Motility Disorders
Scott R. Owens, MD
Key Facts
Macroscopic Features
Sampling of both dilated and normal-appearing areas important
Affected organ(s) may be massively dilated
Megacolon, megaesophagus, megajejunum, etc.
Mucosal stercoral ulcers possible in chronic constipation
Microscopic Pathology
Infiltrative processes must be excluded
Amyloidosis
Fibrosis
Histological changes often subtle (or absent)
Number of ICCs reportedly decreased in chronic (slow-transit) constipation patients
CD117 (c-kit) immunostain highlights ICC
Diagnostic Checklist
Scleroderma preferentially involves fibrosis of inner (circular) smooth muscle
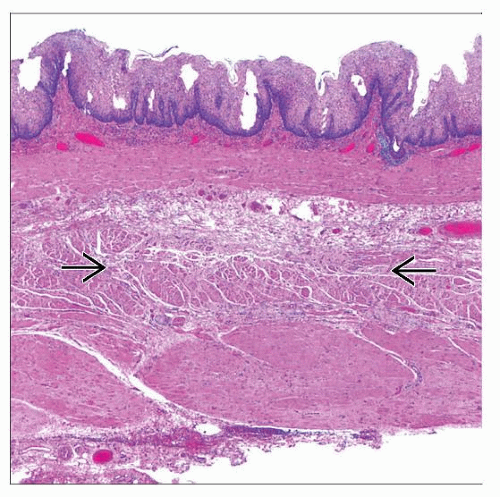
 Gross photograph shows massively dilated colon (“megacolon”) resected from a patient with chronic constipation. The colon was approximately 20 cm in diameter. |
TERMINOLOGY
Definitions
Primary motility disorder: No associated systemic disease
Visceral myopathies (familial or sporadic)
Visceral neuropathies (familial or sporadic)
Chronic (slow-transit) constipation
Secondary motility disorder: Associated with systemic illness
Diabetes mellitus
Scleroderma (systemic sclerosis)
Amyloidosis
ETIOLOGY/PATHOGENESIS
Neuromuscular Dysfunction
Complex gut physiology normally involves myriad neuromuscular interactions
Extrinsic factors
Sympathetic and parasympathetic nervous system
Intrinsic factors
Enteric nerve plexuses
Smooth muscle layers: Inner is circular and outer is longitudinal
Interstitial cells of Cajal (ICC): Intermediary cells between nerve plexus and smooth muscle
Malfunction/injury of any component → possible impact on motility
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree