Mucinous Cystic Neoplasms
Scott R. Owens, MD
Key Facts
Terminology
Mucinous cystic neoplasm
Circumferential proliferation of low-grade or high-grade dysplastic, mucin-producing epithelium that may distend appendix and fill it with mucin
Pseudomyxoma peritonei
Clinical term referring to neoplastic process that fills abdomen with extracellular mucin
Mucinous adenocarcinoma is appropriate diagnosis when lesion is clearly invasive
Clinical Issues
Simple appendectomy with negative margins is probably sufficient for tumors confined to appendix
Truly invasive adenocarcinomas require regional resection with lymphadenectomy (right hemicolectomy)
Prognosis tied predominantly to cytological grade of neoplasm
Macroscopic Features
Evidence of rupture must be carefully sought
Thorough sampling of abdominal tissues in PMP is crucial to adequately search for neoplastic epithelium
Microscopic Pathology
So-called epithelial displacement vs. true mural invasion is root of much controversy
Diagnostic Checklist
Ovarian involvement common in women, leading to previous belief that pseudomyxoma peritonei often originated in primary ovarian tumors
TERMINOLOGY
Abbreviations
Mucinous cystic neoplasm (MCN)
Pseudomyxoma peritonei (PMP)
Synonyms
Appendiceal mucocele
Mucinous cystadenoma (MCA)
Mucinous tumor of uncertain malignant potential
Mucinous tumor of low malignant potential
Borderline tumor of appendix
Low-grade appendiceal mucinous neoplasm (LAMN)
Definitions
Mucinous cystic neoplasm
Proliferation of low- or high-grade, dysplastic, mucin-producing epithelium that may distend appendix and fill it with mucin
Mucocele results when mucin production distends appendix into spherical or sausage-shaped mass
Mucinous cystadenoma
Refers generally to low-grade dysplastic epithelial proliferations confined to appendix
Pseudomyxoma peritonei
Clinical term referring to neoplastic process that fills abdomen with extracellular mucin
Often associated with appendiceal mucinous tumors
Classification of primary appendiceal tumor particularly controversial in this setting
Confusing terminology
Disseminated peritoneal adenomucinosis (DPAM), LAMN, borderline tumor, mucinous tumor of uncertain/low malignant potential
Reflects longstanding controversies regarding spread of acellular or cellular mucin outside appendix without clear-cut invasive carcinoma
Some advocate use of “adenocarcinoma” for any tumor with extraappendiceal spread of mucinous cells
Others suggest possibility of noncarcinomatous spread of mucin-producing cells after appendiceal rupture
Mucinous adenocarcinoma is appropriate diagnosis when lesion is clearly invasive
ETIOLOGY/PATHOGENESIS
Molecular Abnormalities
KRAS mutations in around 70%
Loss of heterozygosity (LOH) of chromosome 5q (including locus linked to APC gene) in up to approximately 20%
CLINICAL ISSUES
Epidemiology
Incidence
Low-grade MCN relatively uncommon (˜ 1 per 100,000 per year)
Pseudomyxoma peritonei even rarer (˜ 0.1 per 100,000 per year)
Primary appendiceal adenocarcinoma (˜ 0.2 per 100,000 per year in North America)
Age
Occur in adults of any age, but 3rd to 8th decade most common
Gender
Occur in both males and females, with female predominance
Presentation
Asymptomatic/incidental
Deep mass
Possible with larger tumors
Abdominal pain
Possible in abdominal dissemination/PMP
Treatment
Options, risks, complications
Simple appendectomy with negative margins probably sufficient for tumors confined to appendix
Truly invasive adenocarcinomas require regional resection with lymphadenectomy (right hemicolectomy)
Surgical approaches
Not standardized for low-grade tumors with peritoneal spread
Some advocate aggressive approach to tumors that have breached appendix with resultant PMP
Omentectomy, splenectomy, peritoneal stripping (“peritonectomy”), cholecystectomy, antrectomy, sigmoid colectomy
Intraoperative hyperthermic chemotherapy to treat unresected tumor cells
Disseminated high-grade tumor/carcinomatosis may not be amenable to aggressive therapy
Adjuvant therapy
Additional cycles of intraperitoneal ± systemic chemotherapy may follow aggressive resection
Prognosis
Good for lesions confined to appendix and completely resected
Outcomes data hampered in extraappendiceal spread by varying diagnostic labels used in different studies
Appears to be tied predominantly to cytological grade of neoplasm
Low-grade extraappendiceal neoplasm has better prognosis than high-grade/frank carcinomatosis
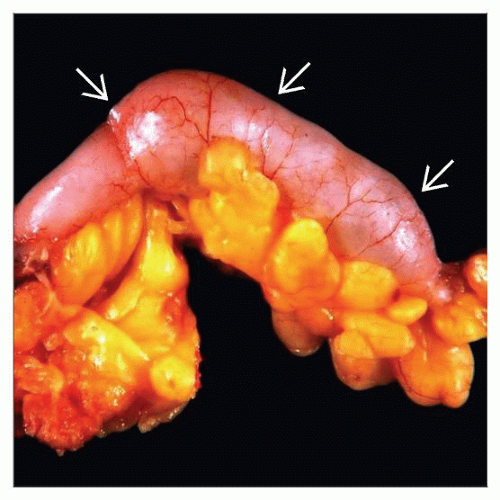
MACROSCOPIC FEATURES
General Features
Dilated mucin-filled appendix
Evidence of rupture must be carefully sought
Sections to Be Submitted
Entire appendix should be submitted when mucinous lesion is seen grossly
Incidental mucinous lesions found after routine appendiceal sampling should prompt complete submission
Thorough sampling of abdominal tissues in PMP is crucial to adequately search for neoplastic epithelium
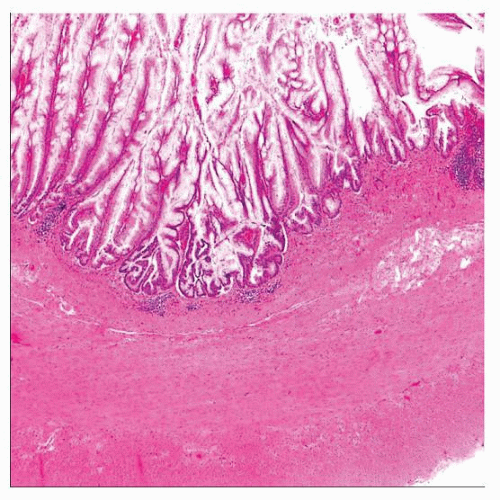
MICROSCOPIC PATHOLOGY
Key Descriptors
Predominant pattern/injury type
Neoplastic
Predominant cell/compartment type
Epithelial, mucinous
Histologic features
Most often have somewhat different morphology than typical colorectal adenomas
Elongated cells with “tall” thin mucin vacuoles and basal nuclei
Dysplastic epithelium may be flattened or have an undulating pattern surrounding luminal mucin
Lesions with serrated architecture resembling serrated polyps of colorectum are possible
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree