling, tenderness, and fullness behind the knee may be reported. Very large cysts can cause significant pain and even neurovascular compromise because of the pressure on surrounding structures. Some cysts become symptomatic only when they rupture, producing redness, swelling, warmth, pain, and tenderness of the calf, which can be confused with a deep venous thrombosis.
Physical Examination
- Physical examination of the knee includes inspection, palpation, ROM, strength, and gait. Acute knee inflammation may make adequate examination difficult or impossible. Normal flexion of the knee is 135 degrees, and extension is 0 degrees.
- Inspection should compare the affected knee to the unaffected side. Subtle warmth is best appreciated by comparing side to side with the examiner’s anterior wrist, which is more sensitive than the digits.
- The bulge sign can be used to detect small knee effusions.
- The patient’s knee is extended flat on the examination table.
- Joint fluid is milked up into the suprapatellar pouch by moving the hand proximally along the medial side of the patella.
- The fluid is then milked down into the medial knee by moving the hand from above the lateral side of the patella along the lateral knee and down to the tibia.
- Excessive fluid creates a bulge medial to the patella.
- The patient’s knee is extended flat on the examination table.
- The anterior drawer test and Lachman test are used to test for cruciate ligament instability. Both knees should be tested for comparison.
- The anterior drawer test is performed with the patient supine and the knee flexed to 90 degrees. The tibia is grasped with both hands and pulled anteriorly.
- Lachman test is performed with the supine patient’s knee in 20 degrees of flexion. The distal femur is stabilized with one hand, while the other hand pulls the tibia forward.
- Excessive anterior displacement of the tibia and a less than sharp end point suggest ACL damage.
- Lachman test is generally believed to be the more sensitive test, but the combination of both tests may be better still.111,112
- The anterior drawer test is performed with the patient supine and the knee flexed to 90 degrees. The tibia is grasped with both hands and pulled anteriorly.
- Stability of the collateral ligaments should be tested in 20 to 30 degrees of flexion and full extension. One hand stabilizes the lateral side of the knee, while the other hand applies abduction force to the distal leg, or one hand stabilizes the medial side of the knee, while the other hand applies adduction force to the distal leg. Excessive motion, usually with pain, signifies medial or collateral ligament damage.
- McMurray test can be used to detect meniscal tears. With the supine patient’s knee in full flexion, the knee is slowly extended as the tibia is rotated internally and externally. A palpable or audible pop, often with pain, suggests a meniscal tear. This test is insensitive but fairly specific.112 Combining McMurray test with joint line tenderness may improve diagnostic ability.111,113
- The examination with osteoarthritis often reveals tenderness along the joint line, a small effusion, crepitus during knee motion, and sometimes palpable osteophytes. Patients with significant medial compartment disease often have a varus (bowleg) deformity when standing. Less commonly, a valgus (knock-knee) deformity may occur with lateral compartment disease.
- With PFPS, crepitus and malalignment of the patella with flexion and extension (patella tracks too far laterally) can sometimes be appreciated. Some quadriceps atrophy may also be present. A knee effusion is infrequently seen. The patellar compression test supports the diagnosis. The examiner immobilizes the patella while the patient contracts the quadriceps muscle, pulling the patella proximally against the femoral condyles, reproducing the pain.
- The prepatellar bursa lies between the skin and the patella. It produces swelling directly above the patella. There may also be redness and warmth, suggesting an infectious process.
- With pes anserine bursitis, pain occurs on the anteromedial aspect of the knee, and the area is exquisitely tender.
- A Baker cyst may be appreciated as a prominence in the medial aspect of the popliteal fossa. In the situation of a ruptured cyst, inflammation of the calf occurs, potentially simulating thrombophlebitis.
Diagnostic Testing
- All new knee effusions that are warm and painful should be tapped. Removal of the synovial fluid is necessary to rule out a septic joint, gout, or pseudogout.
- Plain radiographs of the knee are frequently done as a part of the evaluation of knee pain, but they are not always necessary.
- If the history and physical examination suggest a periarticular problem, plain films are unlikely to be diagnostic and are generally unnecessary. When a significant mechanical articular problem is suggested by the history and physical examination, plain films may be helpful. The Ottawa knee rules can be used to determine, which patients with acute knee injuries require knee films (Table 34-5).112,114
- Standard films include AP and lateral views, and standing films should be obtained if possible.
- Detection of some fractures by plain radiography may require special views.
- With PFPS, radiographs of the patella (Merchant view) may show malalignment of the patella but are usually normal.
- Plain films cannot diagnose ligamentous or meniscal damage but can detect avulsion fractures.
- MRI detects meniscal tears but false positives can occur.
- Ultrasound can be used to visualize a Baker cyst and evaluate for thrombophlebitis of the leg. MRI can also be used to visualize a Baker cyst.
TABLE 34-5 Ottawa Knee Rules
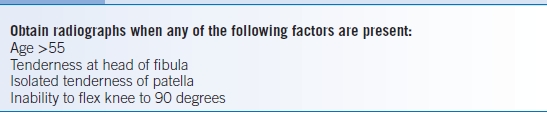
Data from Stiell IG, Wells GA, Hoag RH, et al. Implementation of the Ottawa Knee Rule for the use of radiography in acute knee injuries. JAMA 1997;278:2075–2079.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


