Mixed Cryoglobulinemic Glomerulonephritis
A. Brad Farris, III, MD
Key Facts
Terminology
GN due to immunoglobulins soluble at 37°C, reversibly precipitate with cooling
Etiology/Pathogenesis
Renal disease usually type II mixed cryoglobulinemia & not type I or III
Hepatitis C virus (HCV) comprises ≥ 30% of mixed cryoglobulinemias
Clinical Issues
Proteinuria &/or hematuria
Cryoglobulin serum precipitate, typically IgG and IgMκ
“Essential mixed cryoglobulinemia syndrome” of vasculitis with cutaneous purpura, urticaria, weakness, & arthralgias
Microscopic Pathology
Glomerular mesangial and capillary hypercellularity
Glomerular basement membrane duplication
Eosinophilic, refractile PAS(+) hyaline deposits fill capillary lumina
Ancillary Tests
IgG, IgM, and C3 seen most often on IF
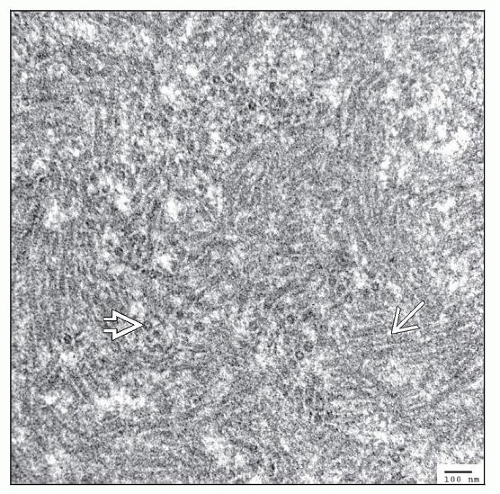
Microtubules, rings, and annular structures on EM
Many glomerular monocytes/macrophages may be CD68(+)
Top Differential Diagnoses
Lupus nephritis, idiopathic MPGN, other GNs
Immunotactoid glomerulopathy
Thrombotic microangiopathy (TMA)
TERMINOLOGY
Abbreviations
Cryoglobulinemic glomerulonephritis (CryoGN)
Synonyms
Cryoglobulinemic GN
Membranoproliferative GN
Essential mixed cryoglobulinemic GN
Definitions
GN due to specific proteins (immunoglobulins) that are soluble at 37°C and reversibly precipitate at cold temperatures
Originally described by Meltzer, Franklin, McCluskey, and colleagues (1966)
ETIOLOGY/PATHOGENESIS
Infectious Agents
Hepatitis C virus (HCV) comprises ≥ 30% of mixed cryoglobulinemias
It was once unknown that HCV caused these cases, & these cases were once termed “essential mixed cryoglobulinemias”
Type II Mixed Cryoglobulinemia
Renal disease typically occurs with type II mixed cryoglobulinemia & not usually with type I or III
Monoclonal component is almost always IgM with kappa light chain (IgMκ)
CLINICAL ISSUES
Presentation
“Essential mixed cryoglobulinemia syndrome”
Systemic vasculitis with cutaneous purpura, urticaria, weakness, & arthralgias
Biopsy shows leukocytoclastic vasculitis
10-60% of cases have renal disease
Proteinuria
1/5 have nephrotic-range proteinuria or nephrotic syndrome
Hematuria
Some have microscopic hematuria
˜ 25% of patients have acute nephritic syndrome with hypertension, increased serum creatinine, proteinuria, and macroscopic hematuria
< 5% of patients develop oliguric or anuric renal failure
Renal dysfunction
Mild renal insufficiency may be present, but serum creatinine is typically normal
Hypertension
Commonly occurs & may be rather severe
Splenomegaly
Laboratory Tests
Cryoglobulin precipitate, typically IgG and IgMκ, detectable as a “cryocrit” or percent of serum composed of precipitate
Best detected when blood specimen is maintained at 37°C until clotting is completed
C4 (early complement component) low and C3 normal or slightly decreased
Serum antibodies against HCV or HCV RNA in most patients
Treatment
Surgical approaches
Renal transplantation uncommonly performed because of usual indolent nature
May recur in transplant
Adjuvant therapy
Plasmapheresis for relief of acute exacerbation of renal disease
Cryofiltration, whereby patient’s plasma is cooled, precipitating out cryoglobulins, and then rewarmed and reinfused
Drugs
Corticosteroids
Aggressive immunosuppressive therapy (pulse methylprednisolone followed by oral steroids and cyclophosphamide) only used with caution to prevent hepatitis C reactivation; typically only used in patients with severe acute vasculitis and multisystem manifestations
Cytotoxic immunosuppressive drugs
Cyclophosphamide (Cytoxan)
Interferon-α
Used to treat hepatitis C virus-associated cryoglobulinemia
Ribavirin
Rituximab
Prognosis
Typically more indolent than idiopathic MPGN
Progression to ESRD uncommon, occurring in around 10% of cases (usually in 5-10 years)
Death may result from infections, cardiovascular disease, and systemic effects of vasculitis
MICROSCOPIC PATHOLOGY
Histologic Features
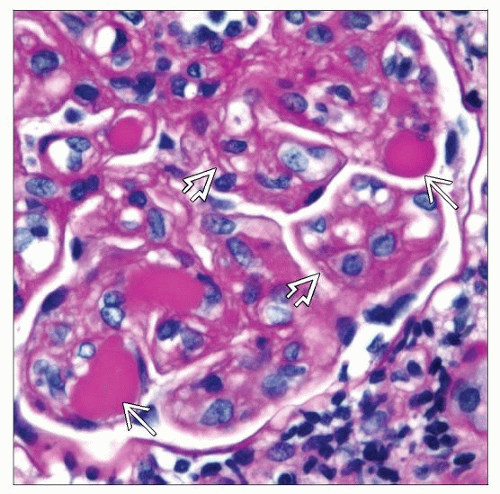
Glomeruli
Diffuse intracapillary hypercellularity with glomerular capillary loop occlusion
Leukocytes, particularly monocytes, compose the hypercellularity
Eosinophilic, refractile-appearing PAS(+) hyaline deposits fill capillary lumina
Known as “intraluminal thrombi” or perhaps more properly “pseudothrombi” since they are not actually composed of fibrin
Also called PAS(+) coagulum by some pathologists
Glomerular basement membrane (GBM) diffusely thickened, appreciated most readily on PAS or Jones stain
Reduplication or “tram tracking” of GBM
Crescents (also known as extracapillary proliferation)
Mild or marked mesangial proliferation associated with cases having heavy proteinuria and renal failure
Tubulointerstitium
Interstitial fibrosis and tubular atrophy is usually mild/localized
Erythrocyte casts in tubular lumina, particularly during acute episodes
Vessels
Vasculitis of small- and medium-sized arteries and arterioles (20-25% of cases)
Intimal and medial fibrinoid necrosis
Intraluminal glassy or refractile deposits in arterioles as they are in glomerular capillary loops
Intimal fibrosis eventually replaces areas of fibrinoid necrosis
ANCILLARY TESTS
Immunohistochemistry
CD68 (KP-1) may stain numerous KP-1-positive monocyte/macrophages (also positive for esterase)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree